Understanding the Urgency: Why Differentiating Between Cardiac Arrest and Heart Attack Matters
In the realm of cardiovascular emergencies, few distinctions are as misunderstood yet as vital as the one between cardiac arrest and heart attack. These two terms are often used interchangeably in public discourse, media coverage, and even casual conversations. However, their medical definitions, causes, treatments, and implications are significantly different. Understanding the difference between heart attack and cardiac arrest could mean the difference between timely intervention and tragic outcomes. Despite their distinct mechanisms, both conditions represent serious medical crises that demand immediate attention. With heart disease remaining the leading cause of death globally, awareness and education about these conditions are not just academic—they are matters of public health and personal safety.
You may also like: How to Naturally Reverse 20 Years of Arterial Plaque: Science-Backed Strategies for a Healthier Heart
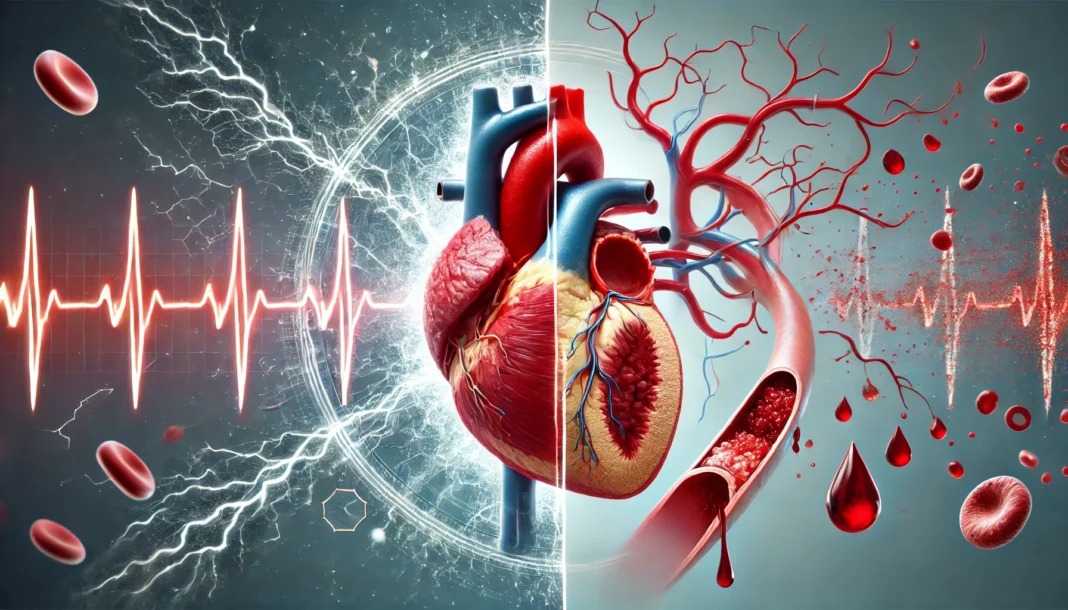
Cardiac arrest occurs when the heart suddenly stops beating due to an electrical malfunction, cutting off blood flow to the brain and other vital organs. A heart attack, on the other hand, is caused by a blockage in the coronary arteries that supply blood to the heart muscle. While a heart attack can lead to cardiac arrest, the two are not synonymous. The confusion between cardiac arrest versus heart attack has contributed to delayed emergency responses and missed opportunities for lifesaving interventions. By demystifying the physiological processes, symptoms, and preventative measures associated with both conditions, we can empower individuals to take appropriate action in critical moments. This article provides a detailed exploration into the key differences, overlapping signs, and essential safety knowledge needed to navigate the high-stakes landscape of cardiovascular emergencies.

What Does Cardiac Arrest Mean? A Closer Look at the Condition
Cardiac arrest is an abrupt and unexpected loss of heart function, typically caused by an electrical disturbance that disrupts the heart’s ability to pump blood effectively. The heart’s rhythmic contractions are regulated by electrical impulses, and when this system malfunctions, it can lead to arrhythmias such as ventricular fibrillation or ventricular tachycardia. These life-threatening arrhythmias prevent the heart from pumping blood, resulting in a complete cessation of circulation. Without immediate intervention, including cardiopulmonary resuscitation (CPR) and defibrillation, death can occur within minutes.
To fully appreciate what cardiac arrest means, it’s important to separate it from myocardial infarction (MI). While they are related and sometimes occur in tandem, cardiac arrest is primarily an electrical failure, whereas MI is a plumbing problem caused by blocked blood flow. The question often arises: what causes cardiac arrest? The answer is multifactorial. It can result from underlying heart disease, especially coronary artery disease, but also from cardiomyopathies, inherited arrhythmia syndromes, severe electrolyte imbalances, drug toxicity, or traumatic injuries.
