Understanding Blood Pressure: A Foundation for Comparison
Blood pressure is a vital indicator of cardiovascular health, reflecting the force of blood pushing against the walls of arteries as the heart pumps. Measured in millimeters of mercury (mmHg), it is expressed through two numbers: systolic pressure, which captures the force when the heart contracts, and diastolic pressure, which records the force when the heart is at rest. Normal blood pressure for the general population is often cited as approximately 120/80 mmHg. Deviations from this benchmark may indicate underlying health concerns or, in some cases, physiological adaptations based on lifestyle, including exercise levels. Understanding the meaning and significance of blood pressure is crucial before evaluating how it may differ in specific populations like athletes.
Unlike the average individual, athletes tend to engage in frequent, high-intensity physical activity that fundamentally alters cardiovascular function over time. This includes increases in heart size, enhanced stroke volume, and improved vascular flexibility. These physiological adaptations raise an important question: do athletes have different blood pressure profiles compared to non-athletes? To explore this, one must consider not just resting blood pressure, but also how an athlete’s blood pressure responds to physical exertion, recovers afterward, and behaves in both the short and long term.
The notion of “athlete blood pressure” is increasingly studied in both sports medicine and cardiology. Experts recognize that exercise-induced cardiovascular adaptations can produce blood pressure readings that fall outside conventional norms while still reflecting good health. This distinction is essential to avoid misinterpreting what may be normal for an athlete as pathological when viewed through a non-athletic lens.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Athlete Blood Pressure vs. General Population: Key Differences
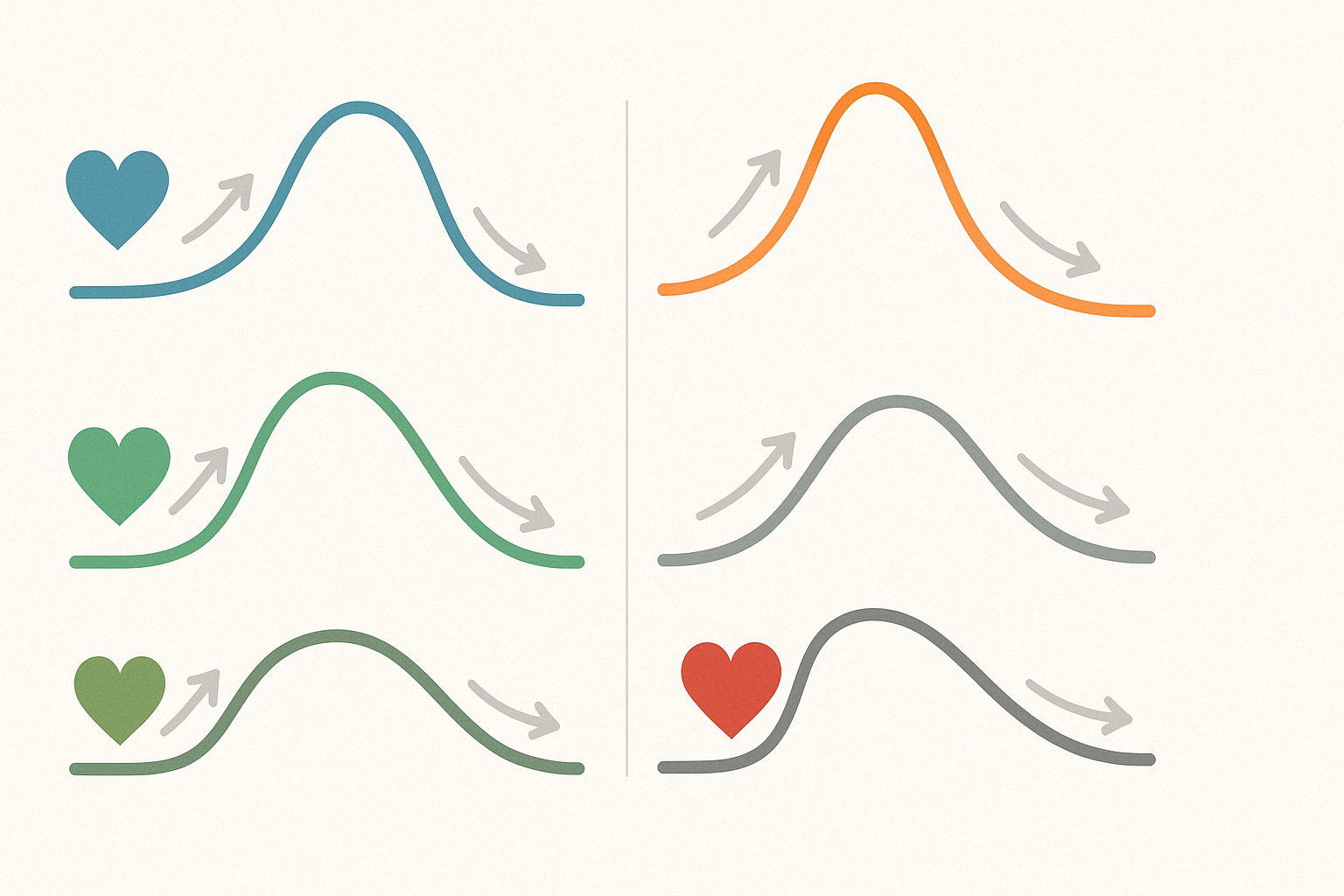
In evaluating whether athletes have different blood pressure than the general population, several important patterns emerge. Research has shown that athletes—especially those involved in endurance sports—often exhibit lower resting heart rates and, correspondingly, lower resting blood pressure. This is largely due to enhanced parasympathetic nervous system activity and increased efficiency of the cardiovascular system. For instance, elite marathon runners may present with resting blood pressure significantly below the 120/80 mmHg average, yet remain in excellent health.
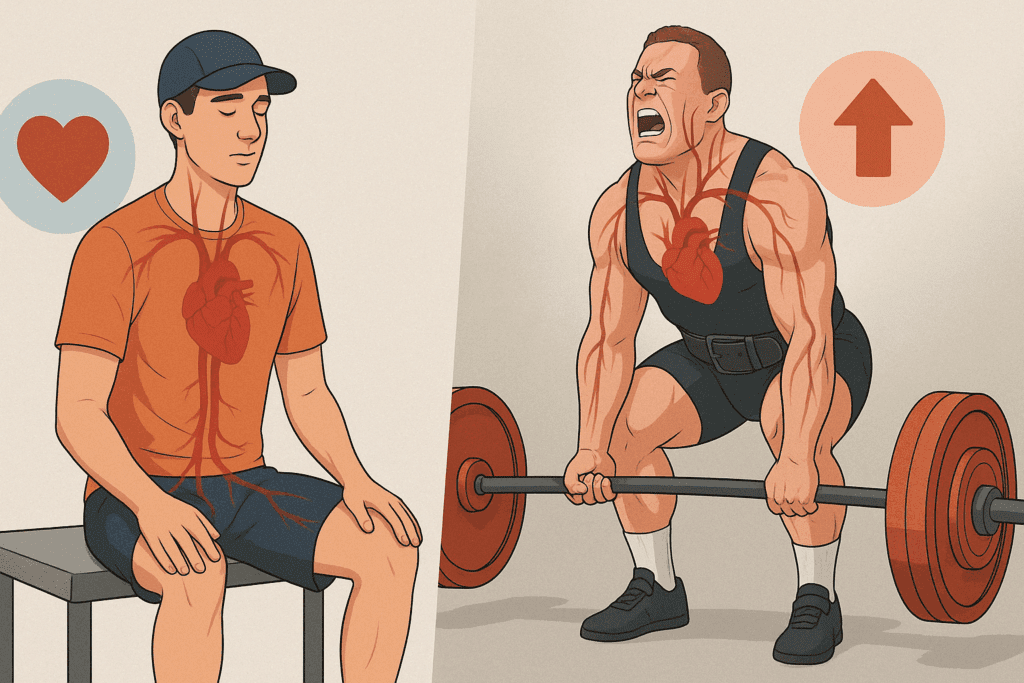
Conversely, strength-based athletes may show higher systolic pressures, particularly during resistance training or heavy lifting. This temporary rise is not necessarily indicative of chronic hypertension but rather reflects the intense physical demands and intrathoracic pressure changes that occur during strength exertion. Even so, repeated exposure to high blood pressure spikes during training must be considered in long-term cardiovascular assessments.
