Understanding the Relationship Between Weight and Diabetes
Diabetes, particularly type 2 diabetes, has long been associated with excess body weight and metabolic imbalance. As the global obesity epidemic continues to escalate, so too does the prevalence of type 2 diabetes, prompting both the medical community and the public to explore whether losing weight can offer a path to reversal. This question, while simple on the surface, leads into a nuanced and evolving area of scientific inquiry. The terms “reversal,” “remission,” and “cure” carry different clinical implications, and it is important to distinguish among them to understand what is realistically achievable through weight loss.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
Scientific studies have consistently shown that adiposity, especially visceral fat stored around the organs, contributes to insulin resistance—the hallmark of type 2 diabetes. This resistance forces the pancreas to produce more insulin to maintain glucose balance, which eventually leads to beta-cell exhaustion. Given this, the logical inquiry follows: can losing weight cure diabetes, or at the very least, improve blood glucose control significantly enough to eliminate the need for medications? Researchers are increasingly exploring how lifestyle interventions, particularly weight loss, can impact the trajectory of the disease. The answers emerging from clinical trials and real-world case studies are both promising and complex.
What Does Diabetes Remission Really Mean?
To understand whether diabetes can be cured with weight loss, it’s essential first to define the concept of remission. In medical terms, remission refers to a period during which the signs and symptoms of a disease are reduced or disappear entirely without active pharmacological treatment. For type 2 diabetes, this typically means achieving and maintaining blood glucose levels below the diabetic threshold—often defined as an HbA1c under 6.5%—without the aid of diabetes medications for at least three to six months.
However, remission is not the same as a cure. Unlike a cure, which implies permanent elimination of disease, remission acknowledges the possibility of recurrence. This distinction is critical when discussing whether losing weight can truly “cure” diabetes or if it merely pushes it into a dormant state. While the idea that you can lose diabetes by losing weight may appeal to many, the reality is more complex and requires a sustained, multi-pronged approach.
