Understanding Coronary Artery Ectasia
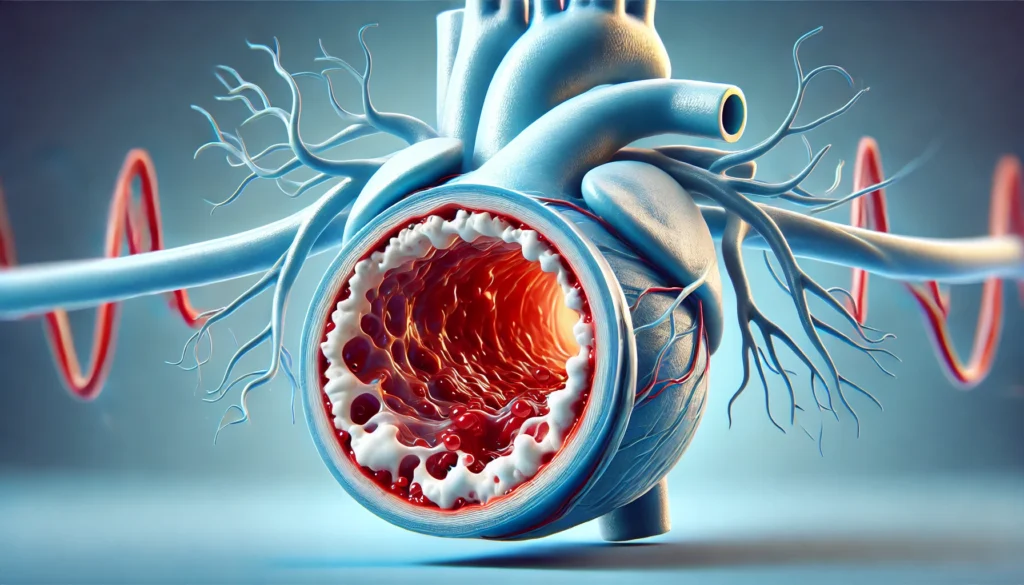
Coronary artery ectasia (CAE) is a relatively uncommon vascular anomaly characterized by the abnormal dilation of the coronary arteries. Unlike atherosclerotic coronary artery disease (CAD), which involves narrowing and obstruction due to plaque accumulation, CAE leads to the excessive enlargement of the arterial lumen. This condition can compromise blood flow dynamics, increase the risk of thrombosis, and contribute to myocardial ischemia. While often considered a variant of CAD, coronary artery ectasia presents distinct pathological and clinical challenges that necessitate targeted management strategies.
The prevalence of CAE varies widely in different populations and is frequently detected incidentally during coronary angiography. The condition may coexist with traditional atherosclerotic disease or manifest independently. Although CAE has been documented in patients with conventional cardiovascular risk factors such as hypertension, hyperlipidemia, and smoking, its precise etiology remains a subject of ongoing investigation. Advances in diagnostic imaging and cardiovascular research have contributed to a deeper understanding of CAE, yet many aspects of its pathophysiology and optimal management strategies remain under active exploration.
You may also like: 5 Modern Treatments for Heart Disease: Advancements in Cardiac Care
Causes and Pathophysiology of Coronary Artery Ectasia
The development of CAE is multifactorial, involving genetic predisposition, inflammatory processes, and endothelial dysfunction. The most commonly implicated factor is atherosclerosis, which contributes to nearly 50% of CAE cases. In these instances, the arterial wall undergoes degenerative changes, leading to localized dilation. However, non-atherosclerotic causes, such as connective tissue disorders, inflammatory vasculitides, and congenital anomalies, also play a crucial role in some patients.
One prevailing theory suggests that CAE arises from an imbalance between arterial wall degradation and repair mechanisms. Matrix metalloproteinases (MMPs), which regulate extracellular matrix remodeling, have been implicated in the breakdown of arterial integrity, leading to aneurysmal dilation. Inflammatory cytokines, including tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6), have also been identified as mediators of arterial wall weakening. Furthermore, endothelial dysfunction, characterized by reduced nitric oxide bioavailability and increased oxidative stress, exacerbates arterial dilation and disrupts normal vascular homeostasis.
