Understanding Clogged Arteries and Cholesterol Levels
The relationship between cholesterol levels and arterial health has long been a subject of medical research and debate. Conventional wisdom suggests that high cholesterol is a primary driver of atherosclerosis, the condition characterized by the buildup of plaques in the arteries. However, many individuals with normal or even low cholesterol levels also develop clogged arteries, leading to serious cardiovascular complications. This paradox challenges the traditional view and necessitates a deeper exploration of other contributing factors beyond cholesterol alone.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
Cholesterol plays a crucial role in the body’s normal functions, including the formation of cell membranes and the production of essential hormones. However, excessive cholesterol, particularly low-density lipoprotein (LDL), is commonly associated with arterial plaque formation. Still, emerging research suggests that inflammation, oxidative stress, genetics, and lifestyle choices are equally significant in the development of arterial blockages, even in individuals with cholesterol levels considered within the normal range.
To fully grasp how clogged arteries can develop without elevated cholesterol, it is essential to analyze the mechanisms behind plaque formation, the influence of other risk factors, and the warning signs that indicate arterial disease. By understanding these elements, individuals can take proactive steps toward cardiovascular health, regardless of their cholesterol levels.
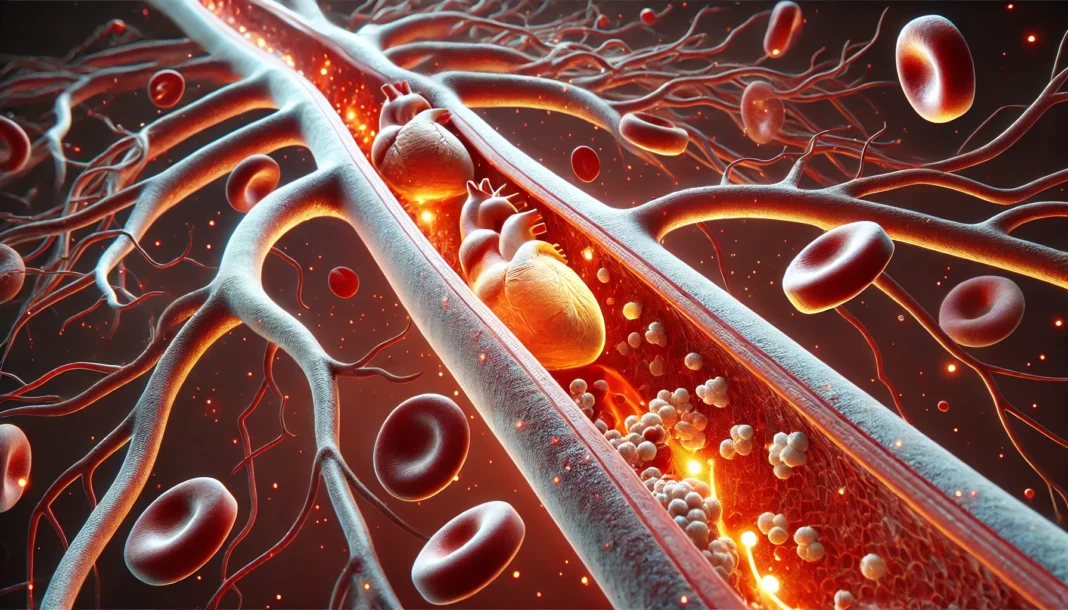
How Do Arteries Become Clogged?
Arteries are blood vessels responsible for delivering oxygen-rich blood throughout the body. When these arteries become clogged, blood flow is restricted, potentially leading to life-threatening conditions such as heart attacks and strokes. This process, known as atherosclerosis, typically results from the accumulation of fatty deposits, calcium, and inflammatory cells within the arterial walls.
