Description
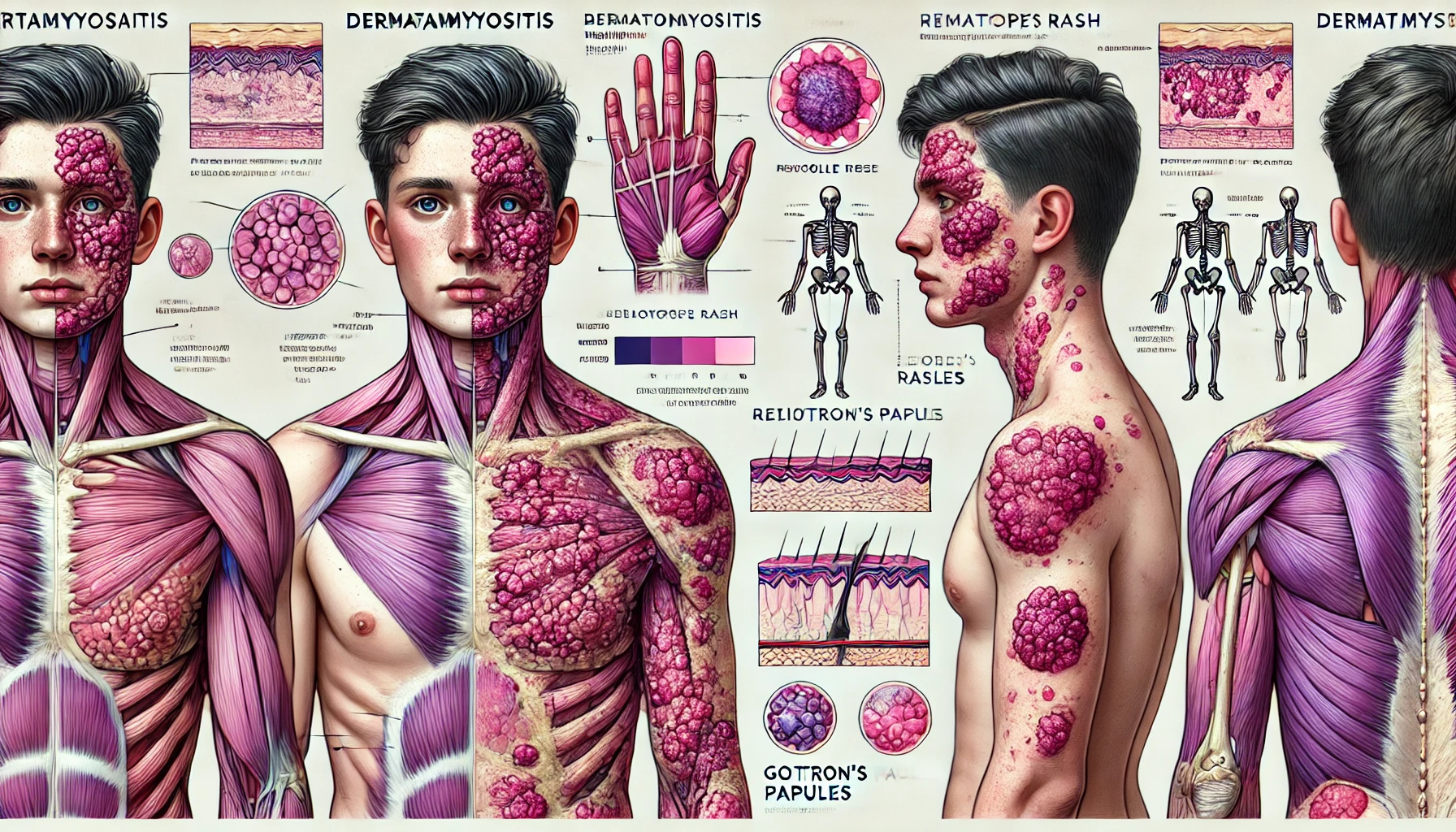
Dermatomyositis (DM) represents a rare autoimmune disorder characterized by skin inflammation (dermatitis) and muscle inflammation (myositis). It often manifests as a rash on the skin and mostly affects the muscles in the shoulders, upper arms, hips, and thighs that are closest to the body’s trunk. Skin symptoms frequently come before or at the same time as muscular discomfort. Due to muscle weakness, this complicated ailment not only presents physical difficulties but also has an impact on overall health. The skin rashes associated with dermatomyositis are typically referred to as heliotrope rash, which presents as a purplish or reddish discoloration around the eyelids, and Gottron’s papules, which are scaly or raised patches on the knuckles and finger joints.