Congenital cases of CAE have been documented in individuals with connective tissue disorders such as Marfan syndrome and Ehlers-Danlos syndrome, highlighting the role of genetic factors in arterial wall integrity. Additionally, Kawasaki disease, a pediatric vasculitis that affects the coronary arteries, has been linked to CAE in long-term follow-ups. These diverse etiological pathways underscore the complexity of CAE pathogenesis and the need for personalized diagnostic and therapeutic approaches.
Clinical Presentation and Symptoms
The clinical manifestations of CAE vary widely, ranging from asymptomatic cases to severe ischemic symptoms. Many patients are diagnosed incidentally during coronary angiography performed for other indications. However, in symptomatic individuals, the most common presentation is angina pectoris, which may occur due to altered coronary blood flow dynamics and microvascular dysfunction.
CAE can predispose patients to thrombotic complications, as regions of arterial dilation promote blood stasis and increase the risk of clot formation. This phenomenon can lead to acute coronary syndromes (ACS), including non-ST-elevation myocardial infarction (NSTEMI) and ST-elevation myocardial infarction (STEMI). In such cases, adherence to AHA NSTEMI guidelines and ACC AHA guidelines NSTEMI executive summary recommendations is crucial for optimal patient management.
In some individuals, CAE may cause symptoms resembling vasospastic angina, with episodic chest pain triggered by endothelial dysfunction and transient arterial constriction. Additionally, patients with extensive ectatic involvement may experience exertional dyspnea or atypical chest discomfort due to impaired coronary perfusion. Recognizing these diverse presentations is essential for timely diagnosis and appropriate risk stratification.
Diagnostic Approaches
The diagnosis of CAE relies primarily on coronary imaging modalities, including invasive coronary angiography and non-invasive techniques such as coronary computed tomography angiography (CCTA) and cardiac magnetic resonance imaging (CMR). Coronary angiography remains the gold standard for defining the extent and severity of CAE, allowing for precise measurements of arterial dimensions and identification of coexisting stenotic lesions.
CCTA provides a valuable non-invasive alternative for evaluating coronary morphology and detecting ectatic segments. Advanced imaging techniques, including three-dimensional reconstructions and computational flow dynamics analysis, offer insights into the hemodynamic consequences of CAE. CMR imaging, particularly with gadolinium-enhanced sequences, can assess myocardial perfusion and viability, aiding in the differentiation of ischemic and non-ischemic pathologies.
In addition to imaging studies, biomarker analysis may support risk assessment in patients with CAE. Elevated levels of inflammatory markers, including C-reactive protein (CRP) and fibrinogen, have been associated with CAE progression and adverse cardiovascular outcomes. Endothelial function tests, such as flow-mediated dilation (FMD) and reactive hyperemia peripheral arterial tonometry (RH-PAT), can provide insights into the underlying vascular dysfunction contributing to CAE pathophysiology.
Contemporary Treatment Strategies
The management of CAE remains challenging due to the lack of standardized treatment guidelines. Therapeutic approaches are primarily guided by the presence of ischemic symptoms, the extent of coronary involvement, and associated cardiovascular risk factors. The mainstay of CAE treatment includes antiplatelet therapy, anticoagulation, and strategies targeting endothelial function and vascular remodeling.
Antithrombotic therapy is a cornerstone of CAE management, given the increased risk of thrombus formation in ectatic vessels. Dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor is commonly employed in patients with concomitant atherosclerotic disease or ACS. In cases with extensive arterial dilation and documented thrombi, anticoagulation with warfarin or direct oral anticoagulants (DOACs) may be considered.
Lipid-lowering therapy, particularly with high-intensity statins, plays a crucial role in stabilizing atherosclerotic plaques and mitigating endothelial dysfunction. The application of coronary artery disease guidelines and CAD treatment guidelines in managing dyslipidemia and systemic inflammation is essential for optimizing cardiovascular outcomes in CAE patients.
