Understanding the Complexity of Type 1 and Type 2 Diabetes
Diabetes is often viewed through a binary lens: either you have type 1 or you have type 2. However, emerging research and clinical cases have begun to challenge this long-standing dichotomy. Medical experts are now uncovering rare but clinically significant instances in which a person may exhibit characteristics of both type 1 and type 2 diabetes, raising important questions about diagnosis, treatment, and risk stratification. While each form of diabetes has unique pathophysiology, overlap is not only possible but may also affect how we manage diabetes in the future.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
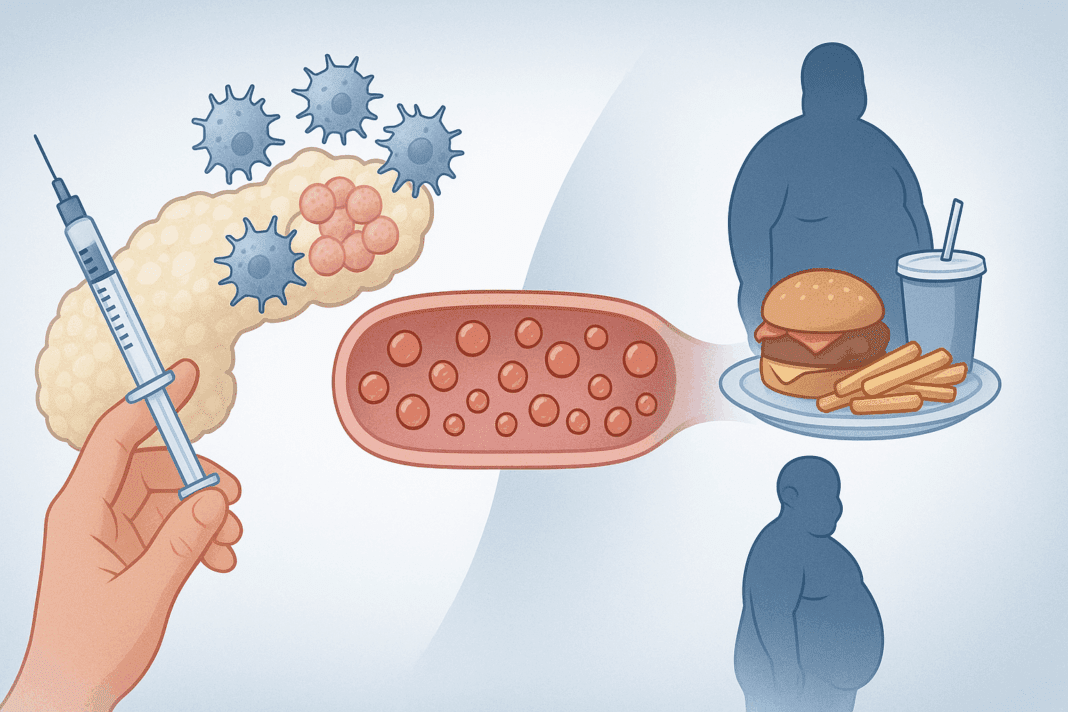
To begin with, it is critical to understand the differences between type I and type II diabetes. Type 1 is an autoimmune disease in which the body attacks the insulin-producing beta cells in the pancreas, leading to a near-total lack of insulin. Type 2, on the other hand, is characterized primarily by insulin resistance, where the body still produces insulin but cannot use it effectively. These distinctions underscore why people often wonder, “can you have diabetes type 1 and 2?” or “can type 1 turn into type 2 diabetes?” The answer lies in the nuances of diabetes pathology and the evolving understanding of metabolic syndromes.
