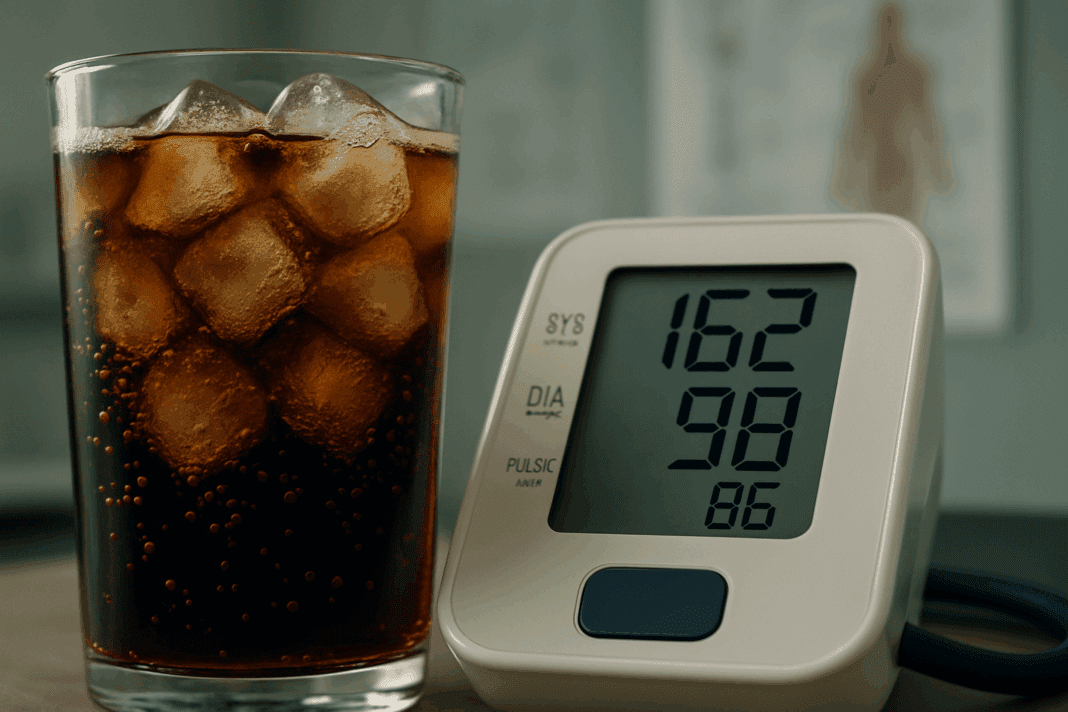
Understanding the link between dietary choices and cardiovascular health has become increasingly important as rates of hypertension and heart disease continue to rise globally. Among the many contributors to elevated blood pressure, the role of sugar-sweetened beverages and caffeinated sodas has generated considerable debate within both the medical community and the general public. Questions such as “does soda raise blood pressure?” or “is Pepsi bad for blood pressure?” are now frequently searched online by health-conscious individuals looking to make informed choices. These questions are not only valid but also grounded in a growing body of scientific literature that examines how soda consumption may influence blood pressure and overall heart health.
The modern diet, particularly in Western societies, is inundated with ultra-processed foods and sugary drinks that deliver high levels of calories with minimal nutritional value. Carbonated soft drinks, including those produced by major brands like Pepsi, have been scrutinized for their potential role in exacerbating chronic diseases, including hypertension. Caffeine, high fructose corn syrup, sodium, and phosphoric acid are just a few of the components in many sodas that may contribute to increased cardiovascular risk. Understanding the cumulative and individual impact of these ingredients can provide clearer insight into whether regular soda consumption poses a significant threat to blood pressure regulation.
To unpack the science behind these concerns, it is essential to explore the mechanisms through which soda may influence blood pressure, examine empirical research findings, and consider individual variability in response to these beverages. By doing so, this article aims to provide a balanced, evidence-based examination of the question: does soda raise blood pressure?
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
The Composition of Soda and Its Physiological Impact
Soda is more than just a fizzy refreshment—it is a complex concoction of chemical ingredients designed to stimulate the senses. Most commercially available sodas, including Pepsi and other cola beverages, contain high levels of added sugars, often in the form of high fructose corn syrup or sucrose. These sugars are quickly absorbed by the body and can lead to spikes in blood glucose and insulin levels. Over time, chronic consumption of high-sugar beverages has been associated with insulin resistance, weight gain, and metabolic syndrome, all of which are significant risk factors for elevated blood pressure.
In addition to sugars, caffeine is a central component in many sodas. While caffeine in moderate doses has been shown to have both beneficial and adverse effects, excessive intake may contribute to short-term increases in blood pressure, particularly among individuals who are sensitive to its effects. The presence of sodium and phosphoric acid in soda formulations can further complicate matters. Sodium can influence fluid retention and vascular resistance, while phosphoric acid has been linked to decreased bone mineral density and potential alterations in calcium metabolism—factors that indirectly affect cardiovascular health.
