In the modern landscape of chronic disease management, few conditions demand as much consistent attention and daily vigilance as diabetes. As the prevalence of this metabolic disorder continues to rise worldwide, individuals and health professionals alike are seeking strategies that go beyond pharmaceutical interventions. Controlling blood sugar is not only about medication; it encompasses an integrative approach involving nutrition, lifestyle modifications, and evidence-backed natural remedies. The growing body of research in nutritional science and functional medicine supports the idea that managing diabetes can be more successful and sustainable when complemented by holistic methods. In this article, we’ll explore expert strategies that align with both medical standards and natural health approaches, designed for those who wish to achieve controlled diabetes while prioritizing long-term wellness.
You may also like: 4 Ways to Have a Healthy Diet: Expert Tips Backed by Science for Better Nutrition and Long-Term Wellness
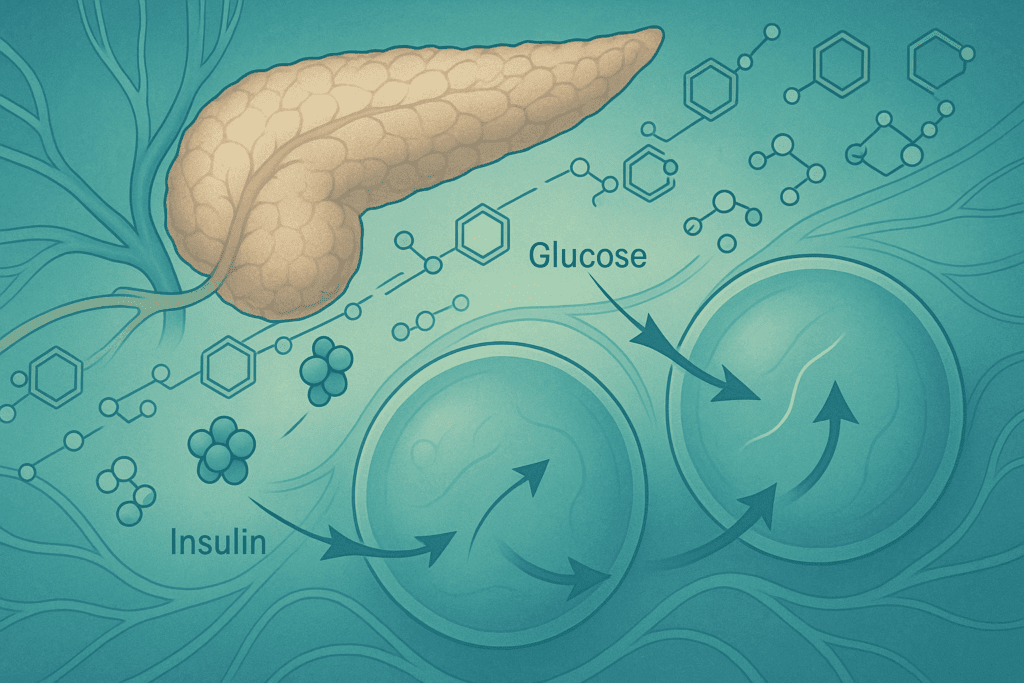
Understanding the Physiology Behind Blood Sugar Regulation
To fully appreciate how to regulate blood glucose naturally, it’s important to first understand the physiological mechanisms involved. The body regulates blood sugar through a complex hormonal dance involving insulin, glucagon, and a host of signaling pathways. Insulin, secreted by the pancreas, facilitates the absorption of glucose into cells for energy or storage. When this system functions properly, blood sugar remains within a narrow, healthy range. However, in individuals with diabetes—whether type 1, type 2, or gestational—this finely tuned system is disrupted. In type 2 diabetes, which is most common, insulin resistance impairs the body’s ability to utilize insulin efficiently, leading to chronic hyperglycemia.
Persistent high blood sugar levels can damage blood vessels, nerves, and organs over time. Hence, controlling blood sugar becomes not just a daily necessity but a vital strategy for preventing complications such as neuropathy, nephropathy, retinopathy, and cardiovascular disease. While insulin therapy or oral hypoglycemics may be necessary for some individuals, others can often achieve controlled diabetes through comprehensive lifestyle interventions. By combining the latest evidence-based insights with time-tested natural approaches, we can illuminate a more personalized and empowering path to health.