Can You Have Type 1 and Type 2 Diabetes at the Same Time? Exploring Dual Diagnosis
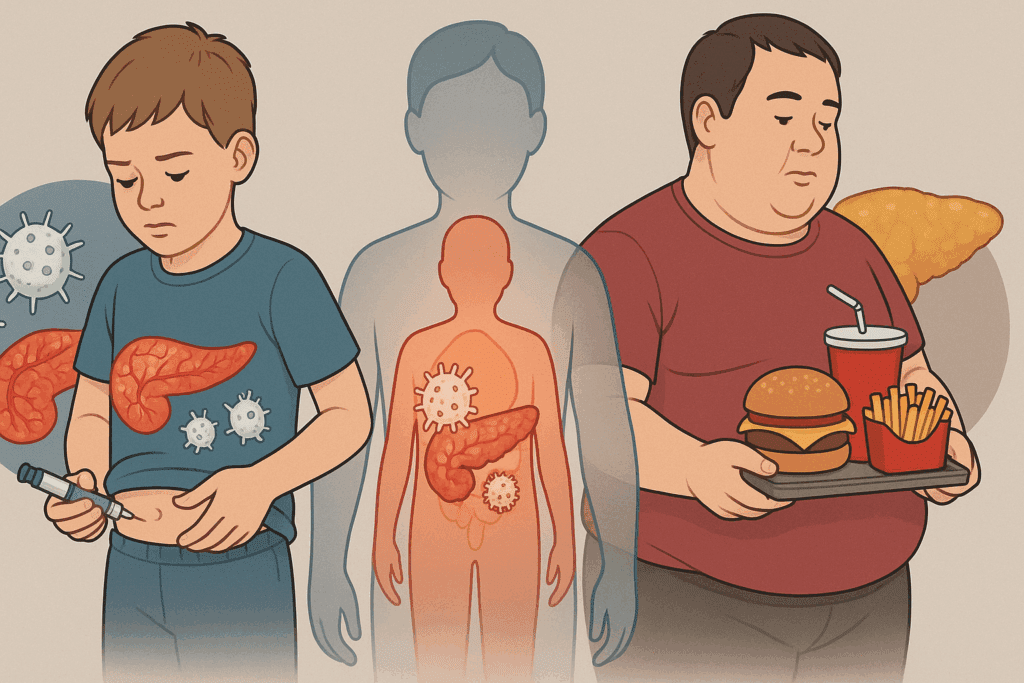
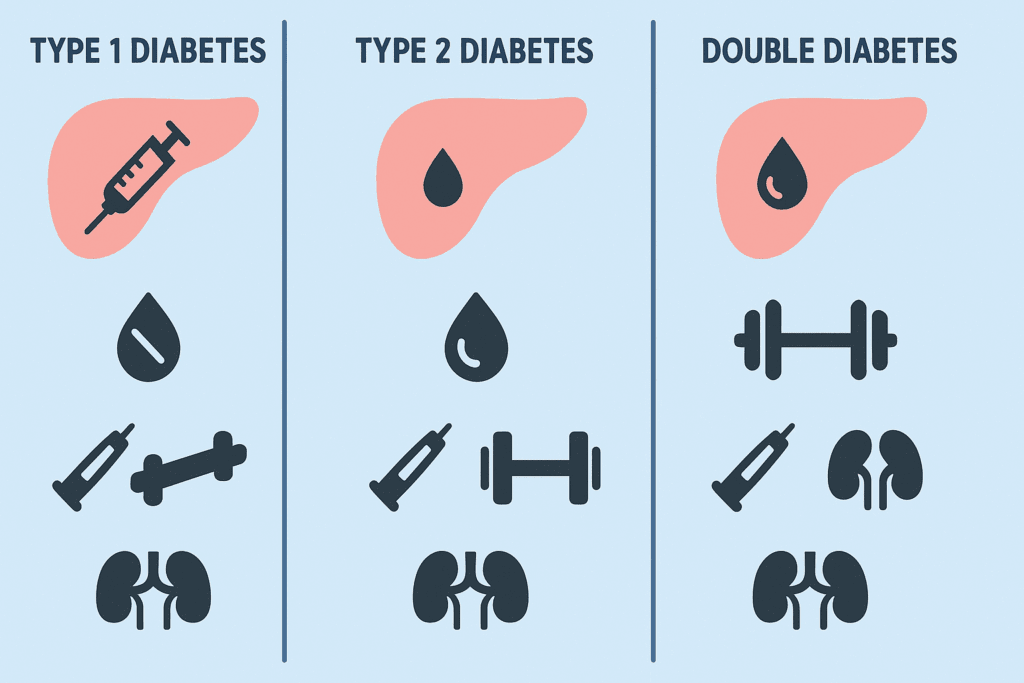
The idea that a single individual could be diagnosed with both type 1 and type 2 diabetes may sound counterintuitive, yet it is medically plausible. This condition is often referred to as “double diabetes” or hybrid diabetes, and it typically occurs when someone with one type of diabetes develops characteristics of the other over time. For instance, a person diagnosed with type 1 diabetes during childhood might develop insulin resistance later in life due to obesity, sedentary lifestyle, or genetic predisposition—hallmarks typically associated with type 2 diabetes.