A common misconception is that all cardiac arrests are secondary to heart attacks. While many cases do result from myocardial infarctions—especially in older adults—this is not always the case. In fact, asking whether most cardiac arrest results from a myocardial infarction highlights the need for clearer public health messaging. Studies show that while a significant portion of cardiac arrest cases are related to heart attacks, other causes like long QT syndrome, Brugada syndrome, and even commotio cordis (a sudden blunt impact to the chest) can lead to arrest without any blockage in the coronary arteries.
Recognizing that cardiac arrest is distinct from a heart attack is vital in shaping timely responses and guiding treatment strategies. With each passing minute without circulation, the chances of survival decrease by 7–10%. Understanding what indicates cardiac arrest and acting without delay can make all the difference.
How a Heart Attack Happens: The Mechanism Behind Myocardial Infarction
A heart attack, clinically termed myocardial infarction, occurs when blood flow to a section of the heart muscle is blocked, usually by a blood clot that forms after a plaque rupture in a coronary artery. This deprives the heart tissue of oxygen and nutrients, causing it to begin dying within minutes. Unlike cardiac arrest, which stops the heart’s electrical activity altogether, a heart attack typically involves a partial or complete blockage of one or more coronary arteries while the heart continues to beat—at least initially.
One of the crucial elements to understand in the discussion of myocardial infarction vs cardiac arrest is the timeline and nature of symptoms. Heart attacks often develop over hours or days with progressive symptoms. Individuals may experience chest pain, pressure, shortness of breath, nausea, and radiating discomfort. These heart arrest symptoms vary from person to person and can be subtler in women, older adults, and those with diabetes.
Although a heart attack can precipitate cardiac arrest, especially if it triggers a dangerous arrhythmia, not every heart attack leads to arrest. Therefore, the assertion that sudden cardiac arrest is the same as a heart attack is inaccurate and potentially dangerous. Treatment also differs significantly. While cardiac arrest requires immediate CPR and defibrillation, a heart attack demands medications like aspirin, nitroglycerin, and rapid revascularization through procedures like angioplasty or coronary artery bypass grafting.
The implications of not recognizing the difference between a heart attack and cardiac arrest can be severe. For example, delaying a 911 call because a person assumes their symptoms are merely indigestion rather than cardiac-related can lead to irreversible damage or death. Therefore, understanding the causes and treatments of myocardial infarction is essential not only for clinicians but for every member of the public.
Symptoms of Cardiac Arrest: What to Watch For When Every Second Counts
Cardiac arrest strikes without warning in many cases, but in others, there may be subtle signs hours or days before the event. The hallmark signs and symptoms of cardiopulmonary arrest include sudden collapse, loss of consciousness, absence of pulse, and cessation of breathing. These symptoms indicate a complete halt of circulatory function and require immediate action.
However, there are sometimes early symptoms of cardiac arrest that precede the event. These can include chest discomfort, heart palpitations, dizziness, unexplained fatigue, or shortness of breath. Such prodromal symptoms are more common in individuals with underlying cardiovascular disease. Recognizing sudden cardiac arrest signs before the actual collapse can allow for earlier intervention, such as seeking emergency care or adjusting medications.
Another important question frequently raised is whether cardiac arrest is painful. Because most individuals lose consciousness within seconds of the heart stopping, the experience is typically not associated with prolonged pain. This offers some reassurance to families grappling with the aftermath of sudden cardiac death. Asking “Is sudden cardiac death painful?” is not just academic—it reflects a human need to understand and find peace in difficult circumstances.
Sudden cardiac arrest symptoms should never be ignored. Whether occurring in an athlete on the field, an elderly person at home, or a middle-aged adult at work, immediate response is essential. The presence of trained bystanders who know CPR and have access to an automated external defibrillator (AED) can double or even triple the chances of survival. Public education on what indicates cardiac arrest is a key component of any comprehensive strategy to improve outcomes.