Other skin symptoms may include a rash on the face, neck, chest, back, and other parts of the body. Muscle weakness in dermatomyositis often begins gradually and may affect proximal muscles, making tasks like climbing stairs, lifting objects, or getting up from a seated position challenging. Dermatomyositis can also affect internal organs, leading to complications such as lung inflammation (interstitial lung disease), heart inflammation (myocarditis), and difficulty swallowing (dysphagia). These internal manifestations can further complicate the clinical picture.
You May Also Like:
Bullous pemphigoid: Description, Causes, and Treatment Protocol
Chronic autoimmune urticaria: Description, Causes, and Treatment Protocol
Dermatomyositis: Description, Causes, and Treatment Protocol is an original (MedNewsPedia) article.
Possible Causes
Although the precise origin of dermatomyositis is still unknown, it is thought to be complex and involves immunological, genetic, and environmental components. Dermatomyositis may be caused by a number of reasons, but the precise causes are still poorly understood. Such causes for dermatomyositis include the following: –
Autoimmune Mechanisms: The autoimmune disease dermatomyositis is characterized by the immune system of the patient mistakenly attacking its own tissues. People with dermatomyositis frequently have autoantibodies, like anti-Jo-1 antibodies, which show an immunological response.
Genetic Factors: Dermatomyositis development could be influenced by a person’s genetic makeup. A higher incidence of autoimmune illnesses, like dermatomyositis, has been linked to specific immune systems and inflammatory gene variants.
Environmental Triggers: Dermatomyositis has been associated with a number of environmental variables, including infections and UV radiation exposure. Coxsackievirus infections in particular have been linked to viral infections in rare instances.

Exacerbating and Mitigating Factors
Complex autoimmune conditions like dermatomyositis can be exacerbated or mitigated by a number of circumstances. For dermatomyositis sufferers to effectively manage their condition and enhance their quality of life, it is crucial to comprehend these variables. The following are some causes and effects of dermatomyositis: –
The following are some examples of the aggravating factors: –
Infections: Dermatomyositis symptoms may be brought on by or aggravated by infections. In certain cases, dermatomyositis has been linked to viral infections, specifically coxsackievirus, and various respiratory diseases.
Sun Exposure: Dermatomyositis skin problems can be made worse by ultraviolet (UV) rays from the sun. Increased skin irritation, redness, and rashes are all effects of sun exposure.
Medications: Statins and antibiotics have both been associated with the onset or worsening of dermatomyositis in certain individuals. It is critical to review all medications, particularly over-the-counter medicines and dietary supplements, with a medical professional after receiving a diagnosis of dermatomyositis to assess any potential effects on the disease.
Physical Overexertion: People with dermatomyositis may have increased weakness and muscle exhaustion as a result of physical strain and overuse. Maintaining physical activity while avoiding overdoing it to risk exacerbating symptoms is crucial.
Stress: It is possible that autoimmune diseases like dermatomyositis will become worse with high amounts of stress. Increased inflammation and worsening symptoms may be caused by ongoing stress.

The following are some of the mitigating factors: –
Supportive Care: Dermatomyositis must be managed with adequate rest, a balanced diet, and mental support. A good diet supports general health, and rest helps control fatigue. People can manage the difficulties of the disease with the aid of support from medical professionals and support organizations.
Occupational Therapy: Despite their weak muscles, people with disabilities can complete everyday tasks and routines with the help of occupational therapists. To improve independence, they suggest tactics and assistive technology.