Nutrition as the Cornerstone of Blood Sugar Control
Among the most potent tools for managing diabetes is nutrition. Diet directly influences postprandial blood sugar spikes and overall glycemic control, making food choices a first line of defense. The glycemic index (GI) and glycemic load (GL) of foods provide useful frameworks for understanding how different carbohydrates affect blood sugar. Low-GI foods such as legumes, non-starchy vegetables, and whole grains release glucose more slowly into the bloodstream, preventing abrupt spikes. Incorporating these into daily meals can significantly contribute to controlling blood sugar levels naturally.
Equally important is the balance of macronutrients. Diets rich in fiber, healthy fats, and lean proteins have been shown to improve insulin sensitivity and reduce glycemic variability. For example, soluble fiber from oats, flaxseed, and chia slows glucose absorption, while omega-3 fatty acids from fatty fish or walnuts may reduce inflammation that exacerbates insulin resistance. A Mediterranean-style diet—rich in vegetables, olive oil, legumes, and fish—has repeatedly demonstrated efficacy in managing diabetes. Beyond macronutrients, micronutrients such as magnesium, chromium, and vitamin D also play pivotal roles in glycemic regulation. Deficiencies in these nutrients have been associated with poor insulin sensitivity and glucose intolerance, and supplementation under medical supervision can offer meaningful improvements.

Exercise and Physical Activity: The Unsung Heroes of Glycemic Stability
Regular physical activity is a cornerstone of diabetes management and a powerful method for enhancing insulin sensitivity. Exercise promotes glucose uptake in skeletal muscles independent of insulin, thus serving as a direct mechanism for lowering blood sugar. Both aerobic activities like brisk walking, swimming, or cycling and resistance training such as weightlifting have proven benefits. In fact, a combination of the two yields superior outcomes in glycemic control compared to either modality alone.
Even modest increases in daily movement can be transformative. For individuals who may find structured exercise challenging due to physical limitations or comorbidities, incorporating more movement into daily routines—such as gardening, household chores, or using stairs—can also promote blood sugar regulation. Post-meal walks are particularly effective for blunting blood glucose spikes and improving postprandial insulin response. Exercise also reduces stress, enhances cardiovascular health, and supports weight management, all of which are critical for those managing diabetes. Therefore, cultivating an active lifestyle not only supports immediate glycemic control but contributes to overall metabolic resilience.
Stress Management and Sleep: Overlooked Drivers of Blood Sugar Variability
While nutrition and exercise are widely acknowledged in diabetes care, stress management and sleep quality are often underappreciated contributors to blood sugar regulation. Chronic stress triggers the release of cortisol, a hormone that increases glucose production in the liver and inhibits insulin activity. This physiological response, known as the fight-or-flight mechanism, may have been adaptive in short bursts but becomes harmful when sustained. Learning to manage stress through mindfulness-based practices—such as meditation, deep breathing, progressive muscle relaxation, or yoga—can significantly mitigate this effect.
Sleep, similarly, plays a pivotal role in maintaining hormonal balance and metabolic health. Inadequate or poor-quality sleep has been linked to insulin resistance, increased appetite, and impaired glucose tolerance. Sleep deprivation disrupts circadian rhythms and alters the secretion of hormones like leptin and ghrelin, which regulate hunger and satiety. For individuals with diabetes, ensuring seven to nine hours of restorative sleep each night can support more stable blood sugar levels and improve insulin function. Prioritizing sleep hygiene—such as establishing consistent sleep schedules, reducing screen time before bed, and creating a calming nighttime routine—should be considered a foundational aspect of managing diabetes effectively.
Evidence-Based Natural Remedies for High Blood Sugar
While lifestyle changes remain the bedrock of diabetes care, a number of natural remedies for high blood sugar have garnered attention for their evidence-backed benefits. These should not replace medical treatment but may serve as complementary strategies under healthcare supervision. One of the most extensively studied herbal supplements is berberine, a compound found in several plants including goldenseal and barberry. Clinical trials have demonstrated that berberine can lower fasting blood glucose and improve insulin sensitivity, with efficacy comparable to metformin in some studies.
Cinnamon, particularly Ceylon cinnamon, has also shown promise in improving glycemic control. Its active compounds may mimic insulin and enhance glucose uptake by cells. However, results are mixed, and dosage and duration of use are still subjects of investigation. Fenugreek seeds, rich in soluble fiber, may slow carbohydrate digestion and glucose absorption, thereby reducing postprandial spikes. Bitter melon, a traditional remedy in various cultures, contains compounds that may act on insulin receptors and pancreatic beta cells to promote better glucose utilization. Alpha-lipoic acid, an antioxidant, has been studied for its role in improving insulin sensitivity and alleviating diabetic neuropathy.