Artificial flavorings, preservatives, and colorants—often overlooked—may also exert subtle physiological effects, particularly when consumed in high quantities. Though these additives are generally recognized as safe by regulatory agencies, emerging research suggests they may disrupt the gut microbiome or induce low-grade inflammation, both of which have been implicated in the development of hypertension. Taken together, these components suggest that soda is not an innocuous indulgence but rather a beverage with the potential to disrupt several pathways related to cardiovascular regulation.
Epidemiological Evidence Linking Soda Consumption to Hypertension
Numerous population-based studies have investigated the correlation between soda intake and the incidence of high blood pressure. A landmark study published in the journal Hypertension found that individuals who consumed more than one sugar-sweetened beverage per day had a significantly higher risk of developing hypertension compared to those who consumed none. The association persisted even after adjusting for other risk factors such as BMI, physical activity, and overall caloric intake.
In another large-scale cohort study conducted by the Nurses’ Health Study and Health Professionals Follow-Up Study, researchers observed a consistent relationship between sugar-sweetened beverage consumption and increased systolic and diastolic blood pressure. These findings were further supported by meta-analyses that pooled data from multiple studies, showing a dose-response relationship: the more soda individuals consumed, the greater their risk of hypertension.
While observational studies cannot establish causation, they provide strong circumstantial evidence that warrants further investigation. Notably, studies have differentiated between regular and diet sodas, with some indicating that even artificially sweetened sodas may contribute to elevated blood pressure through mechanisms not yet fully understood. This suggests that the metabolic effects of soda extend beyond its sugar content alone, adding complexity to the question: is Pepsi bad for blood pressure?
The Role of Caffeine and Sugar in Blood Pressure Regulation
Caffeine, a natural stimulant found in many sodas, has a well-documented but nuanced effect on blood pressure. Acute ingestion of caffeine can cause a temporary spike in both systolic and diastolic pressure by stimulating the sympathetic nervous system and increasing heart rate. For habitual caffeine users, however, tolerance often develops, diminishing this response over time. Still, in individuals with preexisting hypertension or caffeine sensitivity, even modest doses may exacerbate blood pressure elevations.
Sugar, particularly in the form of high fructose corn syrup, is perhaps an even more critical factor. Fructose metabolism has been shown to increase uric acid levels, which in turn can impair endothelial function and promote vasoconstriction. This chain reaction may contribute to increased systemic vascular resistance and elevated blood pressure. Additionally, high sugar intake contributes to weight gain and visceral adiposity, both of which are strongly linked to hypertension.
Studies in adolescents and young adults have revealed that early exposure to sugar-laden beverages may predispose individuals to hypertension later in life. This is especially concerning given the aggressive marketing of soda to younger demographics and the habitual nature of soda consumption once established. As such, the question “does soda raise blood pressure?” becomes particularly relevant when considering long-term public health implications.
Pepsi and Other Colas: Are Some Brands Worse Than Others?
While Pepsi often serves as a stand-in for soda in general discussions, it is worth examining whether specific brands differ significantly in their health impact. Pepsi contains caffeine, high fructose corn syrup, phosphoric acid, and various artificial ingredients, placing it firmly within the category of sugar-sweetened, caffeinated soft drinks. The question “is Pepsi bad for blood pressure?” is valid, given the beverage’s formulation and the established effects of its ingredients.
That said, comparative analyses of different soda brands reveal that most popular colas share a similar ingredient profile, though caffeine and sugar content may vary slightly. Some studies suggest that dark colas, which contain phosphoric acid, may pose additional risks compared to lighter sodas due to potential impacts on mineral metabolism. Furthermore, sodas marketed as “energy” drinks may contain higher concentrations of caffeine and added stimulants, which could exacerbate blood pressure elevations more than traditional colas.
Ultimately, the brand itself may be less important than the category of beverage. Whether it is Pepsi, Coca-Cola, or a generic store-brand cola, the combination of sugar, caffeine, and artificial additives presents a similar set of cardiovascular risks. The frequency and volume of consumption are far more influential in determining health outcomes than brand loyalty or flavor preference.

Individual Variability in Response to Soda Intake
Not all individuals respond to soda consumption in the same way. Genetic predisposition, metabolic profile, age, and existing medical conditions all influence how the body processes the components of soda. For example, some individuals may have genetic variants that affect caffeine metabolism, making them more susceptible to its hypertensive effects. Others may have insulin resistance or metabolic syndrome, amplifying the negative consequences of sugar intake.