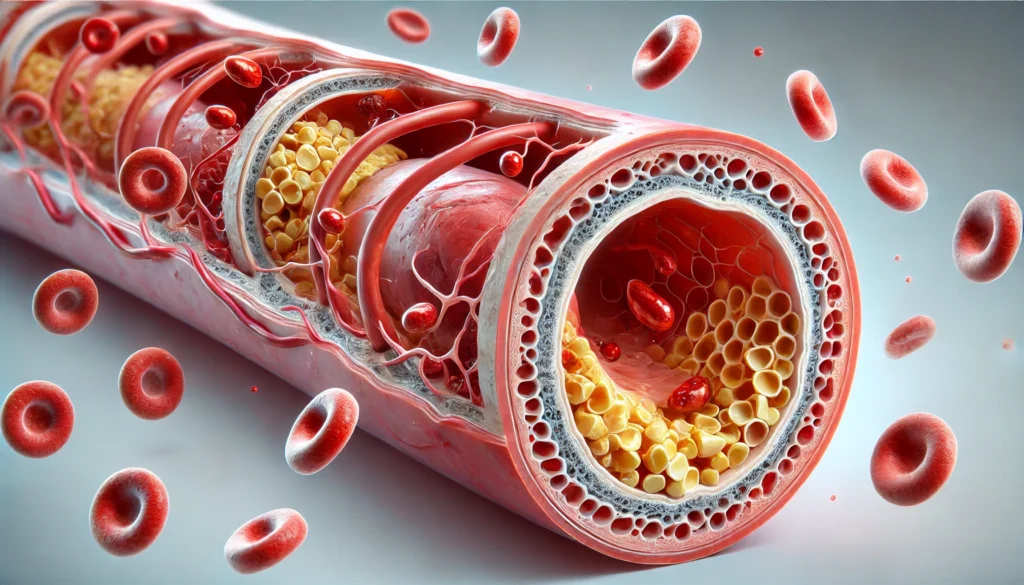
Plaque formation begins when damage occurs to the arterial lining, prompting an immune response that leads to inflammation. Over time, substances such as cholesterol, calcium, and cellular debris accumulate at the site of damage, forming plaques. These plaques can either gradually narrow the arteries or rupture, causing blood clots that completely obstruct blood flow. While high cholesterol has been widely recognized as a major contributor to this process, numerous cases have demonstrated that arterial blockages can occur even when cholesterol levels are within a healthy range.
Several factors beyond cholesterol influence plaque buildup. Chronic inflammation, which can be triggered by conditions such as diabetes, obesity, and autoimmune diseases, is known to accelerate atherosclerosis. Additionally, oxidative stress resulting from free radical damage contributes to arterial damage and plaque instability. Genetic predisposition also plays a role, as some individuals inherit a higher susceptibility to cardiovascular disease regardless of their lipid profile.
The Role of Inflammation in Atherosclerosis
Inflammation is a natural defense mechanism, but chronic inflammation can be harmful to arterial health. When the body’s immune system perceives an injury within the arterial walls, it sends white blood cells to the site, leading to further damage and plaque accumulation. Even in individuals with normal or low cholesterol, persistent inflammation can create an environment conducive to plaque formation.
Conditions such as rheumatoid arthritis, lupus, and chronic infections are linked to increased cardiovascular risk due to their inflammatory nature. Furthermore, lifestyle factors such as smoking, poor diet, and chronic stress contribute to prolonged inflammation, exacerbating the risk of clogged arteries. Understanding the inflammatory process and its impact on arterial health highlights the need for a broader approach to cardiovascular disease prevention beyond cholesterol management alone.
Oxidative Stress and Its Impact on Arterial Health
Oxidative stress occurs when there is an imbalance between free radicals and antioxidants in the body. Free radicals are unstable molecules that damage cells, including the endothelial lining of arteries. When LDL cholesterol undergoes oxidation, it becomes more likely to contribute to plaque formation, even if overall cholesterol levels are within a normal range.
Antioxidants, found in fruits, vegetables, and certain vitamins such as vitamin C and E, help neutralize free radicals and reduce oxidative stress. However, poor dietary habits, exposure to environmental toxins, and excessive alcohol consumption can increase oxidative damage, furthering the progression of atherosclerosis. Incorporating antioxidant-rich foods and reducing exposure to oxidative stressors can play a crucial role in maintaining arterial health.