Medications: Corticosteroids and immunosuppressive medicines are frequently used as part of standard dermatomyositis treatment. These drugs assist in reducing inflammation, regulating the inflammatory reaction, and easing dermatomyositis symptoms. It is essential to take the medicines as prescribed and as advised by the physician.
Physical Therapy: Dermatomyositis treatment is crucial for treating the condition. Physical therapists with expertise collaborate with patients to enhance their functional abilities, flexibility, and muscle strength. Maintaining mobility and reducing muscle weakness are both benefits of these exercises.
Regular Follow-Up: It is essential to schedule regular evaluations and follow-up visits with medical professionals to evaluate the disease’s progression and modify treatment regimens as necessary. More effective care may result from the early identification of problems or exacerbations.
Lifestyle Modifications: Exacerbating factors can be lessened through alterations to one’s way of life, such as limiting sun exposure and maintaining proper cleanliness to avoid infections. The illness can be significantly better managed by staying educated about probable triggers and taking preventative action.

Standard Treatment Protocol
Medicine, physical therapy, and other supportive care are frequently used in the treatment of dermatomyositis. Symptom management, autoimmune response management, inflammation reduction, and general improvement of the patient’s standard of living are the main objectives. The typical treatment protocol is described in the following overview: –
Corticosteroids: Dermatomyositis is frequently first treated with corticosteroids like prednisone. These medications support the suppression of the autoimmune reaction and the reduction of inflammation. To reduce unwanted effects, high doses are beginning to be administered before being gradually lowered to a reduced maintenance dose.
Immunosuppressive Drugs: Immunosuppressive medications may be administered when corticosteroids alone are insufficient or to lower the dose of corticosteroids. Mycophenolate mofetil, azathioprine, cyclosporine, and methotrexate are examples of popular options. The immune system is regulated by these drugs, and inflammation is reduced.
Physical Therapy: Dermatomyositis management includes physical therapy as a key component. A physical therapist creates a personalized training regimen to enhance overall function, muscle strength, and flexibility. Exercise on a regular basis helps keep muscles healthy and prevents atrophy.
Occupational Therapy: Patients who need assistance adjusting to daily tasks and routines can benefit from occupational therapy. They offer methods and tools to help people manage everyday tasks despite muscle limitations.
Supportive Measures: Dermatomyositis can be effectively managed by getting enough sleep, eating a balanced diet, and receiving emotional support. To maintain general health, patients should make sure they get adequate sleep and eat a nutritious diet. Patients who need emotional support can benefit from it from their doctors, nurses, and support staff.
Observation and Follow-Up: To track the progression of the illness and alter treatment as necessary, periodic evaluations with medical professionals are crucial. The importance of monitoring for potential problems, like heart or lung activity, cannot be overstated.
Treatment Options
Several alternative therapies and treatments might be taken into consideration along with the conventional course of treatment for dermatomyositis patients to manage certain symptoms or enhance overall health. These additional treatments comprise the following: –
Topical Corticosteroids: Topical corticosteroids may be topically administered to the afflicted areas for regional skin rashes. They assist in easing skin pain and reducing inflammation.
Intravenous Immunoglobulin (IVIg): Only severe instances of dermatomyositis whose services do not improve with conventional therapies should receive IVIG therapy. Immunoglobulins are administered intravenously in order to modify the immune system and manage inflammation.

Over-the-Counter (OTC) Medications: These are outlined below: –
Pain Relievers
Muscle and joint discomfort may be relieved by over-the-counter painkillers like ibuprofen or acetaminophen.
Moisturizers
Emollient lotions and creams may assist with dermatomyositis-related dry, itchy skin.