Researchers stress that remission should not be viewed as a guarantee but rather as a favorable and achievable clinical goal. Weight loss plays a key role in this process, but the success of remission also depends on individual metabolic profiles, duration of diabetes, and adherence to long-term lifestyle changes. This nuanced understanding underscores the need for clear communication and realistic expectations when considering weight loss as a strategy for diabetes management.

Clinical Evidence: Can You Lose Diabetes by Losing Weight?
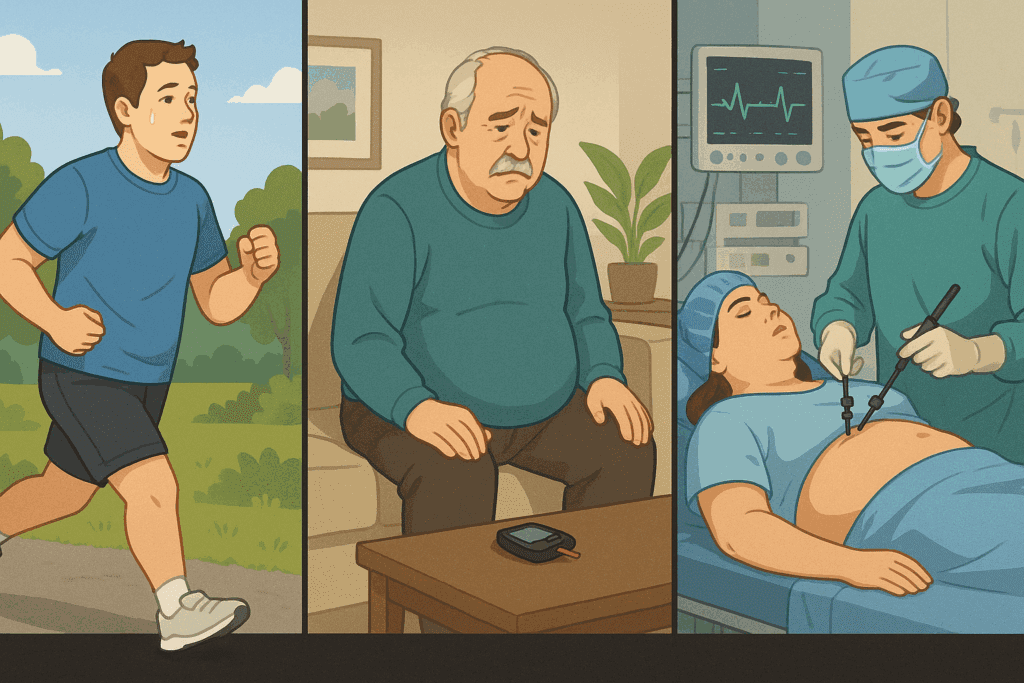
The idea that you can lose diabetes by losing weight is supported by a growing body of clinical evidence. One of the most influential studies in this area is the DiRECT (Diabetes Remission Clinical Trial) study conducted in the United Kingdom. This randomized controlled trial involved adults with type 2 diabetes who followed a structured, low-calorie diet for several months, followed by a gradual food reintroduction phase and long-term support. The results were striking: nearly half of the participants achieved remission at one year, and many maintained it at the two-year follow-up.
The DiRECT study demonstrated that significant weight loss—often around 10 to 15 kilograms (22 to 33 pounds)—could normalize blood glucose levels without medication. Participants who lost more than 15 kilograms were especially likely to experience remission. These findings were groundbreaking because they showed that diabetes is not always a lifelong condition and that, in some cases, its progression can be halted or even reversed through lifestyle changes alone.
However, the success of such interventions also depends on the duration of diabetes. Those diagnosed more recently tend to respond more favorably to weight loss interventions than those who have lived with the disease for many years. This is likely because prolonged hyperglycemia damages pancreatic beta cells over time, reducing their capacity to recover even if insulin resistance improves. Therefore, while the answer to the question “does losing weight cure diabetes” may be a tentative yes for some, the window of opportunity is narrower for others depending on the stage of disease progression.
How Weight Loss Improves Insulin Sensitivity and Glucose Control
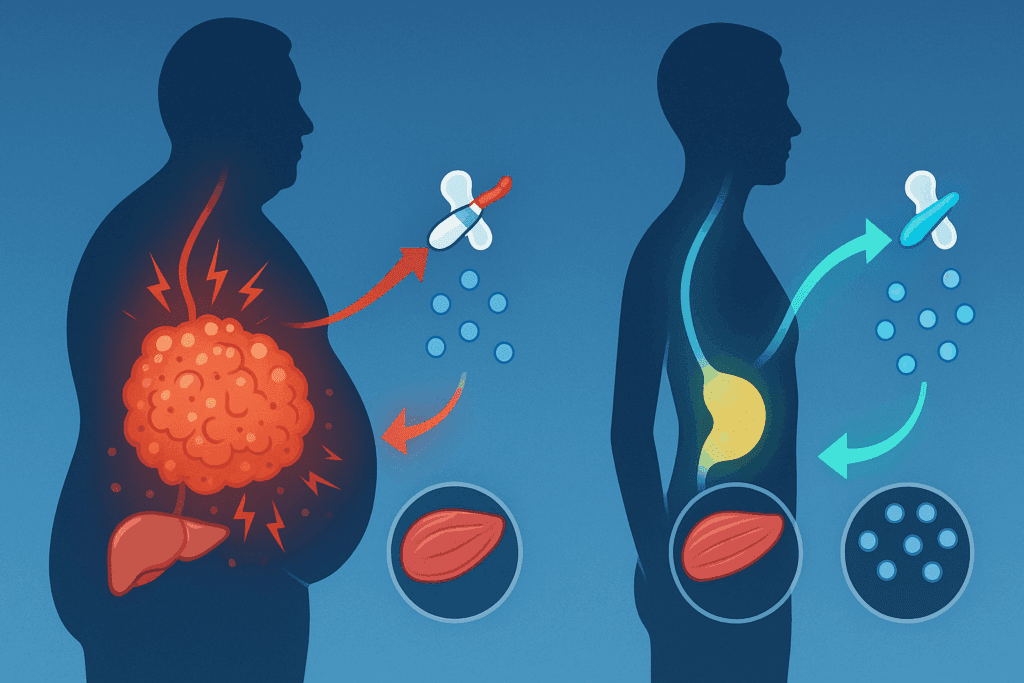
To grasp why weight loss has such a profound impact on type 2 diabetes, it’s important to understand its physiological effects on insulin sensitivity and glucose metabolism. Fat tissue, especially in the abdominal region, is not merely a passive storage site but an active endocrine organ. It secretes hormones and inflammatory cytokines that interfere with insulin signaling, thereby promoting insulin resistance.