This raises the question, “can you get type 1 and type 2 diabetes concurrently?” According to a growing body of research, yes—although such cases are rare, they are medically recognized. Clinicians use a combination of diagnostic tests, including C-peptide levels and antibody screenings, to distinguish between autoimmune destruction and insulin resistance. These tools also help answer inquiries like “can diabetes 2 become diabetes 1?” or “can type 1 turn into type 2 diabetes?” While these transitions are not literal conversions from one type to another, overlapping features can complicate the clinical picture and warrant a dual-diagnosis approach.
The Science Behind Double Diabetes: Mechanisms and Risk Factors
To understand how someone might develop both type 1 and type 2 diabetes, it helps to delve into the biological underpinnings of each condition. In type 1 diabetes, the immune system erroneously targets beta cells, halting endogenous insulin production. This leads to absolute insulin deficiency, often requiring lifelong insulin therapy. In contrast, type 2 diabetes results from a progressive decline in insulin sensitivity, often exacerbated by excess adiposity, high caloric intake, and low physical activity.
However, environmental and lifestyle factors can influence the trajectory of either condition. A person with type 1 diabetes who gains significant weight or adopts an inactive lifestyle may start exhibiting the same metabolic abnormalities seen in type 2 diabetes. Similarly, someone initially diagnosed with type 2 may later test positive for islet autoantibodies, indicating a latent autoimmune diabetes of adulthood (LADA) or even a misdiagnosed type 1. These phenomena contribute to the growing recognition of hybrid or double diabetes.
This overlap has led researchers to reconsider questions like “which type of diabetes is the worst?” or “is type 1 or type 2 worse?” The answer often depends on the individual’s metabolic profile, treatment response, and risk of complications. For example, managing dual diabetes typically requires both insulin therapy and lifestyle interventions aimed at improving insulin sensitivity, thereby complicating treatment protocols and increasing the burden of care.
Challenges in Diagnosing and Treating Hybrid Diabetes
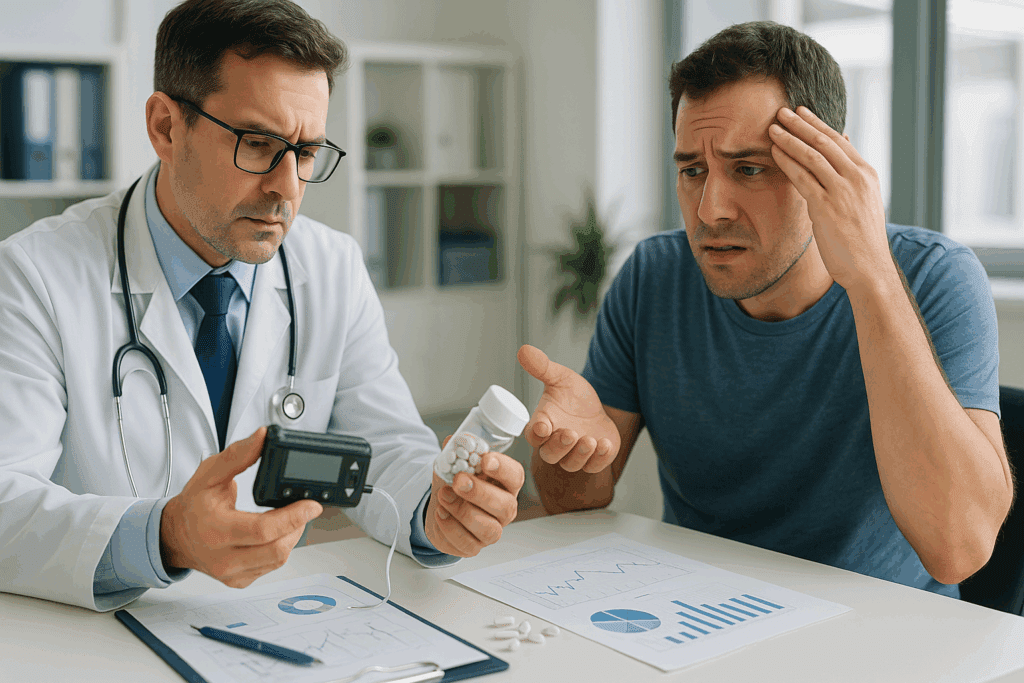
Diagnosing someone with both type 1 and type 2 diabetes presents a clinical conundrum. Since the treatments for these two forms differ—insulin replacement for type 1, and insulin sensitizers like metformin for type 2—it is vital to distinguish the underlying mechanisms. Yet, when both conditions coexist, traditional classification falls short. Many physicians now rely on a broader diagnostic framework that includes genetic testing, autoantibody screening, and an in-depth patient history to determine the best course of action.
In these cases, questions like “can you have type 1 and type 2 diabetes simultaneously?” are not just academic—they guide real-world treatment decisions. A person with double diabetes may need a hybrid treatment strategy: insulin to address the autoimmune component and oral medications or GLP-1 receptor agonists to combat insulin resistance. Diet, physical activity, and stress management also play critical roles. The overlap of these conditions can significantly increase the risk for cardiovascular complications, renal impairment, and neuropathy if not managed meticulously.
