Understanding Gestational Diabetes: A Temporary Condition with Long-Term Implications
Gestational diabetes mellitus (GDM) is a unique form of diabetes that occurs during pregnancy, typically diagnosed between the 24th and 28th weeks of gestation. While it often resolves after childbirth, the condition is far from benign. GDM is associated with increased risks for both the mother and child, including preeclampsia, cesarean delivery, macrosomia, and later development of type 2 diabetes. The question of “can gestational diabetes be reversed” or, more precisely, “can you reverse gestational diabetes” has gained traction in both medical circles and among health-conscious expectant mothers. To address this, it is important to explore what constitutes reversal, how current scientific findings define remission, and the steps individuals can take to protect their long-term metabolic health.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
Unlike type 1 diabetes, which involves an autoimmune destruction of pancreatic beta cells, gestational diabetes is typically the result of pregnancy-induced insulin resistance, superimposed on a background of underlying metabolic vulnerability. Hormones produced by the placenta impair insulin’s effectiveness, causing glucose to accumulate in the bloodstream. In most women, the pancreas compensates by increasing insulin production. However, in those predisposed to insulin resistance, this compensatory mechanism is insufficient, resulting in hyperglycemia.
Given this context, asking whether gestational diabetes can be reversed must be framed within the understanding that it is inherently a transient condition. Still, the implications stretch far beyond pregnancy, making the exploration of prevention and potential long-term remission critical.
Is Gestational Diabetes Truly Reversible or Just Temporarily Controlled?
The notion of reversing gestational diabetes is not entirely straightforward. Because GDM typically resolves after delivery, many healthcare providers might not use the term “reversal” in the same way they would for chronic type 2 diabetes. However, when patients inquire, “can gestational diabetes be reversed?” they are often referring to both the short-term management during pregnancy and the long-term metabolic outcomes after birth.
From a clinical standpoint, reversal during pregnancy means achieving normal blood glucose levels without medication, through lifestyle interventions such as dietary changes and exercise. This level of control is achievable for many women, and studies show that up to 85% of women with GDM can manage the condition through non-pharmacological means. However, this does not eliminate the underlying susceptibility.
More critically, the real question becomes whether gestational diabetes can be reversed permanently to reduce the risk of future diabetes. Research shows that nearly 50% of women with GDM go on to develop type 2 diabetes within 10 years. This alarming statistic highlights the need for proactive, sustained lifestyle changes after delivery. Thus, while gestational diabetes may appear to resolve postpartum, the metabolic dysfunction often persists subclinically, necessitating ongoing vigilance and intervention.

Scientific Evidence Supporting Remission and Risk Reduction
Recent research into gestational diabetes remission has yielded encouraging insights. Longitudinal studies from institutions such as the National Institutes of Health and Kaiser Permanente indicate that sustained dietary improvements, regular physical activity, and breastfeeding can substantially reduce the likelihood of progression to type 2 diabetes. These interventions not only normalize glucose metabolism but also improve insulin sensitivity over time.
One of the most compelling studies on the topic followed more than 4,000 women with a history of gestational diabetes and found that those who adopted at least four of five low-risk lifestyle behaviors—maintaining a healthy weight, eating a balanced diet, exercising regularly, consuming alcohol in moderation, and not smoking—had a 90% lower risk of developing type 2 diabetes compared to those who did not. This strongly suggests that while the condition may not be “cured” in the conventional sense, it can be effectively reversed in terms of risk trajectory.
Further, the Diabetes Prevention Program (DPP), a landmark randomized controlled trial, demonstrated that lifestyle interventions were more effective than metformin in reducing the progression from prediabetes to diabetes in high-risk individuals, including those with prior gestational diabetes. This reinforces the idea that gestational diabetes can, in many cases, be reversed through lifestyle rather than solely relying on medication.