Signs of a Heart Attack: Understanding the Body’s Alarm System
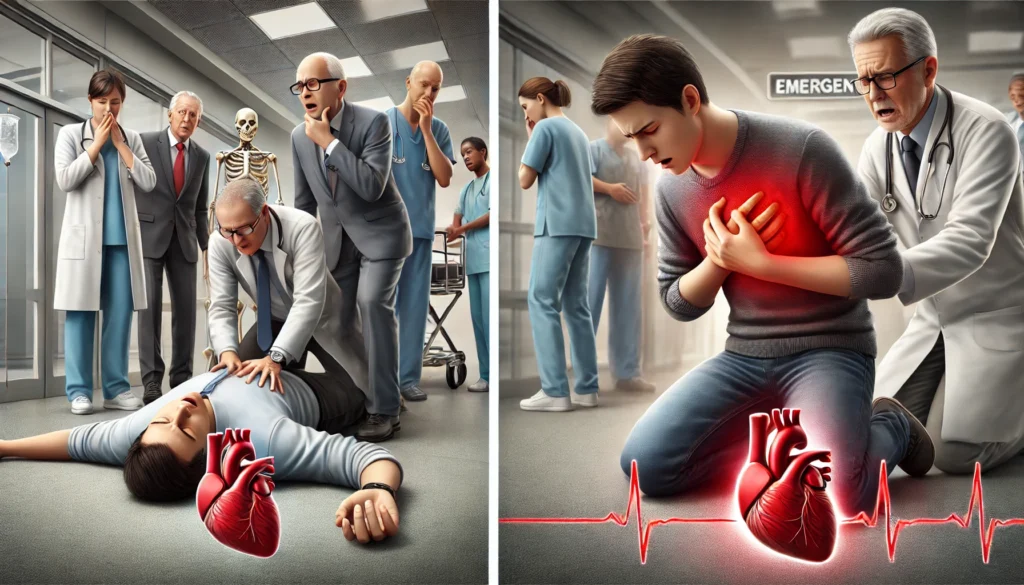
Unlike cardiac arrest, which causes immediate and complete loss of consciousness, a heart attack often provides warning signs that can alert a person to seek medical attention. These signs may include chest pain or pressure, pain radiating to the arm, neck, or jaw, nausea, cold sweats, and shortness of breath. For many, the sensation is described as an elephant sitting on the chest—heavy, tight, and immovable.
That said, symptoms can vary significantly. Women are more likely than men to report atypical symptoms such as fatigue, anxiety, or sleep disturbances. Diabetics may experience a “silent” heart attack with little or no chest pain. This variability complicates diagnosis and increases the importance of understanding both classic and non-classic presentations of heart attack.
The early recognition of heart attack signs is essential because timely treatment can prevent the progression to cardiac arrest. Asking “Is cardiac arrest the same as a heart attack?” demonstrates a need to understand not only the biological differences but also the real-world implications of that distinction. A person having a heart attack is often conscious and able to describe their symptoms, allowing for early intervention. This is in stark contrast to someone in cardiac arrest, who is unresponsive and requires immediate life support.
Moreover, understanding sudden cardiac death symptoms helps bridge the gap between acute myocardial infarction and fatal arrhythmias. In some cases, the two events follow one another in rapid succession, making it all the more critical to recognize symptoms early and respond with urgency.
Can You Prevent Cardiac Arrest? Risk Reduction and Proactive Strategies
While cardiac arrest can occur suddenly and without warning, many cases are preventable through proper management of risk factors and proactive medical care. So, can you prevent cardiac arrest? The answer is yes—at least in many cases—by controlling underlying cardiovascular risk factors and recognizing early warning signs.
High blood pressure, high cholesterol, smoking, obesity, diabetes, and sedentary lifestyle are all modifiable risk factors that contribute to both heart attacks and cardiac arrest. Routine screening, stress testing, and imaging can identify individuals at high risk. Medications such as beta-blockers, statins, and ACE inhibitors are often prescribed to manage these conditions and reduce the likelihood of arrhythmic events.
In certain high-risk populations—such as those with heart failure or inherited arrhythmic disorders—implantable cardioverter defibrillators (ICDs) are life-saving devices that monitor heart rhythms and deliver shocks to restore normal rhythm if a life-threatening arrhythmia occurs. For athletes or young individuals with undiagnosed structural heart conditions, screening programs can help identify those at risk and guide preventive interventions.
Community-level prevention is also critical. Public access to AEDs, widespread CPR training, and timely emergency medical response systems can all reduce mortality from sudden cardiac arrest. Educational campaigns about what causes sudden cardiac arrest and how to respond can empower communities to act quickly and confidently.
Preventing cardiac arrest is not solely the domain of healthcare providers—it is a shared responsibility involving patients, families, schools, workplaces, and public institutions. Understanding what are the reasons for cardiac arrest allows for targeted strategies that can make a meaningful difference in survival rates.