Moreover, diagnostic confusion can arise due to overlapping symptoms. For instance, elevated blood sugar, fatigue, and weight fluctuations can occur in both types. Without proper testing, one might erroneously classify a patient as having only one type of diabetes. This misdiagnosis not only skews epidemiological data but also compromises treatment outcomes, making accurate diagnosis a cornerstone of diabetes care.

Research Developments in Double Diabetes: What the Latest Studies Reveal
Recent research has begun to shed light on the prevalence and implications of dual diabetes. A study published in the Journal of Clinical Endocrinology & Metabolism found that nearly 30% of adults with type 1 diabetes develop insulin resistance as they age, particularly if they gain weight or lead a sedentary lifestyle. This trend underscores why questions like “can type 1 turn into type 2 diabetes?” or “can diabetes 2 become diabetes 1?” are increasingly relevant in both research and clinical settings.
Another study conducted by researchers at King’s College London investigated the presence of autoantibodies in patients initially diagnosed with type 2 diabetes. Surprisingly, up to 10% of these individuals showed markers suggestive of an autoimmune component, indicating possible latent autoimmune diabetes in adults (LADA) or a misclassified case of type 1. These findings further blur the lines between what we traditionally label as type I and type II diabetes, suggesting a spectrum rather than a dichotomy.
Such discoveries have spurred interest in whether there is truly a “type A and type B diabetes,” metaphorically speaking, where individuals express features of both ends of the diabetic spectrum. The complexity of these overlapping syndromes necessitates a shift in both medical education and treatment guidelines to accommodate hybrid cases, which are expected to increase as lifestyle-related risk factors become more prevalent globally.
Clinical Implications and Risk Stratification for Double Diabetes
From a clinical standpoint, understanding dual diabetes is crucial for effective risk management and long-term outcomes. Patients with both type 1 and type 2 diabetes traits often have worse glycemic control, higher body mass index, and increased cardiovascular risk compared to those with only one type. This complexity has reignited the debate over “which type diabetes is worse?” and emphasized the need for personalized medicine.
Clinicians must consider more than just glucose levels. Metrics like hemoglobin A1C, lipid profiles, inflammatory markers, and kidney function tests are essential in evaluating the full metabolic picture. In patients with dual diagnoses, treatment regimens often need to be intensified and monitored more closely to avoid complications such as diabetic ketoacidosis, hypoglycemia, or hyperosmolar hyperglycemic state.