The Role of Nutrition in Reversing Gestational Diabetes
Nutrition remains one of the most potent tools in managing and potentially reversing gestational diabetes. Medical nutrition therapy (MNT), personalized to each patient’s metabolic profile and cultural preferences, can lead to significant improvements in glycemic control. Key components of an effective nutritional strategy include managing carbohydrate intake, emphasizing high-fiber foods, and reducing the consumption of high-glycemic-index meals.
Whole grains, legumes, leafy greens, lean proteins, and healthy fats can help stabilize blood sugar levels. Evidence shows that diets rich in monounsaturated fats and plant-based proteins are associated with improved insulin sensitivity. Moreover, nutrient timing and portion control are equally important. Rather than consuming three large meals a day, spreading food intake into smaller, frequent meals can prevent spikes in blood sugar levels.
Postpartum, maintaining this dietary approach becomes even more crucial. Many women assume that once gestational diabetes disappears, they can return to pre-pregnancy eating habits. However, reverting to a high-sugar, high-fat diet significantly increases the risk of developing type 2 diabetes. Continued adherence to a balanced, low-glycemic diet can, over time, normalize metabolic function and potentially reverse the trajectory of gestational diabetes.

Physical Activity as a Cornerstone of Long-Term Remission
Exercise complements nutrition in reversing gestational diabetes. Physical activity enhances insulin sensitivity, improves glucose uptake by muscles, and promotes overall metabolic health. During pregnancy, moderate-intensity exercises such as walking, swimming, and prenatal yoga can be safely integrated into daily routines, contributing to better glucose control.
Postpartum, structured exercise programs become even more impactful. Research indicates that even moderate levels of physical activity—such as 150 minutes of brisk walking per week—can halve the risk of progressing to type 2 diabetes. Strength training, which helps build muscle mass and improve insulin receptor function, is particularly beneficial when paired with aerobic activity.
Moreover, exercise has mental health benefits that should not be overlooked. The postpartum period can be emotionally taxing, and physical activity can alleviate symptoms of depression and anxiety, both of which are associated with poorer diabetes outcomes. Consistency is key, and incorporating enjoyable forms of movement increases the likelihood of long-term adherence.
The Importance of Breastfeeding in Metabolic Recovery
Breastfeeding provides significant metabolic advantages for both mother and child. For mothers, lactation increases energy expenditure and enhances glucose metabolism. Studies suggest that women who breastfeed for longer durations have a significantly lower risk of developing type 2 diabetes, even after adjusting for other lifestyle factors.
The mechanism behind this benefit lies in the hormonal milieu associated with lactation, which promotes improved insulin sensitivity and lipid profiles. Breastfeeding also facilitates postpartum weight loss, another key factor in mitigating diabetes risk. Additionally, it reduces the infant’s risk of obesity and diabetes later in life by helping to establish healthier metabolic programming from birth.
Given these multifaceted benefits, breastfeeding should be encouraged as a standard component of post-gestational diabetes care. While it is not a stand-alone solution, it serves as an important adjunct in a holistic approach aimed at reversing the condition’s long-term health implications.
Genetics, Ethnicity, and Underlying Risk Factors
While lifestyle plays a pivotal role in whether gestational diabetes can be reversed, genetic predisposition cannot be overlooked. Women of South Asian, African American, Hispanic, and Native American descent are at higher risk of developing GDM, and subsequently, type 2 diabetes. Family history of diabetes further compounds this risk.
Understanding one’s genetic susceptibility is essential for tailoring preventive strategies. For example, women with polycystic ovary syndrome (PCOS) or a personal history of insulin resistance may require more intensive monitoring and earlier intervention. Genetic testing is not yet a routine part of gestational diabetes care, but as precision medicine advances, it may help guide personalized prevention plans.
Nonetheless, even among high-risk populations, evidence supports the notion that gestational diabetes can be reversed—or more accurately, that its progression can be interrupted—through sustained lifestyle changes. Recognizing risk does not equate to inevitability, and proactive management remains the cornerstone of long-term metabolic health.
