Description
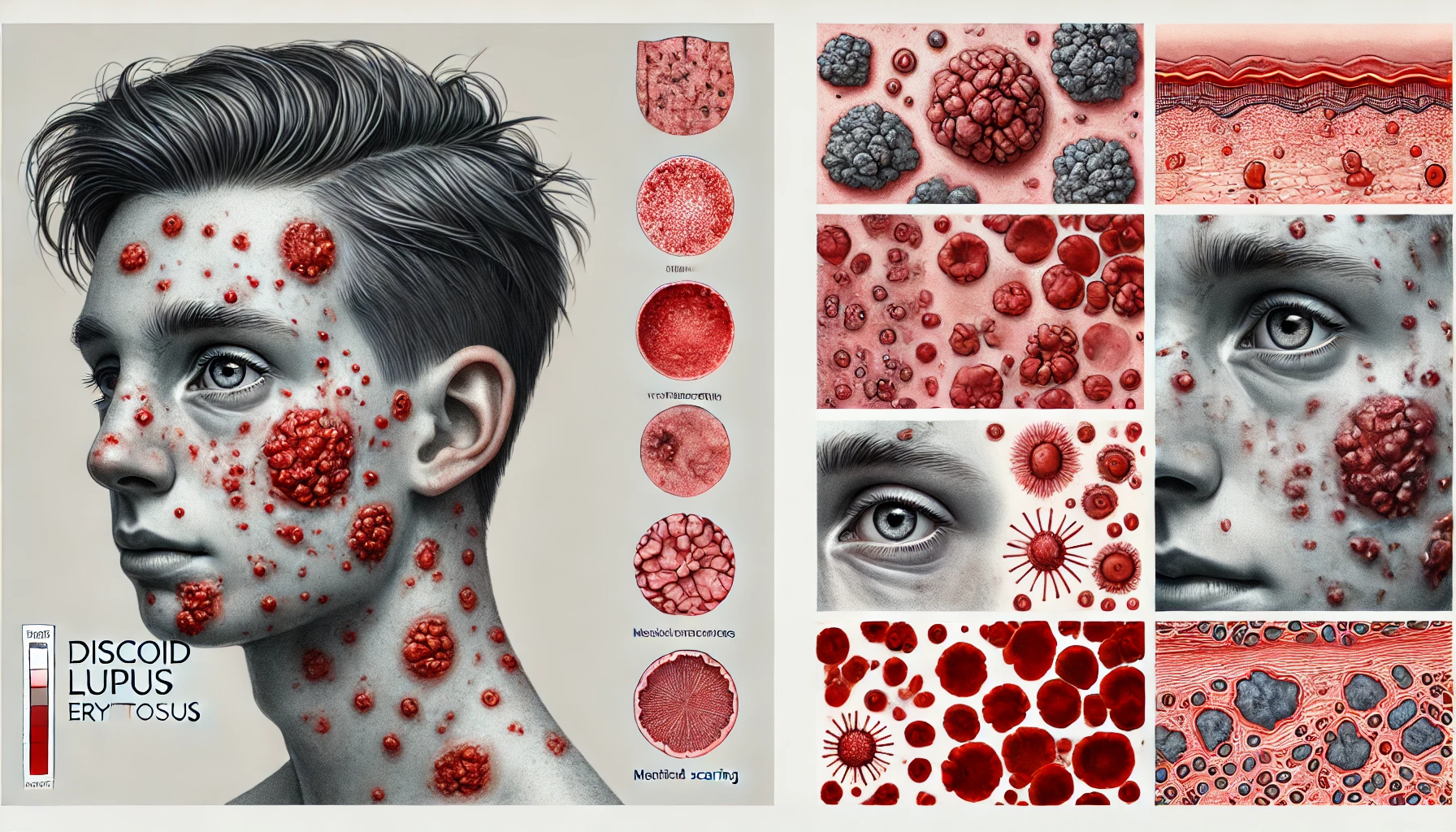
Discoid lupus erythematosus (DLE), another form of systemic lupus erythematosus (SLE), represents a chronic autoimmune disease that mostly affects the skin. It can be identified by the appearance of inflammatory, scaly, and erythematous lesions on sun-exposed body parts like the scalp, face, and ears. While DLE usually affects the skin, it may also flare up in different tissues and organs, sometimes leading to systemic symptoms. Discoid lupus erythematosus manifests as a persistent, recurring autoimmune skin condition. It gets its name from the unique “discoid” or coin-shaped lesions that constitute the disorder. These lesions are often elevated, erythematous, and scaly, and they frequently cause discomfort and disfigurement in those who are affected.