Additionally, education plays a vital role. Patients need to understand the difference between diabetes and type 2 diabetes, especially when their treatment plan incorporates elements of both. They should also be made aware that the type 1 or type 2 classification may not fully capture their condition’s complexity, and that hybrid forms are now part of the clinical lexicon.
The Role of Genetics, Environment, and Lifestyle in Dual Diabetes Development
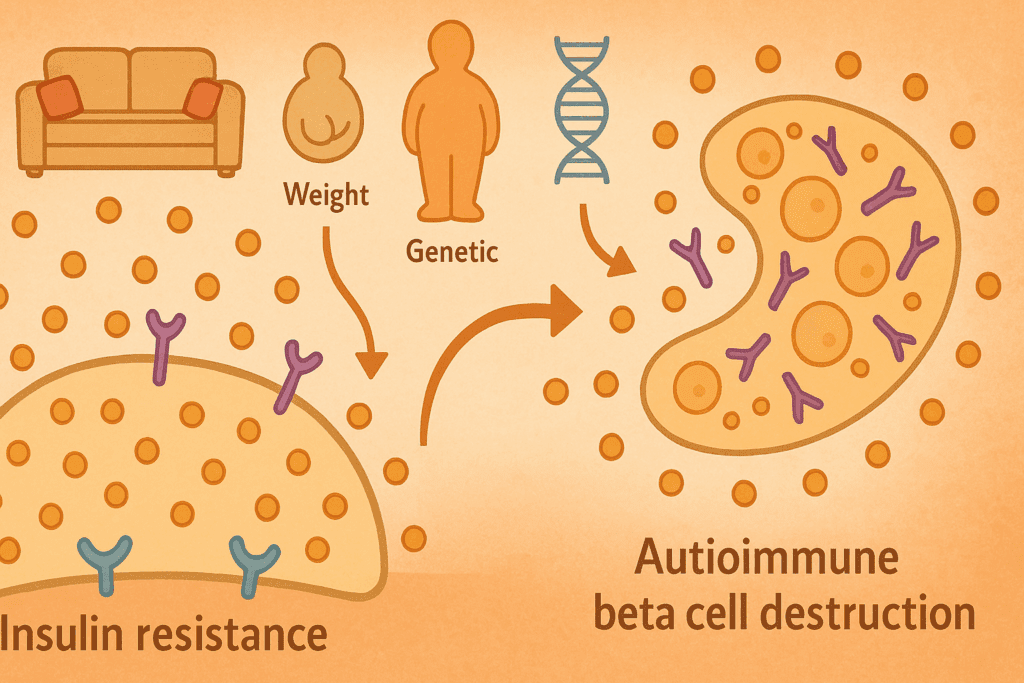
The genesis of dual diabetes lies in the intersection of genetic susceptibility and environmental triggers. Individuals with a family history of autoimmune diseases are at higher risk for type 1 diabetes, while those with a family history of metabolic syndrome are more likely to develop type 2. When both genetic pathways are activated, especially in the presence of modifiable lifestyle factors, the conditions may coexist.
Environmental triggers like viral infections, dietary habits, and exposure to toxins can act as tipping points. In children predisposed to type 1, early-life obesity has been shown to accelerate the onset of symptoms, suggesting that insulin resistance can exacerbate autoimmune damage. Likewise, adults with type 2 who develop severe beta-cell failure may exhibit traits more aligned with type 1, further complicating the classification.
This convergence has given rise to new diagnostic challenges and redefined questions like “is type 1 or type 2 worse?” While both forms have distinct complications, the combination can lead to a more aggressive disease course. Early identification of risk factors, therefore, becomes essential. This includes routine screening for autoantibodies in type 2 patients with poor response to therapy, and early metabolic assessments in type 1 patients who gain weight or have a family history of insulin resistance.
Looking Ahead: The Future of Diabetes Classification and Care
As our understanding of diabetes deepens, many researchers and endocrinologists advocate for a more nuanced classification system. Rather than labeling patients strictly as having type 1 or type 2, some propose a spectrum-based approach that considers autoimmunity, insulin resistance, beta-cell function, and genetic markers. This evolution in classification could improve both diagnostic precision and treatment efficacy.