Medical Monitoring and Follow-Up Care After Pregnancy
Too often, postpartum care is neglected once the immediate concerns of childbirth pass. However, the postpartum period is a critical window for intervening in the natural course of gestational diabetes. Clinical guidelines recommend that women undergo a 75-gram oral glucose tolerance test (OGTT) between 6 and 12 weeks postpartum, yet studies show that nearly half of women fail to complete this screening.
Ongoing monitoring should extend well beyond this initial test. Annual glucose assessments, hemoglobin A1c evaluations, and regular check-ins with primary care providers or endocrinologists can identify early signs of metabolic dysfunction. This proactive approach can help determine whether gestational diabetes has been effectively reversed or if underlying issues persist.
Electronic health records and mobile health technologies offer opportunities to streamline follow-up care and engage patients in their health journeys. By tracking glucose levels, physical activity, diet, and other biomarkers, women can take an active role in maintaining remission and preventing recurrence.
Mental Health and Its Influence on Gestational Diabetes Outcomes
Mental health plays a profound role in diabetes prevention and remission, yet it is often underappreciated in clinical management. Stress, depression, and anxiety are not only common during and after pregnancy but are also independently associated with increased insulin resistance and poor glycemic control.
Mindfulness-based stress reduction, cognitive behavioral therapy, and support groups have shown promise in improving mental well-being and metabolic outcomes in women with gestational diabetes. The psychological burden of managing a high-risk pregnancy should not be underestimated, and integrating mental health support into routine prenatal and postpartum care can yield significant benefits.
Ultimately, reversing gestational diabetes is not simply a matter of diet and exercise—it requires addressing the full spectrum of physical, emotional, and social determinants of health. A holistic model that incorporates mental health support is more likely to result in sustained remission and improved quality of life.
Frequently Asked Questions: Can You Reverse Gestational Diabetes?
1. How soon after delivery should women with gestational diabetes start monitoring for long-term health risks?
Although gestational diabetes often resolves after childbirth, it’s vital to begin postpartum monitoring as early as six weeks after delivery. This initial window offers a unique opportunity to identify any lingering glucose abnormalities before they evolve into chronic conditions. Medical experts recommend a postpartum oral glucose tolerance test (OGTT) during this period, followed by annual screenings. Asking early on whether you can reverse gestational diabetes should be more than a theoretical concern—it should prompt action. These early interventions, coupled with consistent lifestyle assessments, provide the strongest evidence that gestational diabetes can be reversed or at least placed in long-term remission.
2. Does sleep quality play a role in reversing gestational diabetes?
Sleep quality is a significantly underappreciated factor in glucose regulation and metabolic health. Inadequate or disrupted sleep can increase insulin resistance, elevate cortisol levels, and exacerbate hormonal imbalances—all of which may impair your ability to manage or reverse gestational diabetes. Women experiencing postpartum insomnia or sleep fragmentation may unknowingly hinder their metabolic recovery. Establishing sleep hygiene practices, such as maintaining consistent sleep schedules and limiting screen time, can support hormonal balance and improve glucose tolerance. While many focus on diet and exercise, those genuinely seeking to understand if gestational diabetes can be reversed should also consider prioritizing restorative sleep.
3. Can gestational diabetes be reversed more effectively through intermittent fasting postpartum?
Emerging research on intermittent fasting (IF) suggests it may offer metabolic benefits, including improved insulin sensitivity and reduced inflammation. However, the application of IF postpartum requires careful consideration, especially for breastfeeding mothers. While intermittent fasting could theoretically support those asking if gestational diabetes can be reversed, it should only be undertaken under medical supervision. Gradual implementation and modified fasting schedules, such as time-restricted eating with a 12:12 or 14:10 window, might provide gentle metabolic benefits without compromising milk supply. Long-term studies are still ongoing, but early findings suggest IF could be part of a broader strategy for achieving remission after gestational diabetes.