What distinguishes athlete blood pressure further is the recovery rate. Athletes tend to experience quicker normalization of blood pressure post-exercise. This efficient recovery is a marker of cardiovascular resilience and is often used in sports medicine to gauge overall fitness and health status. Therefore, while raw numbers may fluctuate more dramatically in athletes, the context in which these changes occur provides critical insight.
A growing body of evidence also suggests that athletic training alters arterial compliance—the ability of arteries to expand and contract. This flexibility helps buffer sudden changes in blood pressure, allowing athletes to maintain stable perfusion during dynamic activity. Such adaptations may obscure simple comparisons with non-athletes unless interpreted through the lens of sport-specific norms.
Physiological Adaptations: How Training Shapes Blood Pressure
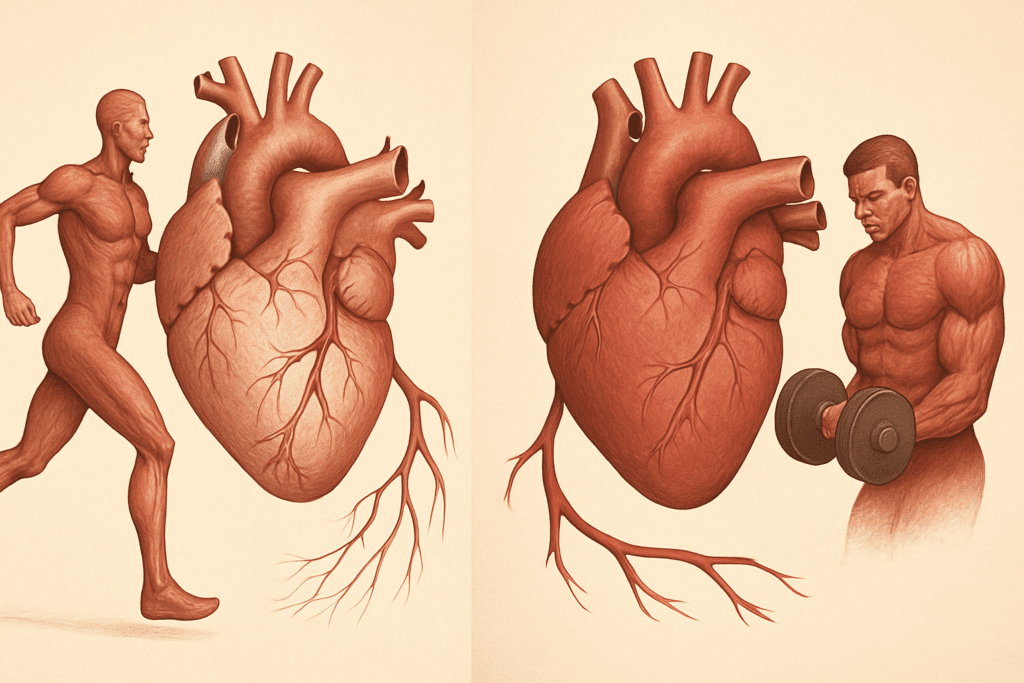
To understand why athlete blood pressure may deviate from typical norms, it’s essential to explore the physiological adaptations induced by sustained training. Endurance exercise, such as cycling or long-distance running, promotes a host of cardiovascular improvements. The heart muscle—particularly the left ventricle—undergoes hypertrophy, increasing stroke volume and reducing the need for high resting heart rates or elevated systolic pressure. This results in a lower resting blood pressure, which is common among endurance athletes.