Genetic Factors and Their Influence on Arterial Blockages
Genetics significantly contribute to cardiovascular disease risk. Some individuals inherit genetic variations that affect lipid metabolism, inflammation levels, or blood vessel function, predisposing them to arterial blockages regardless of cholesterol levels. For example, conditions such as familial hypercholesterolemia, despite its association with high cholesterol, also highlight how genetic factors influence cardiovascular health beyond lipid profiles.
Genetic testing and family history assessments can help identify individuals at higher risk for heart disease. While genetics cannot be changed, lifestyle modifications and medical interventions tailored to an individual’s genetic predisposition can help mitigate cardiovascular risks. Understanding one’s genetic background provides valuable insights into preventive measures and early detection of arterial disease.
Lifestyle Factors That Contribute to Clogged Arteries
While cholesterol is a key consideration in cardiovascular health, lifestyle choices play an equally, if not more, significant role. Diet, physical activity, stress management, and smoking habits all impact arterial health, regardless of cholesterol levels.
Diets high in processed foods, trans fats, and excessive sugars promote inflammation and oxidative stress, accelerating atherosclerosis. Conversely, diets rich in whole foods, fiber, healthy fats, and lean proteins support cardiovascular health. Regular physical activity improves circulation, reduces inflammation, and enhances overall heart function, while sedentary behavior increases the risk of arterial disease.
Smoking is another critical factor, as it damages the endothelium, promotes inflammation, and increases oxidative stress, significantly raising the risk of clogged arteries. Managing stress through mindfulness practices, meditation, and adequate sleep also plays a crucial role in maintaining arterial health, as chronic stress is linked to increased cortisol levels and systemic inflammation.
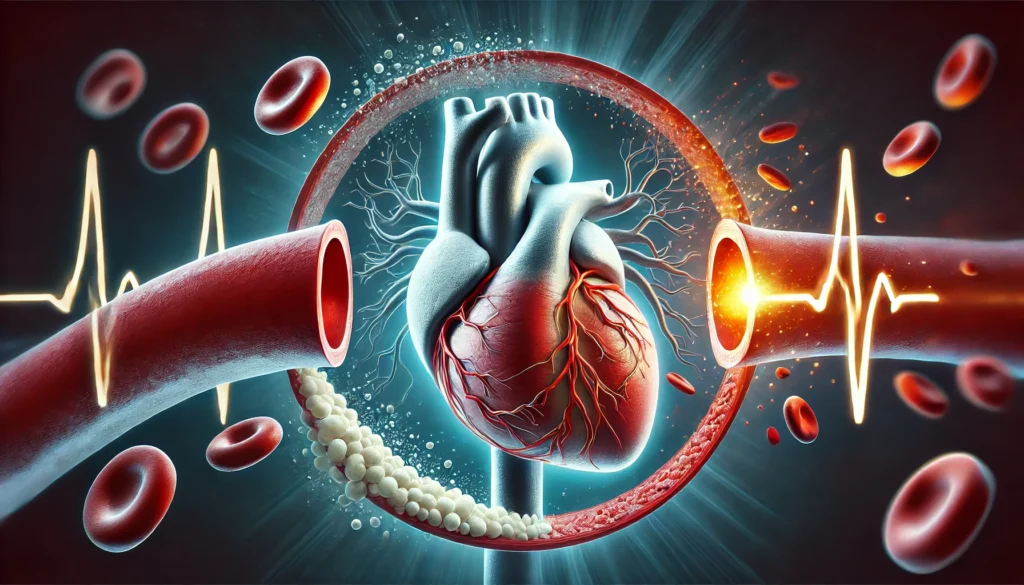
Warning Signs of Clogged Arteries
Recognizing the early signs of arterial disease can prevent severe complications such as heart attacks and strokes. Symptoms vary depending on which arteries are affected, but common warning signs include chest pain (angina), shortness of breath, fatigue, dizziness, and leg pain or numbness. In some cases, clogged arteries remain asymptomatic until a major event occurs, underscoring the importance of regular cardiovascular screenings.