When a person loses weight, particularly visceral fat, these pro-inflammatory signals decrease, improving the body’s response to insulin. As a result, glucose is more efficiently transported into cells, reducing the need for the pancreas to produce excessive insulin. This improvement in metabolic function can lead to lower fasting glucose levels, reduced HbA1c, and overall better glycemic control—all without the need for medications.
In addition, weight loss can reduce liver fat content, which is another key factor in insulin resistance. The liver plays a central role in regulating blood sugar, and excess liver fat is associated with increased glucose production and impaired insulin clearance. By decreasing liver fat, weight loss further supports the restoration of normal glucose regulation. This cascade of physiological improvements helps explain why, in many cases, diabetes can be reversed with weight loss—especially when the intervention is implemented early and sustained over time.
Does Losing Weight Cure Diabetes for Everyone? Factors That Influence Outcomes
While many people experience significant benefits from weight loss, it’s important to acknowledge that not all individuals will achieve remission. Several factors influence whether losing weight will reverse diabetes, including genetics, the duration of diabetes, beta-cell function, and underlying metabolic health. People with a longer history of diabetes may have sustained irreversible damage to their insulin-producing cells, limiting their capacity for recovery.
Moreover, the extent and method of weight loss also matter. Gradual, sustainable weight loss through a combination of calorie restriction, increased physical activity, and behavioral therapy tends to produce better long-term outcomes than rapid or extreme methods. Bariatric surgery, which results in substantial weight reduction, has also shown high rates of diabetes remission, but it comes with surgical risks and lifestyle adjustments that may not be suitable for everyone.
It is also worth considering the role of muscle mass, sleep quality, stress levels, and even gut microbiota in influencing diabetes outcomes. A holistic approach that includes diet, exercise, stress reduction, and sleep optimization is more likely to succeed than focusing on weight loss alone. While the idea that losing weight can cure diabetes holds merit for many, it must be framed within the broader context of personalized medicine and whole-body health.
The Psychological Dimension: Motivation, Adherence, and Sustainable Change
Sustaining weight loss and achieving diabetes remission is not just a matter of willpower; it involves complex psychological and behavioral factors. Individuals diagnosed with type 2 diabetes often face emotional challenges, including stress, depression, and anxiety, which can impede their ability to maintain lifestyle changes. Understanding these psychological barriers is critical for designing effective interventions.
Motivation plays a pivotal role in initiating weight loss, but long-term adherence depends on support systems, habit formation, and the ability to navigate setbacks. Studies have shown that individuals who receive structured support—whether through counseling, peer groups, or digital platforms—are more likely to maintain weight loss and improve glycemic control. Behavioral therapies, including cognitive-behavioral therapy (CBT), have proven effective in helping patients identify triggers, set realistic goals, and stay engaged with their health plans.