While these remedies hold potential, it’s imperative that individuals consult their healthcare providers before integrating them into their regimen. Natural does not always mean safe, especially when interacting with prescribed medications. Ensuring that these interventions are tailored to individual needs is essential for safe and effective integration into a broader diabetes management plan.
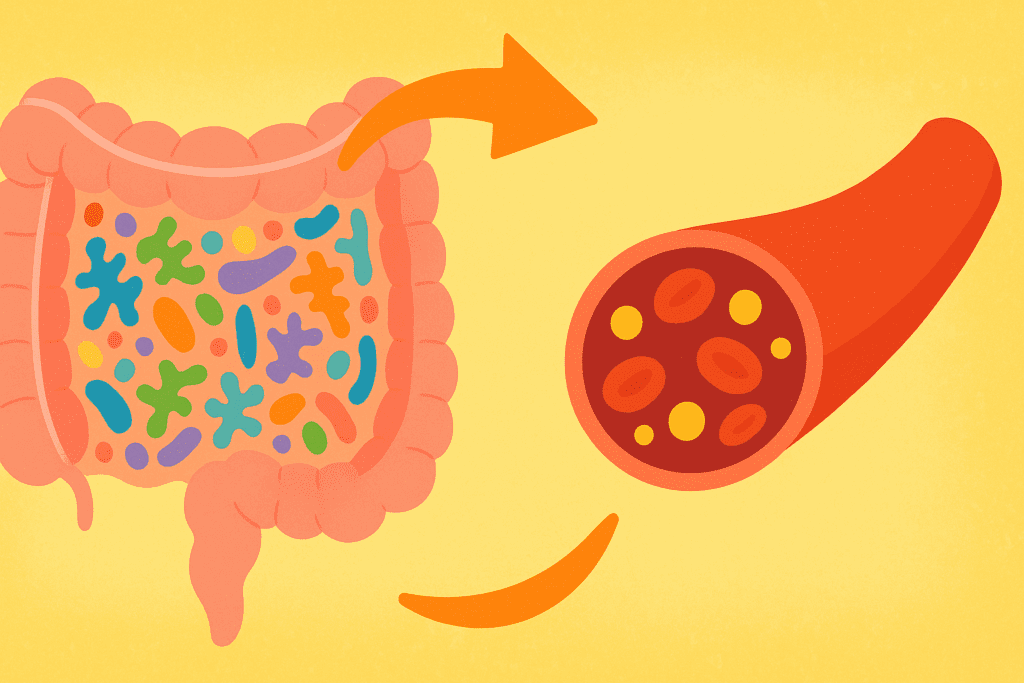
The Role of Gut Health in Controlling Blood Sugar
Emerging research highlights the gut microbiome as a central player in metabolic health, influencing everything from inflammation to insulin sensitivity. The composition and diversity of gut bacteria can affect how the body metabolizes glucose and stores fat. Dysbiosis, or imbalance in gut flora, has been linked to obesity and type 2 diabetes. This discovery has opened new avenues for managing diabetes by supporting gut health through dietary and lifestyle interventions.
Probiotic-rich foods such as yogurt, kefir, sauerkraut, and kimchi can help restore microbial balance, while prebiotic fibers found in garlic, onions, and asparagus provide nourishment for beneficial bacteria. Short-chain fatty acids (SCFAs), byproducts of microbial fermentation of fiber, play a key role in modulating inflammation and enhancing insulin sensitivity. Moreover, reducing ultra-processed foods, which can disrupt gut flora, contributes to a more favorable metabolic environment.
Understanding this gut-blood sugar axis offers new possibilities for individuals seeking natural remedies for high blood sugar. While probiotic supplements are available, whole-food sources of both probiotics and prebiotics are preferable for most people and carry additional nutritional benefits. Maintaining a healthy gut ecosystem can thus serve as a foundational strategy for controlling blood sugar while supporting immune and digestive function.

Weight Management and Its Impact on Controlled Diabetes
Maintaining a healthy weight—or achieving weight loss in the case of overweight or obesity—is strongly correlated with improved blood sugar control. Excess adipose tissue, particularly visceral fat, contributes to chronic inflammation and insulin resistance, making glycemic regulation more difficult. Even modest weight loss, around 5–10% of initial body weight, has been associated with significant improvements in blood sugar, lipid profiles, and overall metabolic health.