Diagnostic tests such as coronary artery calcium scans, carotid ultrasounds, and angiograms help assess arterial health. Early detection allows for timely interventions, including lifestyle modifications, medication management, and, in severe cases, surgical procedures such as stent placement or bypass surgery.
Frequently Asked Questions (FAQ) on Clogged Arteries and Cholesterol
1. Can you have clogged arteries even if your cholesterol levels are normal?
Yes, it is possible to have clogged arteries despite having normal cholesterol levels. While cholesterol contributes to plaque formation, other factors such as chronic inflammation, oxidative stress, and high blood pressure also play significant roles in arterial blockages. Some individuals have normal lipid profiles but suffer from metabolic disorders, such as insulin resistance, which promote atherosclerosis. Additionally, lifestyle factors like smoking, lack of exercise, and poor diet can accelerate arterial damage regardless of cholesterol levels. Regular screenings and a comprehensive approach to heart health are essential for early detection and prevention.
2. What are some non-cholesterol-related causes of arterial blockages?
Inflammation is a major contributor to arterial disease, as it leads to endothelial damage and plaque formation even in individuals with normal cholesterol. Other factors include oxidative stress, which damages blood vessel linings, and genetic predisposition, which may result in vascular abnormalities or inefficient cholesterol metabolism. Hypertension can also strain the arteries, making them more susceptible to plaque buildup. Additionally, chronic infections and autoimmune diseases can trigger long-term inflammatory responses that compromise arterial integrity. A holistic approach that includes anti-inflammatory foods, regular exercise, and stress management is crucial in reducing cardiovascular risk.
3. Can you have blocked arteries with low cholesterol levels?
Yes, having low cholesterol does not necessarily mean that you are free from cardiovascular risk. Many people assume that keeping cholesterol levels low eliminates the possibility of arterial blockages, but this is not always the case. Other risk factors, such as high homocysteine levels, excessive triglycerides, and chronic inflammation, can still lead to plaque buildup. Moreover, some individuals with very low cholesterol may have deficiencies in essential lipids required for cell repair and immune function, potentially leading to vascular dysfunction. This highlights the importance of evaluating overall cardiovascular health rather than focusing solely on cholesterol numbers.
4. What role does inflammation play in arterial disease?
Inflammation is a key driver of atherosclerosis, independent of cholesterol levels. When blood vessels become irritated due to high blood pressure, smoking, poor diet, or infections, the immune system responds by sending white blood cells to the affected areas. This immune response can inadvertently contribute to plaque buildup, leading to narrowed arteries over time. Chronic inflammatory conditions such as rheumatoid arthritis, lupus, or even persistent gum disease can increase cardiovascular risk. Reducing inflammation through dietary choices, stress reduction, and proper medical management can significantly improve arterial health.
5. How does oxidative stress contribute to clogged arteries?
Oxidative stress occurs when there is an imbalance between free radicals and antioxidants in the body. This imbalance leads to cellular damage, including harm to the endothelial lining of arteries. When LDL cholesterol becomes oxidized, it is more likely to embed itself in arterial walls and contribute to plaque formation. People who consume diets low in antioxidants, such as vitamin C and E, may be more susceptible to oxidative stress-related arterial damage. Avoiding excessive processed foods, smoking, and environmental toxins while consuming antioxidant-rich foods can help mitigate this risk.
6. Can genetics influence the development of arterial blockages even with normal cholesterol?
Yes, genetics play a crucial role in cardiovascular health, affecting how the body processes cholesterol, manages inflammation, and repairs blood vessel damage. Some individuals inherit genetic conditions that predispose them to heart disease, such as familial hypercholesterolemia or certain inflammatory gene variations. Even with normal cholesterol levels, genetic factors can make arteries more prone to damage and plaque accumulation. Genetic testing and family history assessments can provide insights into personalized risk factors, guiding preventive measures and treatment strategies.