4. How does stress management affect the chances of reversing gestational diabetes?
Chronic stress triggers hormonal responses that raise blood glucose levels, making it more difficult to achieve and maintain glycemic control. Women who incorporate stress-reduction techniques—such as meditation, deep-breathing exercises, or cognitive behavioral therapy—are more likely to report better postpartum metabolic outcomes. When wondering whether gestational diabetes can be reversed, it’s important not to overlook the role of psychological resilience. Stress management supports balanced cortisol levels and improves sleep, appetite regulation, and insulin function. By managing stress proactively, women position themselves more favorably to achieve long-term reversal of gestational diabetes-related risks.
5. Are there any supplements that can support the reversal of gestational diabetes?
While no supplement alone can replace the importance of lifestyle changes, certain nutrients may enhance the body’s ability to stabilize blood sugar levels. Magnesium, vitamin D, and omega-3 fatty acids have been associated with improved insulin sensitivity in postpartum women. However, these should be taken based on lab-confirmed deficiencies and under the guidance of a healthcare professional. For those exploring whether you can reverse gestational diabetes through integrative strategies, supplementing appropriately may offer added support. It’s essential, however, to rely on well-designed, evidence-based regimens rather than unverified over-the-counter products.
6. How do social and cultural factors influence gestational diabetes outcomes and potential for reversal?
Cultural food practices, family support systems, and access to healthcare all influence how effectively gestational diabetes is managed and reversed. For example, in communities where high-glycemic traditional foods are dietary staples, adapting to a diabetes-friendly plan may require culturally sensitive meal planning. Moreover, women who lack support from partners or family may face greater psychological and logistical challenges in sustaining health behaviors postpartum. When considering whether gestational diabetes can be reversed, it’s essential to acknowledge the real-world barriers many women face. Community-based programs that integrate cultural values into diabetes education are showing promise in improving outcomes and promoting long-term remission.