How Fast Will You Die If Your Heart Explodes? Debunking Myths and Clarifying Real Risks
The question “How fast will you die if your heart explodes?” is often asked with a mix of fear and curiosity. While the phrase is hyperbolic, it reflects a real concern about how quickly death can occur from cardiac events. In truth, the heart doesn’t “explode,” but it can rupture due to a massive myocardial infarction or aortic dissection, leading to sudden death. Similarly, cardiac arrest causes death within minutes if untreated.
In cardiac arrest, the lack of circulation causes brain damage in four to six minutes and death in 10 minutes or less. This timeline underscores the urgency of immediate action. The perception of the heart “exploding” may stem from the rapid collapse associated with arrhythmic events or massive structural failures. Regardless of terminology, the outcome is swift and severe without intervention.
This section reinforces the point that both cardiac arrest and heart attack can lead to rapid death, but timely CPR, defibrillation, and medical treatment can reverse the process. By addressing fears in a factual and compassionate manner, we help demystify sudden death and encourage informed preparedness.
Frequently Asked Questions (FAQ): Cardiac Arrest vs Heart Attack
What are some overlooked early warning signs that may indicate a higher risk of sudden cardiac arrest?
While most people are aware of major red flags like chest pain or collapse, many early signs of cardiac arrest are subtle and frequently missed. Symptoms such as unusual fatigue, recurring dizziness, fainting after exertion, or unexplained episodes of breathlessness can serve as preliminary indicators. These signs of cardiac arrest may appear days or even weeks before a sudden episode, particularly in individuals with underlying heart conditions. People often dismiss these symptoms, attributing them to stress or aging, but they can reflect serious arrhythmic disturbances. Understanding what indicates cardiac arrest early allows for intervention before a potentially fatal event occurs.
How do emotional and psychological stressors contribute to cardiac arrest or heart attack risk?
High levels of chronic stress can trigger both cardiac arrest and heart attack through different pathways. Intense stress activates the sympathetic nervous system, increasing blood pressure and heart rate, which may precipitate arrhythmias in vulnerable individuals. Stress is also a known contributor to atherosclerosis, which increases the likelihood of a heart attack that could lead to cardiac arrest. In fact, emotional trauma has been linked to Takotsubo cardiomyopathy, also called stress-induced cardiomyopathy, which mimics a heart attack and can lead to sudden cardiac arrest in severe cases. The difference between heart attack and cardiac arrest becomes especially important in these psychosomatic cases, where emotional well-being directly influences cardiovascular function.
What role does sleep quality play in preventing cardiac arrest and heart attack?
Poor sleep has been increasingly recognized as a contributor to cardiovascular disease, including sudden cardiac arrest. Sleep apnea, in particular, can cause intermittent hypoxia and surges in blood pressure, leading to structural and electrical changes in the heart. These disturbances can predispose a person to arrhythmias and contribute to what causes sudden cardiac arrest during sleep. Even individuals without sleep apnea may be at risk if they consistently get poor-quality rest, as disrupted circadian rhythms affect the autonomic nervous system. Recognizing the link between sleep and heart arrest symptoms broadens the scope of preventive strategies, emphasizing the importance of holistic health.
Can children or teenagers experience cardiac arrest, and what are the warning signs?
Yes, although rare, cardiac arrest can occur in children and adolescents, often due to congenital heart defects or inherited arrhythmia syndromes. In young individuals, the signs and symptoms of cardiopulmonary arrest may not follow typical adult patterns. Episodes of fainting during exercise, a family history of sudden cardiac death, or recurrent palpitations should never be ignored. The difference between cardiac arrest vs heart attack is even more relevant in this group, as heart attacks are extremely uncommon in the young, making electrical abnormalities the primary concern. Pediatric screenings, especially for athletes, are vital in catching these issues before a tragic event unfolds.
Is cardiac arrest always associated with underlying heart disease, or can it happen in otherwise healthy individuals?
While cardiac arrest is often linked to structural heart disease, it can indeed occur in individuals with no known cardiovascular problems. Genetic conditions like Brugada syndrome, long QT syndrome, or catecholaminergic polymorphic ventricular tachycardia can predispose healthy people to lethal arrhythmias. In such cases, what causes cardiac arrest is not lifestyle-driven but instead lies within the electrical architecture of the heart. This underlines why sudden cardiac arrest vs heart attack cannot be assumed to follow the same trajectory or profile. Even physically fit individuals with no symptoms may carry silent genetic mutations that place them at risk.
Are there any technological advancements that help in predicting or preventing cardiac arrest?