Another important element is the framing of success. Instead of viewing diabetes management as an all-or-nothing endeavor, framing it as a journey toward improved health can help patients stay motivated even if remission is not achieved. For many, the question is not only “will losing weight cure diabetes” but also “how can I improve my quality of life and health outcomes, regardless of the end result?” This mindset fosters resilience, which is essential for sustained change.
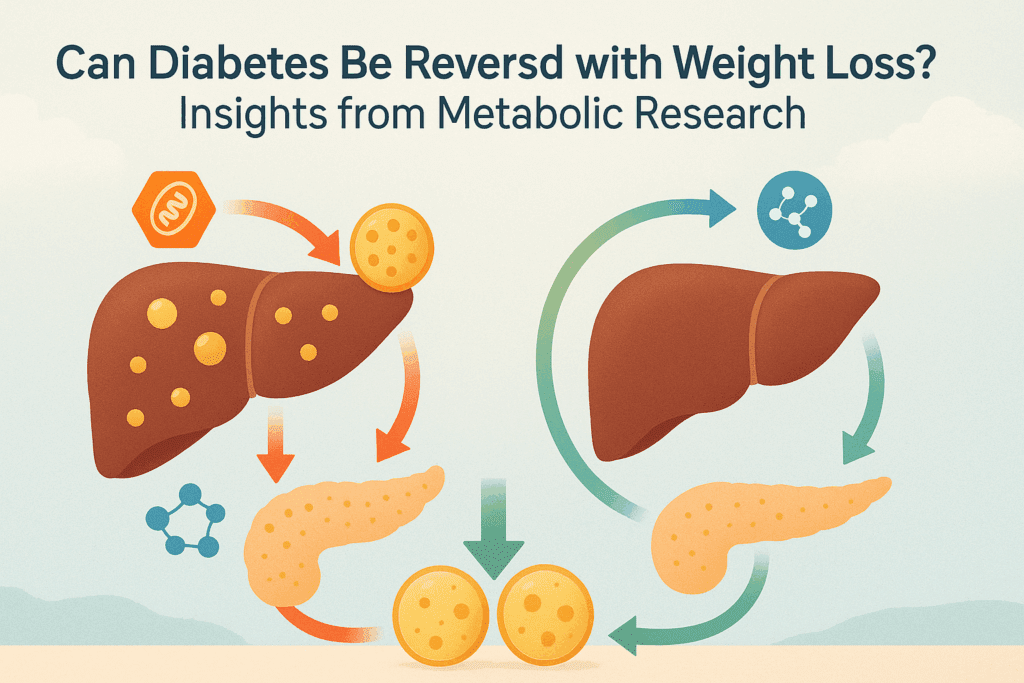
Can Diabetes Be Reversed with Weight Loss? Insights from Metabolic Research
A growing field of metabolic research continues to explore whether diabetes can be reversed with weight loss and, if so, under what circumstances. Animal models and human trials alike suggest that calorie restriction and fat loss can trigger a cascade of beneficial metabolic changes that restore glucose homeostasis. Emerging studies have even begun to identify molecular pathways that mediate these effects, such as changes in mitochondrial function, oxidative stress, and cellular inflammation.
For example, researchers have observed that reducing intra-organ fat, particularly in the pancreas and liver, plays a pivotal role in restoring insulin secretion and sensitivity. This insight aligns with the twin-cycle hypothesis, which posits that excess fat in these organs initiates and perpetuates the cycle of insulin resistance and hyperglycemia. By targeting weight loss to reduce organ fat, it may be possible to reverse the metabolic dysfunctions that define type 2 diabetes.
These findings underscore the importance of early intervention. Individuals who act quickly after diagnosis are more likely to reverse diabetes than those who delay treatment. This is especially true for those who incorporate exercise, nutritional therapy, and behavior modification in a comprehensive, personalized approach. While we still have much to learn, the evidence suggests that for many people, diabetes is not an irreversible condition but a manageable—and in some cases, reversible—metabolic state.