Frequently Asked Questions (FAQ) on Coronary Artery Ectasia
1. What is the difference between coronary artery ectasia and an aneurysm? While both coronary artery ectasia and aneurysms involve arterial dilation, there are key differences between the two conditions. Coronary artery ectasia refers to a diffuse dilation of the coronary arteries, typically exceeding 1.5 times the normal diameter but involving extensive segments of the artery. In contrast, an aneurysm is a focal, localized dilation that often presents a greater risk of rupture due to its more defined structure. An ectatic artery is more likely to affect the entire vascular integrity, whereas aneurysms may develop in isolation without affecting surrounding arterial segments. Additionally, coronary ectasia is frequently associated with atherosclerosis, while aneurysms can result from congenital abnormalities, infections, or connective tissue disorders.
2. How does arterial ectasia affect blood flow in the coronary arteries? Arterial ectasia significantly alters the normal laminar blood flow in the coronary arteries, leading to areas of turbulent circulation. This disruption can result in sluggish blood movement, which predisposes patients to thrombus formation within the dilated segments. Because ectatic vessels lack the normal elasticity required to propel blood efficiently, ischemic events such as angina or myocardial infarction can occur even in the absence of traditional atherosclerotic plaque buildup. Furthermore, the abnormal expansion of the coronary arteries can lead to vascular remodeling, increasing endothelial dysfunction and further contributing to impaired circulation. These hemodynamic changes make coronary artery dilatation a complex and challenging condition to manage clinically.
3. Can coronary artery ectasia be inherited? There is growing evidence that coronary artery ectasia may have a genetic component, particularly in patients with a family history of connective tissue disorders. Studies have identified potential associations between ectatic vessels and mutations in genes responsible for collagen and elastin synthesis, both of which are critical for maintaining arterial integrity. Some patients with cardiac ectasia also exhibit features of inherited conditions such as Marfan syndrome and Ehlers-Danlos syndrome, which further supports the hypothesis of a hereditary link. Additionally, certain populations have been found to exhibit a higher prevalence of coronary ectasia, suggesting that genetic predisposition may interact with environmental and lifestyle factors. However, more research is needed to determine specific genetic markers and their role in the development of the condition.
4. What are the risks associated with untreated coronary ectasia? Untreated coronary ectasia poses multiple risks, including an increased likelihood of thrombotic complications, myocardial infarction, and progressive vascular dysfunction. Because ectatic arteries promote stagnant blood flow, they create an environment conducive to clot formation, which can result in acute coronary syndromes. Over time, chronic coronary artery dilatation may also lead to heart failure, as the inefficient circulation compromises myocardial oxygen supply. Additionally, patients with significant arterial ectasia may experience recurrent angina, even in the absence of obstructive plaque, due to endothelial dysfunction. Without proper management, these risks can severely impact long-term cardiovascular health and quality of life.
5. How does inflammation contribute to coronary artery ectasia? Inflammation plays a pivotal role in the pathogenesis of coronary artery ectasia by weakening arterial walls and promoting abnormal vascular remodeling. Studies have shown elevated levels of inflammatory markers such as C-reactive protein (CRP) and interleukin-6 in patients with ectatic vessels, suggesting a chronic inflammatory process. This persistent inflammation contributes to the degradation of the extracellular matrix, leading to a loss of structural integrity in the arterial wall. Additionally, inflammatory cells infiltrate the vascular endothelium, exacerbating endothelial dysfunction and increasing susceptibility to thrombosis. As a result, anti-inflammatory therapies are being explored as potential treatment options for managing cardiac ectasia.
6. Is coronary ectasia always associated with atherosclerosis? Although atherosclerosis is the most common cause of coronary ectasia, it is not the sole contributing factor. Approximately 50% of patients with ectatic arteries have concurrent atherosclerotic disease, but the remaining cases arise from non-atherosclerotic mechanisms. Other potential causes include connective tissue disorders, congenital abnormalities, Kawasaki disease, and inflammatory vasculitides such as Takayasu arteritis. In some instances, coronary artery dilatation is idiopathic, meaning no clear underlying cause can be identified. This diversity in etiology highlights the importance of a comprehensive diagnostic evaluation to determine the most appropriate treatment approach.