Lifestyle factors such as physical activity, dietary patterns, and stress levels also modulate the impact of soda on blood pressure. An active individual with a balanced diet and healthy weight may experience fewer adverse effects from occasional soda consumption compared to someone who is sedentary, overweight, and has a high-sodium, high-fat diet. Nonetheless, even among seemingly healthy individuals, regular soda intake can subtly contribute to long-term cardiovascular strain.
Furthermore, medication interactions must be considered. Some blood pressure medications may be less effective when combined with high-caffeine or high-sodium diets. Diuretics, for instance, may interact negatively with the sodium content in certain sodas, reducing therapeutic efficacy. Therefore, healthcare providers often advise patients with hypertension to limit or avoid soda as part of a comprehensive treatment plan.
Public Health Recommendations and Preventive Strategies
Given the mounting evidence linking soda consumption to elevated blood pressure, many public health organizations have issued guidelines aimed at reducing intake of sugar-sweetened beverages. The American Heart Association recommends limiting added sugar intake to no more than 25 grams per day for women and 36 grams for men—a threshold easily exceeded by a single can of soda. These recommendations are not arbitrary; they are grounded in evidence showing that even modest reductions in sugar and caffeine intake can lead to measurable improvements in blood pressure and overall cardiovascular health.
Preventive strategies extend beyond individual behavior and encompass broader policy initiatives. Taxation of sugar-sweetened beverages, improved labeling, school-based nutrition education, and restrictions on marketing to children are all tools that can help reduce soda consumption at the population level. Additionally, promoting access to healthier beverage alternatives such as water, herbal teas, and low-sugar juices can provide practical options for those seeking to cut back without sacrificing hydration or flavor.
Healthcare professionals play a crucial role in these efforts by educating patients about the risks associated with soda consumption and providing personalized guidance based on individual health status. For those already diagnosed with hypertension or at high risk, reducing or eliminating soda intake should be a priority alongside other lifestyle modifications such as increasing physical activity, reducing sodium intake, and managing stress.
FAQ: The Impact of Soda on Blood Pressure
1. Can drinking soda occasionally still affect blood pressure?
Even occasional soda consumption may impact blood pressure, particularly for individuals who are genetically predisposed to hypertension or have pre-existing cardiovascular risk factors. While a single can of soda may not trigger an immediate crisis, its high sugar and caffeine content can temporarily raise blood pressure through mechanisms such as increased heart rate and vasoconstriction. More importantly, occasional indulgence can lead to recurring habits that normalize soda intake over time. For those wondering, does soda raise blood pressure even when consumed sporadically, the answer depends largely on personal health context and overall dietary habits. It’s not just about frequency—it’s about cumulative effects and biological sensitivity to soda’s ingredients.
2. Is Pepsi worse for blood pressure than other sodas?
The question is Pepsi bad for blood pressure invites a closer look at the specific ingredients in Pepsi compared to other brands. While most mainstream colas contain similar amounts of caffeine, sugar, and phosphoric acid, some formulations differ slightly in sodium levels and sweetener types. Pepsi, for instance, contains high fructose corn syrup and caffeine, both known to influence cardiovascular function. Individuals with high caffeine sensitivity or metabolic conditions might experience a more pronounced blood pressure response with Pepsi than with a caffeine-free alternative. Ultimately, it’s the combination of ingredients—and their synergy with individual physiology—that determines the degree of impact.
3. Can soda consumption in children lead to high blood pressure later in life?
There is growing concern that early soda exposure may predispose children to hypertension and metabolic syndrome in adulthood. Studies suggest that high sugar intake in youth can lead to insulin resistance, inflammation, and weight gain—each of which contributes to long-term blood pressure dysregulation. Furthermore, the habitual nature of sugary drink consumption means that soda often becomes a lifelong dietary staple. The question of does soda raise blood pressure becomes even more significant when framed as a developmental issue, where early habits set the stage for chronic health outcomes. Encouraging water and natural alternatives from a young age may serve as a critical preventive strategy.
4. How does caffeine-free soda compare to regular soda in terms of blood pressure effects?
Caffeine-free soda removes one variable in the complex equation of soda’s cardiovascular impact, but it does not eliminate all risks. Sugar remains a dominant concern, especially when present in large amounts, as it can still raise insulin and uric acid levels—both implicated in increased blood pressure. Additionally, some caffeine-free sodas contain artificial sweeteners, the long-term effects of which are still under investigation. For individuals asking whether is Pepsi bad for blood pressure if it’s caffeine-free, the answer remains nuanced. While it may be slightly less stimulatory, the metabolic consequences of excess sugar remain problematic.
5. Do diet sodas have the same impact on blood pressure as regular sodas?
The debate over diet sodas and blood pressure is ongoing, with studies producing mixed findings. While diet sodas eliminate sugar, some research indicates that artificial sweeteners may affect insulin response and gut microbiota, potentially influencing blood pressure regulation indirectly. There’s also the psychological component—many people compensate for calorie-free drinks by consuming more unhealthy foods, negating any cardiovascular benefit. So while one might assume that switching from Pepsi to diet Pepsi mitigates risk, the question is Pepsi bad for blood pressure doesn’t become irrelevant—it simply shifts focus to different ingredients with their own set of implications. Long-term studies are still needed to draw definitive conclusions.