In contrast, resistance training promotes a different set of adaptations. While not as beneficial for lowering resting blood pressure as endurance exercise, strength training increases peripheral vascular resistance during activity, often producing short-term spikes in systolic pressure. These surges, although temporary, have led researchers to closely monitor high-intensity athletes for early signs of vascular strain.
Importantly, not all blood pressure changes are beneficial. For example, some athletes may develop exercise-induced hypertension—a condition where blood pressure rises excessively during exertion. While this might go unnoticed in casual settings, it could signal an increased risk of long-term cardiovascular issues, even in otherwise fit individuals. This underscores the importance of tailored monitoring and an individualized approach to interpreting blood pressure readings in athletes.
Hormonal regulation also plays a critical role. Physical training influences the renin-angiotensin-aldosterone system (RAAS), which governs fluid balance and blood pressure control. Athletes often show altered RAAS activity, contributing to their unique blood pressure patterns. These changes may persist even during rest and should be considered when comparing athletes to sedentary individuals.
Interpreting Blood Pressure in Athletes: Clinical Considerations
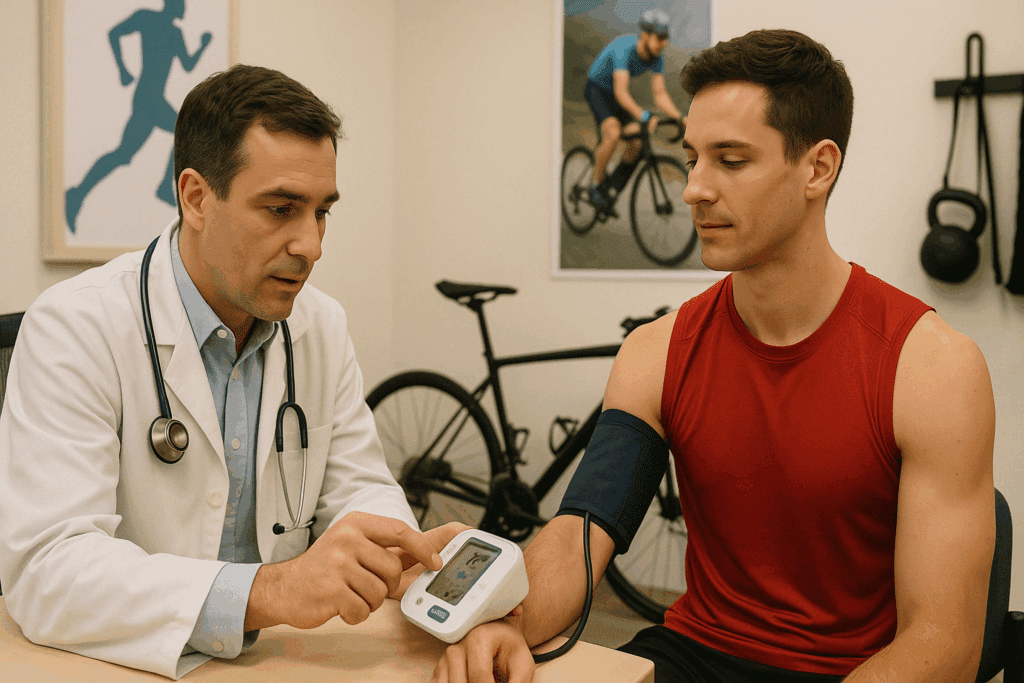
From a clinical perspective, assessing athlete blood pressure requires nuance and expertise. A reading that might be flagged as hypotension in a non-athlete could be entirely normal for a highly conditioned individual. Similarly, a transiently elevated systolic pressure during or immediately after intense training may not indicate a pathology, but rather a typical hemodynamic response to physical stress. Distinguishing between physiological adaptation and pathological deviation is central to proper diagnosis and management.