The scalp, face, neck, ears, and upper torso are the parts of the body most frequently afflicted. Patients suffering from DLE frequently develop photosensitivity as a result of the skin lesions that are its trademark. These skin lesions may trigger permanent loss of hair on the head and scarring in extreme situations. Although DLE predominantly impacts the skin, some patients may also experience systemic symptoms. DLE must be recognized as systemic lupus erythematosus (SLE), an extremely pervasive autoimmune condition that can impact numerous organs and tissues.
You May Also Like:
Crohn’s disease (CD): Description, Causes, and Treatment Protocol
CREST syndrome | Limited cutaneous systemic sclerosis: Description, Causes, and Treatment Protocol
Discoid lupus: Description, Causes, and Treatment Protocol is an original (MedNewsPedia) article.
Possible Causes
While the precise origin of discoid lupus erythematosus is still unknown, it is thought to be a result of an interaction of environmental factors, genetic predisposition, and an aberrant immune reaction. The following are some possible root causes and aggravating parameters: –
Immune Dysfunction: DLE is mostly caused by an aberrant immunological response. Tissue damage and inflammation result when the immune system wrongly targets and destroys healthy skin cells. Environmental factors, like ultraviolet (UV) radiation from the sun, may cause or aggravate an inflammatory reaction.
Genetics: Given that DLE tends to occur in families, there exists proof to support a genetic component. Immune regulatory and function-related genes are hypothesized to play a role in the emergence of autoimmune diseases like DLE.
Environmental Triggers: It is commonly known that UV rays of the sun can cause DLE. Infections, hormonal changes, and some drugs can also make the condition worse or cause flare-ups.

Exacerbating and Mitigating Factors
Although DLE predominantly affects the skin, a number of aggravating and mitigating factors, including the ones listed below, can modify its symptoms and intensity: –
The exacerbating factors include: –
Infections: For some DLE patients, viral infections, in particular, can cause illness flare-ups. Colds and flu, which are viral infections, can stimulate immune responses and worsen inflammation, which may exacerbate skin lesions. Maintaining proper hygiene and getting treatment for infections quickly will help lower the likelihood of flare-ups.
Sunlight Exposure: Exposure to ultraviolet (UV) radiation from the sun constitutes one of the most widely recognized aggravating factors for DLE. For those with DLE, sunlight can cause or exacerbate skin sores. Inflammation and immune system stimulation brought on by UV radiation can trigger illness flare-ups. Therefore, it is essential for people with DLE to limit their time in the sun, particularly during peak sunshine hours, and utilize sun protection gear, including sunscreen, wide-brimmed hats, protective clothes, and sunglasses.
Stress: DLE and other autoimmune diseases can be brought on by or made worse by psychological stress and anxiety. Stress can cause immune system dysregulation, which could result in flare-ups or worsen symptoms. Stress can have a negative impact on the condition, although it can be managed with mindfulness exercises, therapy, or relaxation techniques.
Medications: For those who are vulnerable, some drugs can make DLE symptoms worse. Drug-induced DLE flares have been linked to medications including anticonvulsants, antibiotics (like tetracyclines), and antihypertensives (like thiazide diuretics).

The mitigating factors include: –
Infection Prevention: Infection-related disease exacerbations can be lessened by maintaining excellent hygiene, which includes frequent handwashing, and by receiving the appropriate vaccines.
Sun Protection: Consistent sun protection can be one of the best strategies to reduce the symptoms of DLE. This involves applying a broad-spectrum sunscreen with a high SPF, wearing protective clothing like long sleeves and wide-brimmed hats, staying in the shade during peak sun hours (typically from 10 a.m. to 4 p.m.), and employing sunglasses to shield the eyes and sensitive skin around them.
Stress Management: DLE symptoms can be improved by reducing stress through relaxation exercises, yoga, mindfulness meditation, or counseling. Maintaining the immune system in check and lowering the possibility of disease flare-ups are both benefits of stress management.
Medication Management: Patients with DLE must talk to their medical professionals about their drug options and any side effects. Drug-induced flare-up aggravating factors can be reduced with careful medication management.
Lifestyle Modifications: Living a balanced lifestyle may help reduce symptoms. This includes obtaining enough rest, keeping up a balanced diet, engaging in moderate physical activity, and abstaining from known triggers like excessive alcohol or smoking.

Standard Treatment Protocol
A combination of medicinal, topical, and lifestyle therapies is frequently used in the treatment of discoid lupus erythematosus. Treatment focuses mostly on reducing systemic involvement risk, treating skin symptoms, and avoiding scarring. The following components might constitute part of the typical therapy protocol: –
Antimalarial Medications: The antimalarial medications chloroquine and hydroxychloroquine are frequently recommended for mild to severe DLE cases. They have immunomodulatory qualities that can lessen inflammation, modulate the inflammatory response, and stop skin lesions from spreading. The full effects of these medications might not become apparent for several weeks or months.