Long-Term Outcomes: Maintaining Remission and Preventing Relapse
Achieving remission is a significant milestone, but maintaining it is an ongoing challenge. Long-term studies have shown that some individuals who enter remission eventually relapse, particularly if they regain weight or revert to unhealthy habits. This highlights the need for continued monitoring, support, and lifestyle reinforcement even after initial success.
Long-term maintenance involves developing sustainable eating patterns, regular physical activity, stress management, and ongoing medical supervision. Tools such as continuous glucose monitoring (CGM) and digital health apps can help individuals track their progress and stay engaged with their health goals. Medical teams also play a critical role in providing follow-up care, adjusting treatment plans, and offering psychological support when needed.
Importantly, even those who do not achieve full remission often experience substantial health improvements through weight loss. These include better blood pressure control, improved lipid profiles, reduced risk of cardiovascular disease, and enhanced quality of life. Thus, the pursuit of weight loss should not be viewed solely through the lens of diabetes remission but as part of a broader strategy for lifelong metabolic health.
Frequently Asked Questions: Can Losing Weight Cure Diabetes?
1. If someone loses a large amount of weight, will their diabetes always go into remission?
While significant weight loss can dramatically improve blood glucose levels, it doesn’t guarantee remission for everyone. Factors like the length of time a person has had diabetes, the degree of pancreatic beta-cell damage, and genetic predispositions all influence outcomes. In some individuals, weight loss may lower insulin resistance but not restore full insulin production. So while it is true that losing weight significantly increases the chances of remission, it would be misleading to assume that remission is guaranteed in all cases. Therefore, the question “can losing weight cure diabetes” depends largely on individual physiology and disease progression.
2. How long does diabetes remission last after weight loss?
Diabetes remission achieved through weight loss can last several years, but its duration varies significantly among individuals. Those who continue to maintain a healthy weight, engage in physical activity, and avoid processed foods often maintain remission longer. However, if weight is regained or lifestyle changes are not sustained, blood glucose levels may rise again. This demonstrates that even if you can lose diabetes by losing weight, long-term vigilance is essential. Remission is a dynamic state, not a permanent fix, underscoring the importance of ongoing lifestyle management.
3. Are there any signs that indicate weight loss is improving diabetes before lab tests confirm it?
Yes, there are early signs that may suggest improvements before lab results reflect major changes. These can include reduced thirst, fewer episodes of fatigue, and improved mood or energy. Some people also notice less frequent urination and better sleep quality. However, these symptoms are not conclusive proof of reversal. While these indicators may support the idea that you can lose diabetes by losing weight, only proper diagnostic testing can confirm a state of remission.
4. Does the type of diet used for weight loss influence diabetes remission success?
Absolutely, not all diets have the same effect on diabetes. Research shows that low-calorie and low-carbohydrate diets are particularly effective in reducing insulin resistance and promoting fat loss in organs like the liver and pancreas. Mediterranean and plant-based diets may also be beneficial due to their anti-inflammatory properties. Diet quality impacts not just weight loss but also hormonal and metabolic regulation. So when asking if diabetes can be reversed with weight loss, it’s crucial to consider how the weight is lost, not just how much is lost.
5. Can weight loss benefit people with type 1 diabetes, or is this relevant only for type 2?
While remission is not applicable to type 1 diabetes—since it’s an autoimmune condition that destroys insulin-producing cells—weight loss can still offer significant benefits. For people with type 1 diabetes who are overweight, reducing body fat can improve insulin sensitivity, which helps with glycemic control. This may lower insulin requirements and enhance overall metabolic function. So although the question “can losing weight cure diabetes” doesn’t apply to type 1 in the same way, weight loss remains an important tool for health management. Improved cardiovascular markers and energy balance are notable side effects of healthy weight reduction in this population.