When evaluating blood pressure in athletes, healthcare providers must consider variables such as sport type, training intensity, age, sex, and genetic predisposition. For example, male athletes often exhibit higher systolic pressure during exertion compared to their female counterparts, owing partly to differences in muscle mass and hormonal profiles. Additionally, adolescent athletes may display transient elevations in blood pressure during growth spurts, which may normalize over time.
Ambulatory blood pressure monitoring (ABPM) is increasingly used to gain a comprehensive view of blood pressure over a 24-hour period. This approach helps detect white coat hypertension—a phenomenon where anxiety during clinical visits causes artificially elevated readings—or masked hypertension, where elevated pressures go unnoticed during routine exams. In athletic populations, ABPM offers a more accurate representation of typical blood pressure behavior, particularly when aligned with training schedules.
Ultimately, understanding athlete blood pressure hinges on context. Rather than applying one-size-fits-all thresholds, clinicians should employ individualized assessments, incorporating fitness level, sport-specific demands, and personal history. Misinterpreting normal athletic adaptations as pathology can lead to unnecessary concern or inappropriate treatment, while overlooking subtle warning signs may delay critical interventions.
The Role of Sports Cardiology: Preventive and Personalized Care
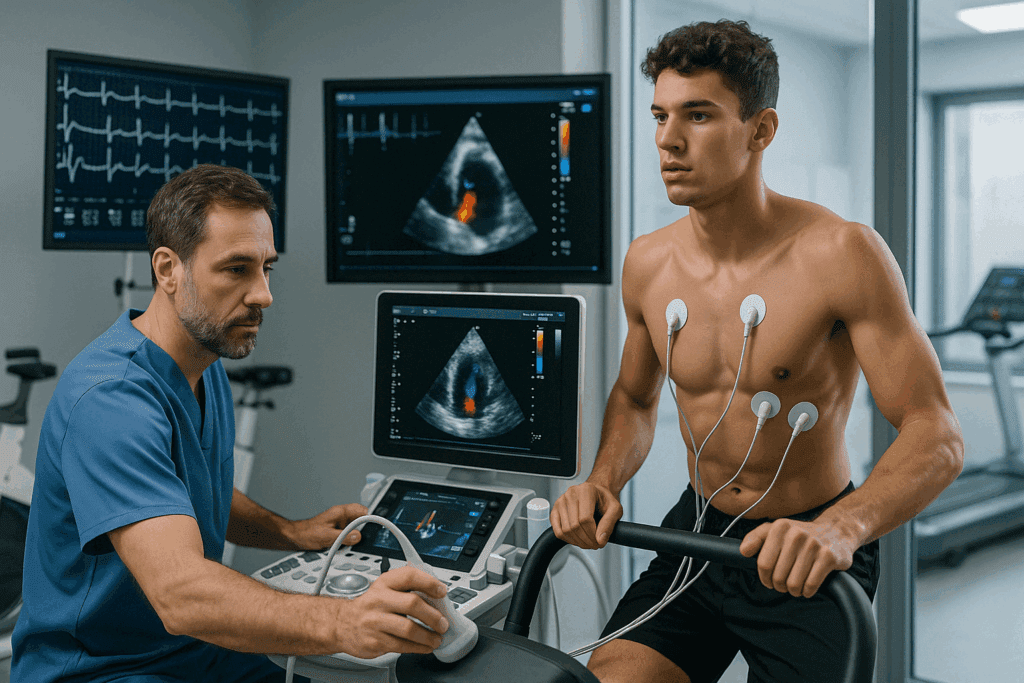
As the intersection of athletics and medicine grows more complex, the role of sports cardiology has become increasingly vital. Sports cardiologists are uniquely equipped to interpret cardiovascular metrics, including blood pressure, within the framework of elite and recreational athletic performance. Their insights help differentiate between benign adaptations and early markers of disease.