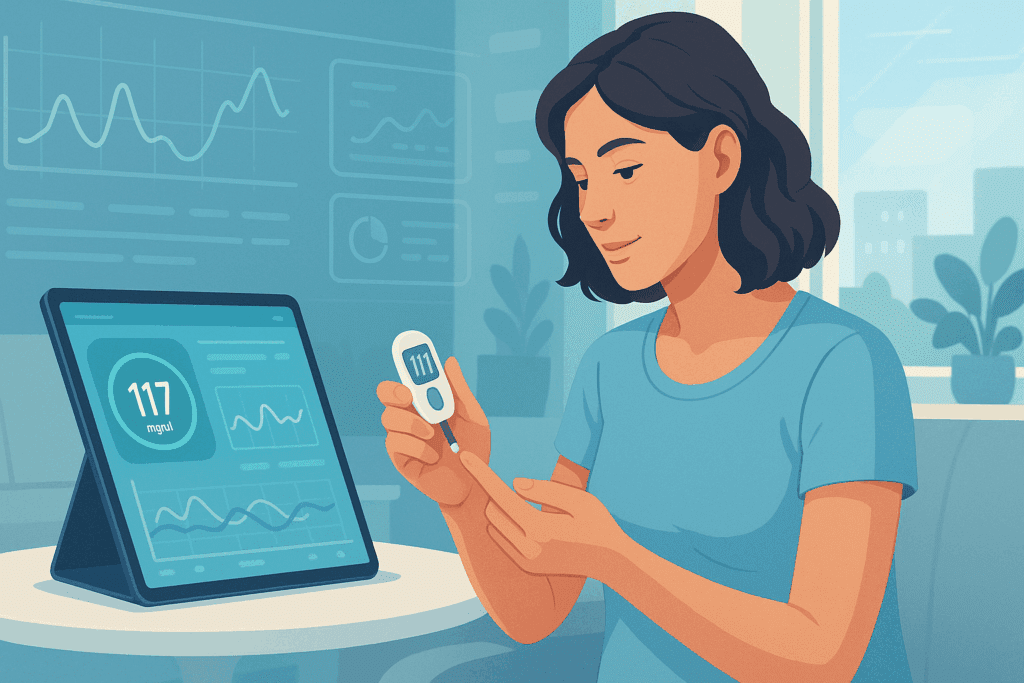
7. Can technology, like continuous glucose monitoring (CGM), enhance efforts to reverse gestational diabetes?
Continuous glucose monitors offer real-time data on blood sugar fluctuations, allowing users to see how food, stress, sleep, and exercise affect their glucose levels. While traditionally used in type 1 and type 2 diabetes, CGMs are increasingly being explored as tools for those in the postpartum phase of gestational diabetes. For women wondering, “can gestational diabetes be reversed if I closely track my levels?”—CGMs provide actionable insights that can dramatically refine diet and activity choices. These devices foster accountability and can empower women to make timely adjustments that support sustained remission. Though not yet standard care, CGMs may represent the future of personalized metabolic monitoring after GDM.
8. Is it possible to reverse gestational diabetes even if it was insulin-treated during pregnancy?
Many women believe that needing insulin during pregnancy dooms them to future diabetes, but that’s not necessarily true. While insulin use suggests a more severe degree of glucose intolerance, it does not preclude the possibility of reversing gestational diabetes in the long run. In fact, research shows that many insulin-treated women who adopt rigorous postpartum health strategies can normalize their glucose metabolism and prevent the onset of type 2 diabetes. The key is recognizing that postpartum efforts must be even more intentional. When insulin has been part of your GDM journey, asking whether you can reverse gestational diabetes is especially relevant—and entirely achievable with a structured and proactive plan.
9. How does weight cycling (yo-yo dieting) affect attempts to reverse gestational diabetes?
Repeated cycles of rapid weight loss followed by regain can impair metabolic flexibility and increase insulin resistance, making it more difficult to maintain stable blood sugar levels. While weight loss is often emphasized as a strategy for reversing gestational diabetes, the method of weight management matters significantly. Sustainable, gradual weight loss supported by a balanced lifestyle is more effective than extreme or short-lived dieting regimens. Women who focus on long-term behavior change rather than quick fixes are more likely to see lasting improvement. Therefore, when asking if gestational diabetes can be reversed, it’s important to remember that how weight is managed is just as crucial as whether weight is lost.
10. What role does partner involvement play in the reversal of gestational diabetes?
Support from a partner can make a profound difference in the outcome of gestational diabetes, especially during the demanding postpartum period. Shared meal planning, physical activity, and mutual health goals create an environment where healthy choices become sustainable. Studies show that women with supportive partners are more likely to follow postpartum screening guidelines and maintain healthier habits. When considering whether you can reverse gestational diabetes, it’s wise to view health as a team effort. Encouraging co-participation in lifestyle changes may not only improve maternal outcomes but can also benefit the entire family’s health trajectory.
Can You Reverse Gestational Diabetes? Key Takeaways for Long-Term Health
The answer to the question “can you reverse gestational diabetes” is both hopeful and nuanced. In the immediate sense, gestational diabetes often resolves after childbirth. However, the deeper challenge lies in reversing the long-term risk trajectory toward chronic metabolic disease. Evidence suggests that with timely, sustained, and comprehensive lifestyle changes—including optimized nutrition, regular physical activity, breastfeeding, and mental health support—many women can reduce or even eliminate their risk of developing type 2 diabetes.
While gestational diabetes may be transient by definition, its impact can be lasting. The science clearly shows that remission is possible, especially when interventions begin early and continue beyond pregnancy. For women asking whether gestational diabetes can be reversed, the research offers a resounding call to action: through informed choices and committed care, it is not only possible to manage the condition but to alter its course entirely. As medical understanding deepens and individualized care advances, the path forward becomes clearer—not just for managing gestational diabetes, but for empowering women with the tools to reclaim their health for the long term.
Further Reading:
Prediabetes Is on the Rise—But It Can Be Reversed
Gestational Diabetes: Causes, Symptoms & Treatment
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