Recent innovations have introduced wearable and implantable technologies that monitor the heart in real-time, offering earlier warnings of dangerous rhythms. Smartwatches with ECG capabilities, implantable loop recorders, and smartphone-enabled telemetry tools are becoming more accessible. These devices can alert users to irregular heart rhythms that may signal impending cardiac arrest. Understanding what are the reasons for cardiac arrest, especially in high-risk individuals, now includes leveraging digital health to improve early detection. Although these tools don’t replace medical diagnostics, they serve as valuable adjuncts in bridging the gap between symptoms of cardiac arrest and timely intervention.
How do survival rates differ between heart attacks and cardiac arrests outside of hospital settings?
The survival rate for out-of-hospital cardiac arrest remains low—generally below 10%—primarily due to delayed or absent bystander intervention. In contrast, survival rates for heart attacks, especially when treated promptly, are significantly higher. This discrepancy highlights a crucial aspect of cardiac arrest versus heart attack: cardiac arrest demands an immediate, coordinated emergency response that includes CPR and defibrillation. The concept of “time is myocardium” for heart attacks has its counterpart in “time is life” for cardiac arrest. Efforts to increase CPR training and public access to AEDs are essential in narrowing this survival gap.
What lifestyle changes offer the most protection against both cardiac arrest and heart attack?
Although the origins of cardiac arrest and heart attack differ, their shared risk factors mean many preventive measures overlap. Regular cardiovascular exercise, blood pressure control, smoking cessation, and a heart-healthy diet lower the risks for both events. Stress management and adequate sleep further enhance protection. Learning how to prevent sudden cardiac arrest also involves understanding personal and family medical history, ensuring early screenings, and staying informed about symptoms. These proactive efforts offer a unified defense against sudden cardiac death symptoms stemming from either electrical or circulatory problems.
Why is the phrase “cardiac attack vs heart attack” considered outdated or misleading?
The term “cardiac attack” has been informally used to describe both cardiac arrest and heart attack, leading to confusion in both lay and medical communities. While well-intentioned, it fails to distinguish the vital physiological differences between these two emergencies. The phrase often conflates the causes and treatments, potentially endangering lives when someone delays calling emergency services. Clarifying that cardiac arrest is not the same as a heart attack ensures better emergency recognition and resource allocation. Moving toward medically precise language like myocardial infarction vs cardiac arrest supports improved public education and outcomes.
How should families of high-risk individuals prepare for potential cardiac emergencies at home?
Families with members at elevated risk for cardiac arrest should have a plan that includes CPR certification, accessible emergency contacts, and ideally, a home AED. Education on recognizing sudden cardiac arrest signs and symptoms of cardiac arrest is crucial. For patients with known arrhythmias or heart failure, clear communication with healthcare providers about emergency protocols is essential. Knowing that most cardiac arrest results from a myocardial infarction may inform medication and lifestyle adherence. Proactive preparation bridges the gap between awareness and action, potentially transforming a fatal event into a survivable crisis.
Conclusion: Protecting Your Heart—Knowledge, Action, and the Power to Save Lives
Understanding the distinction between cardiac arrest vs heart attack is more than an academic exercise—it is a crucial step toward informed health decisions, effective emergency response, and improved outcomes. While both conditions share some overlapping symptoms and risk factors, their underlying causes, treatments, and implications differ significantly. Recognizing symptoms of cardiac arrest, learning what causes sudden cardiac arrest, and knowing that cardiac arrest is not the same as a heart attack empowers individuals to act swiftly and appropriately.
Whether you’re wondering “Is sudden cardiac arrest heart disease?” or seeking clarity on the difference between heart attack and cardiac arrest, the takeaway is clear: education saves lives. From bystander CPR to lifestyle modifications and medical therapies, each of us has a role in reducing the devastating toll of cardiovascular emergencies. The next time someone confuses a cardiac attack vs heart attack, you’ll be ready not just with the right words—but with the knowledge that can truly make a difference.
In a world where sudden cardiac death symptoms may appear without warning, and where questions like “Is cardiac arrest painful?” reflect deep human concerns, the antidote is clear, accessible, and actionable knowledge. Arm yourself and your community with that knowledge, and together we can prevent tragedy and promote heart health for all.
cardiovascular emergency response, sudden heart stoppage, emergency heart treatment, electrical heart failure, heart rhythm disorders, life-threatening arrhythmias, coronary artery blockage, heart health education, early warning signs heart issues, defibrillator usage guide, CPR life-saving tips, automated external defibrillator access, arrhythmia awareness, public CPR training, heart function collapse, emergency cardiac care, inherited heart conditions, heart event first aid, medical causes of collapse, high-risk cardiac patients
Further Reading:
Heart Attack and Sudden Cardiac Arrest Differences
Understanding the Difference Between a Heart Attack and a Cardiac Arrest
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.