One area of focus is the identification of conditions that may elevate cardiovascular risk in athletes, such as hypertrophic cardiomyopathy, congenital heart defects, or arrhythmogenic right ventricular cardiomyopathy. In such cases, blood pressure abnormalities may offer an early clue, prompting deeper diagnostic evaluation. Through echocardiograms, stress tests, and electrocardiograms (ECGs), sports cardiologists can uncover subtle changes that general screening might miss.
Athlete blood pressure is also a factor in return-to-play decisions following injury, illness, or cardiovascular events. Accurate assessment ensures that individuals resume physical activity safely and without undue risk. For instance, after myocarditis—a heart inflammation often triggered by viral infections—monitoring blood pressure response to gradually increasing exertion is critical.
Preventive care in sports cardiology extends beyond elite athletes. Weekend warriors and youth athletes also benefit from expert evaluation, particularly if they exhibit unusual symptoms such as dizziness, palpitations, or unexplained fatigue. Blood pressure that deviates from expectations may be the first indicator that something deeper needs attention.
Importantly, sports cardiology emphasizes education and shared decision-making. Athletes and coaches gain a better understanding of cardiovascular health, enabling informed choices about training intensity, recovery strategies, and when to seek medical consultation. This collaborative approach aligns with the principles of trustworthiness and expertise at the core of the EEAT framework.

Do Athletes Have Different Blood Pressure Across Sports?
A nuanced understanding of athlete blood pressure must also account for the diversity across different sports. Not all athletes are physiologically alike, and the nature of their training imposes distinct cardiovascular demands. For instance, endurance athletes like cyclists and long-distance runners often demonstrate lower resting blood pressure due to high levels of aerobic conditioning. These individuals benefit from enhanced arterial compliance and reduced peripheral resistance.
In contrast, power-based sports such as sprinting, football, and weightlifting place acute stress on the cardiovascular system, often leading to transient elevations in systolic blood pressure during performance. Over time, the repetitive nature of these pressure surges may contribute to different cardiovascular remodeling compared to endurance athletes. However, resting blood pressure in strength-trained individuals may still fall within normal limits, provided they are in good health.
Combat sports and mixed-modal disciplines like CrossFit or wrestling introduce an additional layer of complexity. These athletes often experience fluctuations in blood pressure due to dehydration, weight cycling, and sympathetic nervous system activation. Monitoring becomes especially important in these populations to distinguish between adaptive responses and red flags for potential cardiovascular risk.
Even within team sports, positional roles can influence cardiovascular profiles. A soccer midfielder covering significant ground may have a different hemodynamic profile than a goalkeeper who exerts in bursts. Understanding the specific demands of a sport—and even a position—can enhance the precision of blood pressure interpretation and improve athlete care.
Addressing Misconceptions: Athlete Health Isn’t Always Perfect
Despite the perception that athletes epitomize health, they are not immune to cardiovascular issues. In some cases, intense training can unmask underlying conditions or even contribute to vascular strain if recovery and monitoring are inadequate. Elevated blood pressure, even in the fittest individuals, warrants attention when it persists outside of expected ranges or presents alongside other symptoms.
One common misconception is that low resting blood pressure in athletes is always beneficial. While it often reflects high cardiovascular efficiency, excessively low readings may be associated with dizziness, fatigue, or poor perfusion—particularly during periods of dehydration or illness. Identifying the threshold where low pressure becomes problematic is key to comprehensive care.
Another area of concern is overtraining syndrome. This condition, characterized by prolonged fatigue, performance decline, and altered physiological markers, can include abnormal blood pressure responses. In these cases, the body’s usual homeostatic mechanisms become dysregulated, reinforcing the importance of monitoring both during and outside of training periods.