Precision medicine, aided by artificial intelligence and machine learning, is also poised to revolutionize diabetes care. Algorithms can analyze vast datasets to identify patterns of hybrid diabetes earlier than traditional methods. Such tools could guide clinicians in tailoring interventions, predicting complications, and improving patient outcomes. Meanwhile, public health strategies must also evolve to address lifestyle factors contributing to both forms of diabetes.
In this context, the question “can you have type 1 and type 2 diabetes?” becomes not just a clinical puzzle but a catalyst for rethinking how we define, diagnose, and treat diabetes in the 21st century. By embracing complexity and integrating advances in genomics, diagnostics, and therapeutics, the medical community can offer more individualized and effective care.
Frequently Asked Questions (FAQ): Dual Diagnosis in Diabetes
1. Can you have diabetes type 1 and 2 if you were diagnosed with one early in life?
Yes, it is possible to have characteristics of both diabetes type 1 and type 2, even if one was diagnosed early in life. For instance, individuals with type 1 diabetes diagnosed during childhood may later develop insulin resistance due to weight gain, aging, or lifestyle changes. This condition, often referred to as “double diabetes,” reflects a hybrid of type I and type II diabetes. Though uncommon, it poses unique management challenges, as both insulin therapy and insulin-sensitizing strategies are needed. Regular metabolic screenings can help catch signs of evolving insulin resistance, even in longstanding type 1 cases.
2. Can type 1 turn into type 2 diabetes as someone gets older?
Type 1 diabetes does not turn into type 2 diabetes in the literal sense, as they are driven by different mechanisms. However, someone with type 1 can acquire traits typically associated with type 2, such as insulin resistance, especially if they become overweight or sedentary. This overlap leads to clinical confusion and sometimes raises the question, “can type 1 turn into type 2 diabetes?” It’s more accurate to say that an individual with autoimmune diabetes can also develop insulin resistance. This scenario underscores the importance of adapting treatment as a patient ages and their metabolic needs shift.
3. Which type of diabetes is the worst in terms of complications and daily management?
The question of which type of diabetes is the worst is complex and largely individualized. Type 1 requires constant insulin administration and can be life-threatening without it, while type 2 often progresses silently and may remain undiagnosed for years. In cases where both are present, patients face the double burden of managing insulin dependency and insulin resistance. Psychological stress, treatment fatigue, and risk of complications like cardiovascular disease may increase in dual diagnoses. Rather than ranking them, it’s more practical to focus on early diagnosis, education, and personalized care.
4. Can you have type 1 and type 2 diabetes at the same time, and how is it confirmed?
Yes, a person can have type 1 and type 2 diabetes concurrently, though it is rare. Diagnosis involves testing for both autoimmune markers (such as GAD antibodies) and signs of insulin resistance (like high C-peptide levels). Clinicians may ask, “can you have type 1 and type 2 diabetes together?” especially in patients who do not respond as expected to standard treatment. Confirming a dual diagnosis requires both lab results and clinical history. This diagnosis leads to more complex treatment regimens, often blending therapies from both diabetes types.
5. What factors increase the chances that someone can get type 1 and type 2 diabetes together?
There are several risk factors that may increase the likelihood of developing both diabetes types. A family history of autoimmune disease increases the chance of type 1, while obesity and physical inactivity heighten the risk for type 2. If someone with type 1 adopts a lifestyle that fosters metabolic syndrome, they may eventually display features of type 2. Therefore, it’s plausible to ask, “can you get type 1 and type 2 diabetes if both genetic and lifestyle risks are present?” The intersection of environmental and hereditary factors plays a significant role in such dual developments.
6. Can diabetes 2 become diabetes 1 through disease progression or poor control?
Type 2 diabetes cannot become type 1 through progression or mismanagement. However, in rare cases, patients initially diagnosed with type 2 are later found to have latent autoimmune diabetes in adults (LADA), which behaves more like type 1. This misclassification may lead people to wonder, “can diabetes 2 become diabetes 1?” While the two types are biologically distinct, diagnostic errors do occur. That is why antibody screening is crucial for patients whose condition doesn’t improve with standard type 2 treatments. Accurate classification ensures that appropriate therapies are applied.