7. What lifestyle habits increase the risk of clogged arteries aside from high cholesterol?
Several lifestyle factors contribute to arterial blockages beyond cholesterol levels. Sedentary behavior reduces circulation and increases the likelihood of plaque accumulation. Poor dietary habits, such as consuming trans fats, excessive sugar, and processed foods, contribute to systemic inflammation and endothelial dysfunction. Smoking directly damages the inner lining of arteries and accelerates the formation of plaques. Chronic stress elevates cortisol levels, which can increase blood pressure and promote vascular inflammation. Incorporating regular physical activity, a balanced diet, and stress management techniques can help maintain arterial health.
8. How can someone prevent arterial blockages if their cholesterol levels are already low?
Even with low cholesterol, prevention should focus on maintaining healthy blood vessels and reducing inflammation. Eating a nutrient-dense diet rich in omega-3 fatty acids, fiber, and polyphenols helps protect the arteries from oxidative damage. Engaging in regular cardiovascular exercise improves circulation and promotes endothelial function. Avoiding smoking, excessive alcohol consumption, and chronic stress also plays a significant role in arterial health. Routine medical checkups, including blood pressure and inflammation marker assessments, can help identify risks early on. Preventative measures should always be tailored to an individual’s overall cardiovascular profile rather than just cholesterol levels.
9. What are the best dietary choices for people concerned about arterial blockages beyond cholesterol control?
A heart-healthy diet should include anti-inflammatory and antioxidant-rich foods, even for individuals with normal or low cholesterol. Leafy greens, berries, nuts, and fatty fish provide essential nutrients that protect blood vessels. Whole grains and legumes help regulate blood sugar and prevent insulin resistance, which can indirectly contribute to arterial disease. Fermented foods promote gut health, reducing systemic inflammation that can affect cardiovascular function. Avoiding highly processed foods, excess sugars, and artificial trans fats is critical in maintaining arterial integrity. Combining these dietary habits with a physically active lifestyle further enhances cardiovascular protection.
10. What are some early warning signs of clogged arteries in people with normal cholesterol?
Many people with normal cholesterol assume they are not at risk for heart disease, but subtle warning signs may indicate underlying arterial issues. Symptoms such as fatigue, dizziness, and mild chest discomfort can be early indicators of restricted blood flow. Shortness of breath during physical activity may suggest developing blockages in coronary arteries. In some cases, erectile dysfunction in men can be an early sign of cardiovascular problems due to poor circulation. Unexplained leg pain or numbness, particularly when walking, may signal peripheral artery disease. Since symptoms can be vague or absent until a major cardiovascular event occurs, regular medical screenings remain essential for those concerned about arterial health.
Conclusion: Taking a Comprehensive Approach to Arterial Health
The belief that normal or low cholesterol levels guarantee protection against clogged arteries is a misconception. While cholesterol plays a role in plaque formation, factors such as inflammation, oxidative stress, genetics, and lifestyle choices contribute equally to cardiovascular risk. Understanding these broader influences allows for a more comprehensive approach to heart health, emphasizing inflammation control, dietary improvements, physical activity, and stress management.
Preventive measures such as regular screenings, adopting a heart-healthy lifestyle, and addressing underlying inflammatory conditions can significantly reduce the risk of arterial disease. By shifting the focus beyond cholesterol alone, individuals can take proactive steps to safeguard their cardiovascular health and prevent life-threatening complications associated with clogged arteries.
arterial plaque buildup, cardiovascular health risks, arterial disease prevention, heart disease without high cholesterol, inflammation and heart disease, oxidative stress and arteries, genetic heart disease risk, blood vessel health, silent heart disease symptoms, non-cholesterol heart disease factors, arterial inflammation causes, lifestyle impact on heart health, blood circulation problems, endothelial dysfunction, hypertension and arterial health, diet for artery health, exercise for heart disease prevention, chronic inflammation and arteries, heart attack risk factors, peripheral artery disease signs
Further Reading:
Cholesterol and Artery Plaque Buildup
Heart attack despite low cholesterol?
What are the symptoms of a blocked artery?
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.