6. How does soda consumption interact with stress-related blood pressure changes?
Stress and soda can form a dangerous synergy when it comes to blood pressure. Elevated cortisol from chronic stress can already predispose individuals to higher blood pressure; adding stimulants like caffeine or sugar from soda can compound this effect. Moreover, people under stress may be more likely to reach for comfort drinks like soda, turning an emotional response into a physiological feedback loop. For individuals asking does soda raise blood pressure during stressful periods, the answer is particularly affirmative, as soda can amplify the body’s sympathetic nervous system response. Healthier coping mechanisms, such as herbal teas or mindfulness practices, are preferable alternatives.
7. What role does hydration play in mitigating the blood pressure effects of soda?
Proper hydration with water can help counteract some of the dehydrating effects of caffeine and sodium found in soda. When the body is well-hydrated, blood viscosity decreases, and vascular function improves, potentially lessening soda’s short-term impact on blood pressure. However, hydration should not be viewed as a remedy for habitual soda consumption. Asking does soda raise blood pressure cannot be answered away by simply drinking more water; the underlying metabolic effects of sugar and additives persist regardless. Still, maintaining hydration is a supportive measure that complements broader dietary changes.
8. Can quitting soda lead to noticeable improvements in blood pressure?
Yes, many individuals experience meaningful reductions in blood pressure after cutting out soda, especially when they replace it with healthier options like water, herbal teas, or unsweetened beverages. These improvements often occur alongside weight loss, reduced sugar intake, and better insulin sensitivity. For someone questioning is Pepsi bad for blood pressure, personal experience after cessation can be eye-opening. Beyond numbers on a monitor, people often report feeling less jittery, more mentally clear, and less prone to sugar cravings. It’s a holistic benefit that spans physical and psychological well-being.
9. Are there cultural or socioeconomic factors that influence soda-related blood pressure risks?
Access to health education, clean water, and nutritious food plays a significant role in dietary habits, including soda consumption. In communities where healthier beverages are expensive or unavailable, soda often becomes a default choice. Marketing efforts also disproportionately target certain demographics, compounding the challenge. For individuals in these settings, asking does soda raise blood pressure is more than a health inquiry—it becomes a reflection of broader systemic issues. Public health policies that address access and education can help mitigate the risks linked to soda in vulnerable populations.
10. What innovations are emerging in beverage alternatives to reduce blood pressure risk?
As awareness grows about the health effects of soda, new beverage options are emerging that aim to offer flavor without the negative cardiovascular consequences. Functional drinks containing adaptogens, magnesium, electrolytes, or plant-based antioxidants are gaining popularity. These drinks not only hydrate but may support relaxation and blood pressure regulation. For those seeking to transition away from soda but still crave carbonation and taste, these alternatives can serve as a bridge. By choosing smartly, people who wonder is Pepsi bad for blood pressure can shift toward beverages that support—not sabotage—their cardiovascular health.
Conclusion: Reassessing Soda’s Role in Cardiovascular Health
In addressing the question “does soda raise blood pressure?” the scientific consensus points toward a cautious but affirmative answer. While the relationship is complex and influenced by multiple variables, the evidence overwhelmingly suggests that regular consumption of soda—particularly those high in sugar and caffeine—can contribute to elevated blood pressure and increased cardiovascular risk. This conclusion is especially pertinent when examining widely consumed products such as Pepsi, leading many to reasonably ask, “is Pepsi bad for blood pressure?”
Although individual responses to soda may vary based on genetic, metabolic, and lifestyle factors, the cumulative impact of frequent consumption is difficult to ignore. The combination of high fructose corn syrup, caffeine, sodium, and artificial additives creates a metabolic environment that is not conducive to optimal blood pressure regulation. Over time, even moderate intake can subtly erode cardiovascular resilience, particularly in vulnerable populations.
For consumers seeking to protect their heart health, the most prudent course of action is to reduce or eliminate soda from the diet and replace it with healthier alternatives. Water, herbal infusions, and nutrient-rich smoothies offer hydration without the drawbacks associated with sugary, caffeinated beverages. As public awareness continues to grow, so too does the potential for meaningful change in dietary habits and health outcomes.
Ultimately, making informed decisions about beverage choices is a small but significant step toward achieving long-term cardiovascular wellness. By understanding the science and respecting the signals from our own bodies, we can navigate the beverage aisle with greater confidence and make choices that truly support our health and vitality.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Drinking 2 servings of sugary drinks like soda per week may harm heart health