7. Can lifestyle modifications help manage coronary artery ectasia? While lifestyle changes cannot reverse coronary artery ectasia, they can play a crucial role in managing symptoms and reducing cardiovascular risk. Patients are often advised to adopt a heart-healthy diet rich in anti-inflammatory foods such as omega-3 fatty acids, fruits, vegetables, and whole grains. Regular exercise, particularly moderate-intensity aerobic activity, can enhance endothelial function and improve circulation, although high-intensity workouts should be approached cautiously. Smoking cessation is imperative, as tobacco use exacerbates endothelial dysfunction and accelerates vascular damage. Stress management techniques, including meditation and controlled breathing exercises, may also help mitigate the impact of chronic inflammation on the vascular system. When combined with medical therapies, these lifestyle interventions contribute to improved overall cardiovascular health.
8. Are there any emerging treatments for coronary ectasia? Recent advancements in cardiovascular research have identified several promising treatment avenues for coronary artery ectasia. Novel anticoagulants and antithrombotic therapies are being investigated for their ability to reduce thrombotic risk in ectatic vessels more effectively than traditional medications. Additionally, endothelial-targeted therapies, such as nitric oxide-enhancing agents and antioxidants, are being explored to mitigate endothelial dysfunction. Some experimental studies suggest that regenerative medicine approaches, including stem cell therapy, may aid in restoring arterial integrity by promoting vascular repair. Imaging advancements, such as AI-driven analysis of coronary angiography, are also improving diagnostic precision and treatment personalization. These innovations hold potential for enhancing long-term management strategies for patients with cardiac ectasia.
9. How does coronary artery ectasia affect treatment decisions for other cardiovascular conditions? The presence of coronary artery ectasia can complicate the management of other cardiovascular diseases, particularly when it coexists with traditional coronary artery disease. Because an ectatic artery behaves differently from a stenotic artery, treatment decisions regarding revascularization, stenting, or bypass surgery must be carefully considered. In some cases, percutaneous coronary interventions (PCI) may be less effective due to altered hemodynamics within dilated segments. Additionally, standard anticoagulation protocols may need to be adjusted to account for the higher thrombotic risk associated with coronary artery dilatation. A multidisciplinary approach involving cardiologists, vascular specialists, and hematologists is often required to optimize patient outcomes.
10. What is the long-term outlook for patients with coronary ectasia? The long-term prognosis for patients with coronary ectasia varies depending on the severity of arterial dilation, the presence of coexisting cardiovascular conditions, and individual risk factors. While some individuals remain asymptomatic for years, others may experience recurrent ischemic episodes or develop heart failure due to chronic coronary insufficiency. Advances in medical therapy, including anticoagulation and endothelial function-modulating treatments, have improved symptom management and reduced the likelihood of major adverse cardiac events. Ongoing research into personalized treatment strategies and novel therapeutics offers hope for better long-term outcomes. Regular monitoring, adherence to preventive measures, and proactive cardiovascular care remain essential for optimizing patient prognosis.
Conclusion
Coronary artery ectasia remains a complex cardiovascular condition with diverse etiological factors and clinical implications. While traditional management strategies focus on mitigating thrombotic risk and optimizing vascular health, ongoing research is expanding therapeutic horizons. Future advancements in molecular cardiology, imaging technologies, and precision medicine are expected to enhance our ability to diagnose, risk-stratify, and treat CAE effectively. By adhering to American Heart Association acute coronary syndrome guidelines and emerging evidence-based interventions, clinicians can improve outcomes and quality of life for patients affected by this unique vascular disorder.
cardiac vessel dilation, abnormal coronary arteries, cardiovascular disease management, ischemic heart conditions, myocardial blood flow issues, vascular abnormalities, heart health research, endothelial dysfunction causes, coronary imaging techniques, thrombotic risk factors, arterial wall integrity, heart attack risk assessment, inflammatory cardiovascular disorders, advanced cardiac treatments, heart disease prevention strategies, coronary flow reserve, myocardial ischemia symptoms, non-obstructive coronary disease, personalized cardiology treatments, vascular remodeling research
Further Reading:
Coronary Artery Ectasia: Review of the Non-Atherosclerotic Molecular and Pathophysiologic Concepts
Coronary Artery Ectasia-A Review of Current Literature
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