Sustainable weight management strategies include focusing on nutrient-dense, satiating foods, practicing mindful eating, and addressing emotional triggers that lead to overeating. Rather than pursuing restrictive diets, individuals often achieve better outcomes by adopting a gradual, personalized approach that fits their lifestyle and preferences. Intermittent fasting and time-restricted eating have also shown some promise in improving insulin sensitivity and reducing fasting glucose levels, although these should be approached with caution and medical oversight, especially in those on glucose-lowering medications.
When weight loss is combined with the other pillars of diabetes management—such as improved sleep, reduced stress, and regular exercise—it enhances the likelihood of achieving and maintaining controlled diabetes. The goal is not perfection but progress, sustained by daily habits that reinforce metabolic balance and long-term health.
Sustaining Lifestyle Changes for Long-Term Glycemic Control
One of the greatest challenges in managing diabetes is not knowing what to do, but doing it consistently over time. Sustainable behavior change requires a combination of motivation, knowledge, support, and environmental alignment. Behavioral psychology suggests that small, achievable goals, when stacked over time, create momentum and lasting change. Building routines around meal planning, physical activity, and sleep can transform once-difficult habits into second nature.
Social support plays an equally critical role. Individuals who are surrounded by supportive family members, friends, or peer groups are more likely to maintain healthy behaviors. Participation in diabetes education programs, community wellness groups, or virtual health coaching platforms can provide both accountability and encouragement. Moreover, embracing a mindset of self-compassion rather than perfectionism helps individuals recover from setbacks without losing motivation.
Technology also offers tools to support long-term success. Continuous glucose monitors (CGMs), fitness trackers, and mobile apps can provide real-time feedback and data-driven insights into how various lifestyle factors influence blood sugar. Used strategically, these tools empower individuals to fine-tune their approach and stay engaged with their goals. Ultimately, sustaining lifestyle change is about creating a personalized system that supports consistency, resilience, and empowerment.

Frequently Asked Questions: Controlling Blood Sugar Naturally
1. Can emotional health impact how effective natural remedies for high blood sugar are?
Absolutely. Emotional health plays a significant role in how well the body responds to interventionsaimed at controlling blood sugar. Chronic emotional stress can elevate cortisol levels, which in turn can increase insulin resistance and disrupt glycemic balance. Even when using effective natural remedies for high blood sugar, unresolved psychological stress may blunt their impact. Incorporating practices like mindfulness meditation or cognitive-behavioral therapy alongside nutritional strategies often yields better results. Emotional resilience isn’t just a bonus—it’s a vital part of managing diabetes with a holistic approach.
2. What role does personalized nutrition play in managing diabetes long-term?
While general dietary guidelines can be helpful, personalized nutrition takes into account individualresponses to food, which can vary widely. For some, legumes may stabilize blood glucose; for others, they may cause spikes. Tools such as continuous glucose monitoring (CGM) devices and food sensitivity testing can help tailor dietary choices more effectively. This precision can enhance the success of natural remedies for high blood sugar and help support controlled diabetes more consistently. Personalized plans make managing diabetes more responsive to your unique metabolic profile.
3. How can workplace environments affect efforts toward controlling blood sugar?
Sedentary routines, irregular meal schedules, and workplace stress can all undermine efforts atcontrolling blood sugar. Skipping meals, consuming high-sugar snacks during work hours, or being glued to a desk for hours can cause glucose levels to fluctuate dramatically. Employers who offer wellness programs, encourage movement breaks, and provide healthier food options contribute significantly to employees managing diabetes more effectively. Even small changes like walking meetings or standing desks can make a difference. Environmental design and workplace culture are often overlooked but essential components of sustained blood sugar control.
4. Are there social or cultural factors that influence the success of natural remedies for high blood sugar?
Yes, cultural beliefs and social practices can profoundly affect how people engage with naturalremedies for high blood sugar. In some communities, herbal therapies and dietary traditions already align with proven nutritional science, enhancing compliance and outcomes. Conversely, stigma around chronic illness or mistrust in natural approaches may hinder adoption. Supportive social networks can help normalize practices for managing diabetes and create a culture of shared accountability. Understanding these social dynamics is key to creating health plans that are both respectful and effective.
5. How does meal timing influence the body’s ability to maintain controlled diabetes?
Meal timing, particularly in relation to circadian rhythms, can greatly affect glucose metabolism.Eating larger meals late at night has been associated with higher fasting glucose levels and reduced insulin sensitivity. Conversely, front-loading calories earlier in the day may enhance the effectiveness of natural remedies for high blood sugar. Intermittent fasting or time-restricted eating (under medical guidance) has shown promise in helping with controlled diabetes. Aligning meals with the body’s natural clock can optimize hormonal balance and improve glycemic outcomes.