6. What role does muscle mass play in diabetes remission through weight loss?
Muscle tissue plays a key role in glucose metabolism because it is one of the primary sites for insulin-stimulated glucose uptake. When people lose weight through resistance training or combine aerobic activity with strength-building exercises, they not only reduce fat but also improve insulin sensitivity by increasing muscle mass. This dual action enhances the possibility of remission. Therefore, people wondering if diabetes can be reversed with weight loss should also consider how muscle preservation or growth enhances their odds. A weight loss strategy that includes muscle building is more metabolically advantageous than one that focuses solely on calorie restriction.
7. What psychological strategies help sustain diabetes remission after weight loss?
Psychological resilience, cognitive reframing, and long-term goal setting are crucial for sustaining remission. Many people who ask “will losing weight cure diabetes” are focused on the endpoint, but maintaining behavioral change requires a shift in mindset. Daily habits, stress management techniques like mindfulness, and identity transformation—from someone managing illness to someone pursuing optimal health—can make a profound difference. Support groups, accountability partners, and behavioral therapy also help reinforce healthy behaviors. The journey doesn’t end with weight loss—it continues with the psychological work of sustaining change.
8. Is bariatric surgery a better option for achieving remission compared to lifestyle-based weight loss?
Bariatric surgery often results in rapid and substantial weight loss, with higher remission rates in many studies compared to lifestyle interventions alone. It alters gut hormones that affect appetite, satiety, and insulin sensitivity, sometimes leading to remission even before significant weight loss occurs. However, surgery carries risks and lifelong implications for nutritional intake, which must be weighed carefully. For some, the question isn’t just “does losing weight cure diabetes” but whether surgical or non-surgical routes provide safer, more sustainable outcomes. Ultimately, personalized care based on medical history and preferences should guide this decision.
9. How early in the course of diabetes should weight loss be pursued for the best chance of remission?
Timing is a crucial factor. Individuals diagnosed within the past six years are more likely to achieve remission through weight loss, according to longitudinal studies. The earlier weight loss interventions begin, the less damage occurs to insulin-producing beta cells, making functional recovery more plausible. For those who ask whether you can lose diabetes by losing weight, the answer is far more favorable if lifestyle changes begin soon after diagnosis. Proactive management early on can reduce complications and potentially eliminate the need for long-term medication.
10. What are emerging technologies that support weight loss and diabetes reversal?
New technologies such as continuous glucose monitors (CGMs), digital health apps, and AI-powered nutrition coaches are transforming diabetes care. These tools provide real-time feedback, allowing individuals to make informed dietary and activity-related decisions. Some programs use machine learning to tailor interventions based on individual response patterns. As we explore whether diabetes can be reversed with weight loss, these innovations offer precision tools that can optimize efforts. While traditional lifestyle changes remain foundational, technology now plays an increasing role in facilitating sustainable, personalized outcomes.
Conclusion: Does Losing Weight Cure Diabetes or Simply Transform It?
Asking “does losing weight cure diabetes” is both a clinical and philosophical inquiry. The latest research shows that in many cases, type 2 diabetes can be pushed into remission through sustained weight loss and lifestyle intervention, especially when initiated early in the disease’s course. However, labeling this a “cure” may oversimplify a condition that remains dynamic and responsive to numerous factors, both biological and behavioral.
Weight loss clearly plays a transformative role in managing and potentially reversing type 2 diabetes, particularly when accompanied by comprehensive lifestyle changes. For many individuals, the answer to whether diabetes can be reversed with weight loss is a resounding yes—albeit with caveats regarding maintenance and individual variability. The idea that you can lose diabetes by losing weight is not merely anecdotal; it is increasingly backed by rigorous science and real-world results.
Ultimately, the conversation around diabetes should shift from one of inevitability to one of possibility. With the right tools, support systems, and medical guidance, individuals can reclaim control over their metabolic health. Whether or not this constitutes a cure, the impact on long-term outcomes is profound—and it starts with the empowered decision to pursue sustainable, health-focused weight loss.
Further Reading:
Losing weight can reverse type 2 diabetes, but is rarely achieved or recorded
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.