Topical Corticosteroids: For mild to moderate levels of DLE, topical corticosteroids are frequently used as initial therapy. They influence an autoimmune reaction in the skin by lowering inflammation. Different dosages of these drugs should be considered depending on the dimension and position of the lesions.
Systemic Corticosteroids: Systemic corticosteroids, such as prednisone, may be used for short-term symptom relief in severe cases of DLE if other treatments are unsuccessful. The possibility of serious side effects, however, makes their prolonged use generally discouraged.
Immunosuppressive Medications: Immunosuppressive drugs including methotrexate, mofetil, mycophenolate, or azathioprine could represent a possibility for people with refractory DLE or individuals who are unable to tolerate corticosteroids. The immune system is suppressed, and skin inflammation is decreased by these medications.
Scar Management: Dermatologic therapies like corticosteroid injections or laser therapy might be advised for those who have scarring from prior DLE lesions in order to improve the appearance of their skin.
Sun Protection: It is crucial to educate people about sun safety precautions. Patients should be instructed to stay out of the sun during peak hours, use protective gear like sunglasses and wide-brimmed hats, and cover up with sunscreen containing a high SPF index.
Aloe Vera hydrates and calms irritated skin—Feel the Relief, Buy Aloe Vera Supplements Today!

Treatment Options
Although traditional medical treatments are essential for managing DLE, some people turn to alternative and complementary treatments to ease their symptoms and boost the efficacy of conventional medicine. Several of such possibilities include: –
Aloe Vera: When used topically, aloe vera gel can help calm inflamed skin and minimize inflammation and redness.
Turmeric (Curcumin): An ingredient in turmeric called curcumin is shown to have anti-inflammatory and immunomodulatory effects. It can be included in the diet or consumed as a supplement.
Omega-3 Fatty Acids: Fish oil supplements frequently contain omega-3 fatty acids, which have anti-inflammatory qualities. According to certain research, they might alleviate skin irritation and ameliorate DLE symptoms.
Green Tea: Polyphenols found in green tea may have anti-inflammatory and antioxidant properties. It can be ingested as a beverage or used topically.
Licorice Root: An anti-inflammatory and calming effect can be achieved with licorice root extract. Areas that are affected can receive a topically administered dose.
Calendula: Calendula, commonly called marigold, is an anti-inflammatory and wound-healing plant. Skin lesions may be treated using calendula cream or ointment.
Oatmeal Baths: Skin that is itchy and inflamed can benefit from oatmeal baths. Inconvenience may be lessened by mixing colloidal oatmeal with bathwater.
Stress Reduction Techniques: It may be possible to lessen the frequency and intensity of DLE flares by managing stress using methods like yoga, meditation, or relaxation exercises.
Dietary Modifications: A healthy, balanced diet full of vitamins, minerals, and antioxidants can promote good skin health. Avoiding trigger meals, such as those high in caffeine or spicy meals, might make some DLE patients feel better.
Supplements: Vitamin D supplements might be taken into consideration, particularly when there is a deficiency, but it is important to speak with a healthcare professional before doing so.
Complementary Therapies: Acupuncture, acupressure, and traditional Chinese medicine are examples of alternative therapies that some people with DLE find helpful. However, each person will respond differently to these strategies in terms of effectiveness.
However, it is critical for people with DLE to establish a close working relationship with a healthcare professional, particularly a rheumatologist or dermatologist skilled in addressing autoimmune skin diseases. Standard medical procedures, sun protection, scar care, and auxiliary therapies may assist with managing DLE symptoms successfully and enhance the general standard of living. In order to track therapy success and make any adjustments, it is also crucial to schedule regular follow-up consultations.
Conclusion
Discoid lupus erythematosus (DLE) is a chronic autoimmune condition that primarily affects the skin, posing both physical and emotional challenges for those impacted. Timely diagnosis and personalized treatment are crucial to managing symptoms, minimizing flare-ups, and preventing long-term complications such as scarring or systemic progression. A well-rounded approach—including prescribed medications, sun protection, and stress management—offers significant relief and helps maintain skin integrity.
Complementary therapies and lifestyle changes, such as dietary modifications and mindfulness practices, may further enhance the efficacy of traditional treatments. Close collaboration with healthcare professionals ensures that individuals with DLE receive tailored care that addresses their specific needs, promoting better outcomes and an improved quality of life. Regular follow-ups and ongoing education are essential in empowering patients to manage their condition effectively.
Additional resources for further reference
https://www.ncbi.nlm.nih.gov/books/NBK493145
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD002954.pub3/full
https://onlinelibrary.wiley.com/doi/abs/10.1111/dth.12358
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.