Understanding that athlete blood pressure exists on a spectrum—and that even optimal physical conditioning does not guarantee immunity from cardiovascular risk—is crucial. Encouraging athletes to view health as a multifactorial, dynamic process rather than a binary outcome fosters a more realistic and proactive mindset.
Frequently Asked Questions: Understanding Athlete Blood Pressure and Cardiovascular Health
1. Can stress impact athlete blood pressure even if the athlete is physically fit?
Absolutely. While physical fitness provides numerous cardiovascular benefits, stress—whether psychological, emotional, or situational—can elevate blood pressure even in athletes. Competitive stress, performance anxiety, or lifestyle pressures outside of training can activate the sympathetic nervous system, leading to increased heart rate and vascular resistance. Unlike exercise-induced changes, stress-related elevations are less predictable and can persist longer, particularly if recovery protocols are inadequate. This suggests that even those with optimized athlete blood pressure may benefit from mindfulness training, therapy, or relaxation techniques to maintain holistic cardiovascular health.
2. How do sleep quality and circadian rhythms influence athlete blood pressure patterns?
Athlete blood pressure can vary significantly based on sleep quality and circadian alignment. Athletes with disrupted sleep—common during travel, competitions, or overtraining—may exhibit elevated nocturnal blood pressure or a blunted dipping pattern, which typically helps regulate cardiovascular load during rest. Chronobiological disruptions may also impair hormonal rhythms involved in blood pressure regulation, such as cortisol and melatonin. As such, prioritizing sleep hygiene and maintaining consistent sleep-wake cycles is essential for supporting optimal athlete blood pressure and overall cardiovascular stability.
3. Are wearable technologies reliable for monitoring athlete blood pressure trends?
Consumer-grade wearables are improving, but their ability to track athlete blood pressure with medical-grade accuracy remains limited. While they may provide general trends and help detect patterns over time, they are not substitutes for validated, clinically approved devices, particularly in diagnosing conditions like masked or white-coat hypertension. However, when used alongside professional assessments, wearables can help athletes track recovery, hydration status, and post-exercise recovery trends. For those questioning, “do athletes have different blood pressure throughout the day?”—these devices can provide insightful, albeit approximate, data on daily fluctuations and help tailor training accordingly.
4. How does altitude training affect athlete blood pressure in the short and long term?
Training at high altitudes triggers a series of physiological responses that may initially elevate blood pressure due to increased sympathetic nervous system activation and lower oxygen availability. Over time, however, acclimatization leads to enhanced red blood cell production and improved oxygen efficiency, potentially resulting in normalized or even reduced resting pressures. These adaptations can vary between individuals, and it’s not uncommon for athletes to experience transient hypertension during early phases of altitude exposure. Understanding how altitude alters athlete blood pressure dynamics is crucial for preventing complications during both training and competition.
5. Could hydration status cause misleading athlete blood pressure readings?
Yes, hydration plays a significant role in the accuracy of athlete blood pressure measurements. Dehydration, which is common during prolonged or high-intensity workouts, can cause blood pressure to drop acutely or fluctuate inconsistently. Conversely, overhydration without proper electrolyte balance may dilute sodium levels, impacting blood pressure regulation and cardiovascular performance. For athletes who wonder, “do athletes have different blood pressure during competition versus recovery?”—hydration may be a major variable influencing that distinction. Maintaining electrolyte balance and consistent fluid intake is therefore critical for both performance and accurate blood pressure monitoring.
6. Are there differences in athlete blood pressure across different age groups?
Indeed, age influences how the cardiovascular system responds to training and affects the baseline and reactive measures of blood pressure. Younger athletes generally exhibit greater arterial elasticity and more pronounced recovery patterns after exertion, which can help maintain lower resting blood pressure. As athletes age, arterial stiffness may increase slightly, and recovery times may lengthen, subtly altering their blood pressure profiles even if overall fitness remains high. This underscores why age-specific evaluations are necessary when addressing athlete blood pressure and emphasizes the importance of longitudinal health tracking.