6. Can advances in digital health technology help improve results when managing diabetes naturally?
Digital health tools—like smartphone apps, wearable fitness trackers, and CGMs—offer unprecedenteddata on blood sugar patterns and lifestyle impacts. They enable users to identify what behaviors are helping or hindering progress toward controlled diabetes. Some platforms even provide AI-powered coaching or real-time feedback, making it easier to track the effectiveness of natural remedies for high blood sugar. This tech-driven personalization bridges the gap between intention and outcome. When used consistently, digital tools can empower users to make informed decisions and reinforce long-term success.
7. Are there environmental toxins that may interfere with controlling blood sugar?
Emerging research suggests that endocrine-disrupting chemicals (EDCs) like BPA, phthalates, andcertain pesticides may contribute to insulin resistance. These toxins are found in everyday products, from plastics to personal care items. Reducing exposure—such as switching to glass containers or using fragrance-free cleaning products—can support efforts at managing diabetes. While not a standalone solution, detoxifying your environment may enhance the body’s receptivity to natural remedies for high blood sugar. This ecological perspective highlights the importance of considering hidden barriers to glycemic control.
8. How can travel or changes in routine affect someone working toward controlled diabetes?
Travel often brings irregular eating, different time zones, and limited access to familiar foods, all ofwhich can disrupt blood sugar regulation. People managing diabetes may need to plan ahead by packing stable snacks, adjusting medication schedules, and practicing flexibility without compromising their core goals. Natural remedies for high blood sugar, like herbal supplements or stable fiber-rich snacks, can be travel-friendly options for supporting consistency. With planning and adaptability, it’s possible to maintain controlled diabetes even when routines are upended. Travel does not have to derail health if approached mindfully.
9. What’s the connection between hydration and controlling blood sugar?
Hydration is often overlooked but plays a key role in blood glucose regulation. Dehydration can leadto higher blood sugar concentrations because there is less fluid in the bloodstream to dilute glucose. Drinking enough water supports kidney function, which helps the body excrete excess sugar. Moreover, staying hydrated can reduce feelings of hunger that lead to unnecessary snacking, further aiding in managing diabetes. Especially when using natural remedies for high blood sugar, water intake can amplify their effectiveness.
10. Can improving sleep quality directly enhance results from natural strategies for managing diabetes?
Yes, sleep quality has a bi-directional relationship with blood sugar regulation. Poor sleep increasesstress hormones and inflammation, which negatively affect insulin function. In contrast, restful sleep helps stabilize hormonal rhythms and improves the body’s response to natural remedies for high blood sugar. Techniques such as sleep hygiene, magnesium supplementation, and calming herbal teas like chamomile can be valuable allies in controlling blood sugar. Long-term, prioritizing restorative sleep can become a cornerstone in achieving truly controlled diabetes through natural means.
Reimagining Diabetes Management Through Integrative Health
Controlling blood sugar is far more nuanced than simply reacting to glucose readings. It is a dynamic and ongoing process that responds to a multitude of factors—diet, activity, stress, sleep, gut health, and more. As such, managing diabetes effectively demands a multifaceted strategy that honors both the science of conventional medicine and the wisdom of natural health traditions. The goal is not merely the absence of high glucose readings but the presence of vibrant health, metabolic flexibility, and a higher quality of life.
Evidence-based natural remedies for high blood sugar are not fringe ideas; they are increasingly validated by scientific research and embraced by progressive health practitioners. From berberine and cinnamon to microbiome modulation and stress reduction, these strategies offer real hope for achieving controlled diabetes in a way that is safe, sustainable, and empowering. By integrating these remedies into a comprehensive care plan, individuals can gain greater control over their health trajectory and reduce their dependence on medication where appropriate.
As our understanding of diabetes deepens, so too does our appreciation for the body’s remarkable ability to heal and adapt when given the right conditions. By focusing on the root causes of insulin resistance and addressing them with a combination of lifestyle, dietary, and evidence-based natural approaches, we can reimagine what it means to live well with diabetes. Controlling blood sugar naturally is not a fringe pursuit; it is a forward-thinking, holistic pathway to lasting health grounded in both science and self-agency.
Further Reading:
The Science Behind a Plant-Based Diet and Diabetes Reversal
14 Easy Ways to Lower Blood Sugar Levels Naturally
Diabetes management: How lifestyle, daily routine affect blood sugar