7. How do doctors distinguish between type I and type II diabetes when symptoms overlap?
Distinguishing between type I and type II diabetes involves more than evaluating symptoms, as both types can present with fatigue, weight loss, and high blood glucose. Physicians rely on lab tests such as C-peptide levels and the presence of islet autoantibodies. These help clarify whether the pancreas is failing due to autoimmune attack or simply underperforming due to insulin resistance. Because of the blurred clinical presentation, people sometimes ask whether it’s a case of type A and type B diabetes—a colloquial way of expressing the hybrid nature of some diagnoses. In these ambiguous situations, a combination of metabolic and immunologic data provides the clearest answer.
8. Is type 1 or type 2 worse when it comes to long-term health risks?
Determining whether type 1 or type 2 is worse depends on individual context. Type 1 can lead to acute life-threatening episodes like diabetic ketoacidosis, whereas type 2 tends to cause chronic organ damage if left uncontrolled. Those with dual diabetes face the compounded challenge of managing both risks simultaneously. Hence, when patients ask, “is type 1 or type 2 worse?” the answer often lies in their access to care, adherence to treatment, and co-existing conditions. Long-term complications from either can be mitigated with vigilant management and lifestyle modification.
9. What is the key difference between diabetes and type 2 diabetes in clinical discussions?
In everyday language, people often use the term “diabetes” to refer broadly to all types, but clinically, distinctions are essential. The difference between diabetes and type 2 diabetes lies in etiology, treatment, and progression. Type 2 is only one subset of diabetes, with its own set of diagnostic and management criteria. Misusing the term can lead to confusion, especially when communicating with healthcare professionals about treatment options. Precision in language helps ensure that interventions are appropriate for the patient’s specific condition.
10. How can early detection help if someone is developing features of both diabetes types?
Early detection is crucial in identifying individuals who may be on the trajectory toward a dual diagnosis. Monitoring for both autoimmune markers and insulin resistance indicators can allow for preemptive action before full-blown symptoms emerge. For example, a patient with type 1 who gains weight and becomes less responsive to insulin may benefit from metformin to address emerging type 2 traits. Conversely, a type 2 patient with unexplained weight loss and poor glucose control might need screening for type 1 autoantibodies. Recognizing the possibility that one can have diabetes type 1 and 2 equips clinicians and patients to act before complications arise.
Conclusion: Rethinking Diabetes Through the Lens of Dual Diagnosis and Individualized Risk
The notion that a person can simultaneously exhibit characteristics of both type 1 and type 2 diabetes challenges conventional thinking and underscores the need for a more flexible, nuanced approach to diabetes care. While traditional definitions still serve as a foundation, modern science reveals that metabolic health is often more complex than previously believed. This has direct implications not only for diagnosis and treatment but also for how we educate both healthcare providers and patients.
As we continue to ask questions like “can type 1 turn into type 2 diabetes?” or “which type of diabetes is the worst?”, it becomes clear that these are no longer simple either-or queries. The reality is that some patients straddle both categories, requiring hybrid management plans that address autoimmune destruction and insulin resistance simultaneously. Understanding the difference between diabetes and type 2 diabetes, and acknowledging that some patients experience elements of both, allows for a more tailored, patient-centered approach.
The convergence of type I and type II diabetes into a hybrid diagnosis emphasizes the urgency of early screening, personalized interventions, and lifestyle modifications. Clinicians and researchers must remain agile, embracing the evolving landscape of diabetes classification and care. By doing so, they can more effectively address the rising tide of diabetes-related complications and improve long-term outcomes for those living with this multifaceted condition. In short, understanding the interplay between type 1 and type 2 diabetes is not just a medical curiosity—it is a necessary evolution in the way we view, manage, and ultimately prevent one of the world’s most prevalent chronic diseases.
Further Reading:
Initial Combination Therapy in Type 2 Diabetes
Risk Factors Contributing to Type 2 Diabetes and Recent Advances in the Treatment and Prevention
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.