7. What role does menstrual cycle phase play in female athlete blood pressure readings?
Hormonal fluctuations throughout the menstrual cycle can impact vascular tone, fluid retention, and overall cardiovascular reactivity. During the luteal phase, for instance, progesterone-driven fluid shifts can result in slightly elevated blood pressure in some women. Female athletes who track their cycles often observe these variations and can adjust training load or recovery strategies accordingly. Understanding that athlete blood pressure may change subtly with hormonal phases helps normalize these shifts and supports a more personalized, physiology-informed approach to training.
8. Can nutrition strategies directly influence athlete blood pressure control?
Nutrition is a foundational pillar of cardiovascular regulation. Diets rich in potassium, magnesium, and antioxidants—such as those found in leafy greens, berries, and legumes—support vascular health and help maintain normal blood pressure levels in athletes. In contrast, excessive sodium intake, particularly from processed sports snacks or recovery drinks, can elevate pressure unnecessarily. Athletes often require tailored nutrition plans that consider not only performance but also long-term cardiovascular effects. A key question, “do athletes have different blood pressure due to dietary habits?” often points to the interplay between sport-specific fueling strategies and individual metabolic responses.
9. How do genetics influence variations in athlete blood pressure?
Genetic predispositions can significantly impact how an athlete’s cardiovascular system responds to training. Some individuals naturally have lower or higher baseline pressures due to inherited factors, regardless of fitness level. Genetic variations in enzymes like ACE (angiotensin-converting enzyme) or genes affecting nitric oxide production can shape an athlete’s capacity for vasodilation and blood pressure regulation. This highlights why athlete blood pressure should never be assessed in isolation—personal and family history must be included to create a complete picture of cardiovascular health. Genetic testing, though not yet mainstream, is becoming more accessible and may soon play a bigger role in athletic cardiovascular screening.
10. What future innovations might improve athlete blood pressure monitoring and management?
Emerging technologies, including AI-powered diagnostics and smart textiles, promise more accurate, real-time monitoring of blood pressure in athletic settings. These tools could help distinguish between normal training responses and early signs of overtraining or cardiovascular dysfunction. Furthermore, digital platforms may integrate multiple data streams—such as sleep, hydration, and heart rate variability—to offer a more comprehensive view of athlete health. As we continue exploring questions like “do athletes have different blood pressure profiles based on training type or recovery mode?”—technology will likely play a central role in uncovering individualized patterns and optimizing performance safely.
Conclusion: Interpreting Athlete Blood Pressure for Long-Term Cardiovascular Health
The question “do athletes have different blood pressure?” cannot be answered with a simple yes or no. Instead, it invites a deeper appreciation of how athletic training molds cardiovascular physiology, often resulting in blood pressure readings that deviate from general norms yet remain healthy within the context of performance and adaptation. Athlete blood pressure reflects a complex interplay between sport-specific demands, training intensity, genetic predisposition, and individual health status.
Clinicians, athletes, and sports professionals alike must move beyond rigid benchmarks and embrace a more nuanced, personalized approach to cardiovascular monitoring. By recognizing the spectrum of normal within athletic populations, avoiding misdiagnosis, and appreciating the unique physiological profiles that athletes present, we can better support long-term health and performance.
With an emphasis on evidence-based evaluation, preventive screening, and individualized care, the field of sports cardiology continues to play a vital role in advancing our understanding of athlete blood pressure. In doing so, it reinforces the core principles of EEAT—Experience, Expertise, Authoritativeness, and Trustworthiness—while ensuring that athletes of all levels can safely pursue their goals with clarity and confidence.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Athletes and Blood Pressure: Insights into Hypertension Risks and Prevention