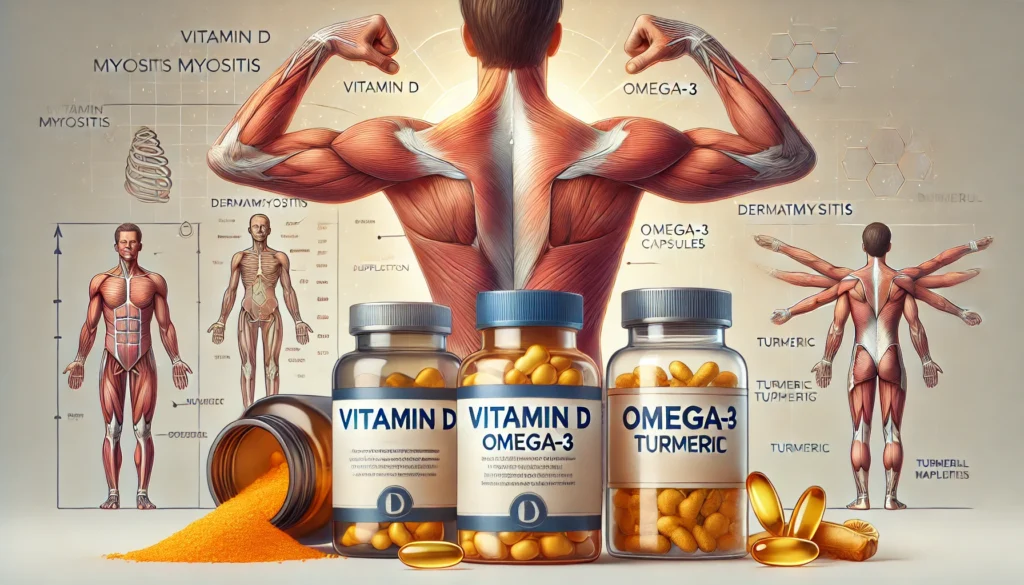
Nutritional Supplements: These include the following: –
Vitamin D
To improve bone health and lower the possibility of osteoporosis, vitamin D supplements might be advised, especially for people on persistent corticosteroid therapy.
Calcium
Sustaining bone strength and lowering the chance of fractures require a proper calcium intake.
Omega-3 Fatty Acids
Dermatomyositis-related inflammation may be decreased by omega-3 supplements, which are frequently made from fish oil and possess anti-inflammatory qualities.
Herbal and Natural Remedies: Alternative and complementary therapies may provide some alleviation and enhance conventional remedies. Before using, it is crucial to examine these alternatives with a healthcare professional. Some possible treatments include the following: –
Aloe Vera
To alleviate skin irritation and minimize redness, aloe vera gel may be used topically.
Turmeric/Curcumin
Turmeric contains a substance called curcumin, which is recognized for its anti-inflammatory effects and may be helpful for people with autoimmune disorders.
Acupuncture
Acupuncture can be effective in treating pain and muscular stiffness in some people with dermatomyositis. A licensed and experienced practitioner should be consulted before receiving acupuncture.
However, working together with their medical team to create a thorough treatment plan that covers their unique requirements and symptoms is essential for people with dermatomyositis. For patients who have dermatomyositis, the combination of conventional medicines and adjunct treatments may help control the condition and enhance their standard of life. To track development and make appropriate modifications to the treatment strategy, regular check-ins with healthcare professionals and continued communication with them are crucial.
Conclusion
Dermatomyositis is a complex autoimmune disorder that requires a multifaceted approach to management. By combining medication, physical and occupational therapy, and lifestyle modifications, individuals can achieve symptom control, improve muscle function, and enhance overall quality of life. While conventional treatments such as corticosteroids and immunosuppressive drugs remain the cornerstone of care, complementary therapies, including nutritional supplements and physical therapy, can provide additional support.
Early diagnosis, regular follow-ups with healthcare providers, and adherence to treatment protocols are essential in managing this condition effectively and preventing complications. Patients and caregivers should stay informed, proactive, and engaged in the treatment process to optimize outcomes and maintain independence. Through personalized care plans and consistent monitoring, individuals with dermatomyositis can lead fulfilling lives despite the challenges posed by the disease.
Additional resources for further reference
https://www.ncbi.nlm.nih.gov/books/NBK558917
https://www.thelancet.com/journals/lancet/article/PIIS0140673699051570/fulltext
https://www.jaad.org/article/S0190-9622(19)32309-6/fulltext
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.