The relationship between sunlight and eczema has long intrigued both dermatologists and patients alike. While traditional treatment methods often rely on topical steroids, antihistamines, and lifestyle modifications, growing interest has emerged around the question: does sunlight help eczema? With the rise in interest toward natural and non-pharmacological approaches, sunlight exposure has become a subject of scientific inquiry and practical relevance. This article delves into the complex connection between eczema and ultraviolet (UV) light, shedding light on its benefits, limitations, and the safest ways to incorporate sun exposure into a comprehensive eczema management plan.
You may also like: Breakthrough Approaches to Eczema Alternative Healing: What Works and Why It Matters
Understanding Eczema: Causes, Symptoms, and Mechanisms
To appreciate the role of sunlight in eczema treatment, one must first understand the underlying nature of the condition. Eczema, also known as atopic dermatitis, is a chronic inflammatory skin disease that affects millions of individuals worldwide. It is characterized by itchy, red, and often scaly patches of skin that may crack or ooze when scratched. Eczema typically follows a relapsing-remitting course, meaning that flare-ups can be triggered by environmental factors, allergens, stress, hormonal changes, or irritants.
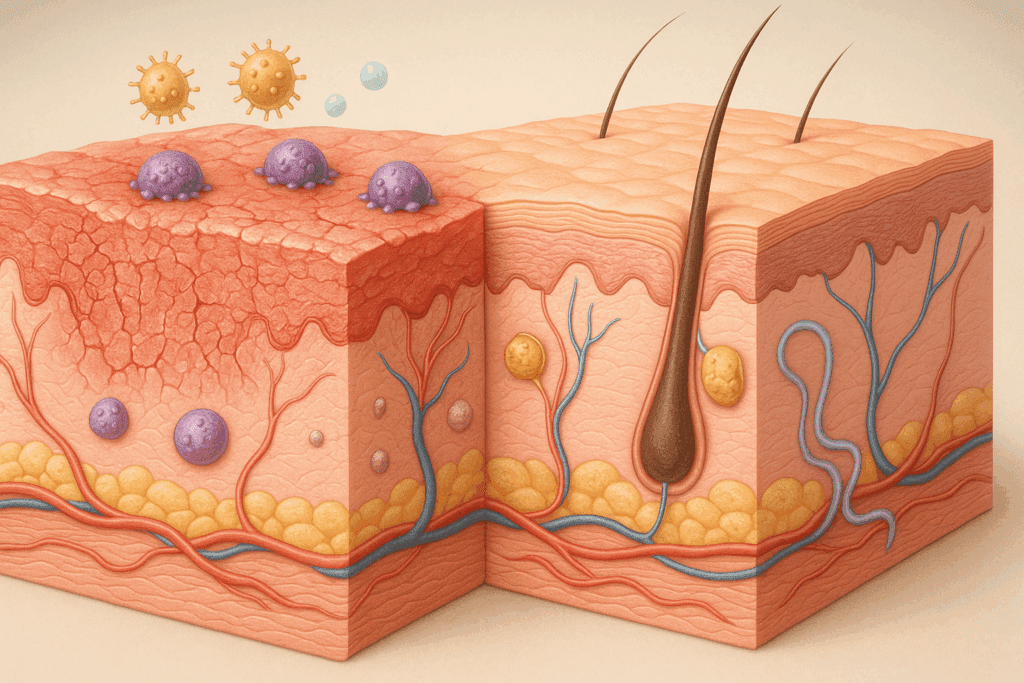
At a biological level, eczema is driven by a combination of genetic, immunological, and environmental elements. Individuals with eczema often have a compromised skin barrier, allowing allergens and microbes to penetrate more easily and activate an exaggerated immune response. The immune system in eczema patients is often skewed toward a Th2-dominant response, which amplifies inflammation and contributes to symptoms. This immunological dysfunction, in tandem with environmental stimuli, is what perpetuates the vicious cycle of flare-ups.
Historical and Modern Perspectives on Sunlight and Skin Health
Sunlight has played a role in skin therapy for centuries. Ancient civilizations, including the Egyptians and Greeks, recognized the healing properties of sunlight and incorporated it into their medical practices. The concept of heliotherapy—the therapeutic use of natural sunlight—gained popularity in the 19th century and was notably used in treating skin conditions like psoriasis and tuberculosis-related skin lesions.
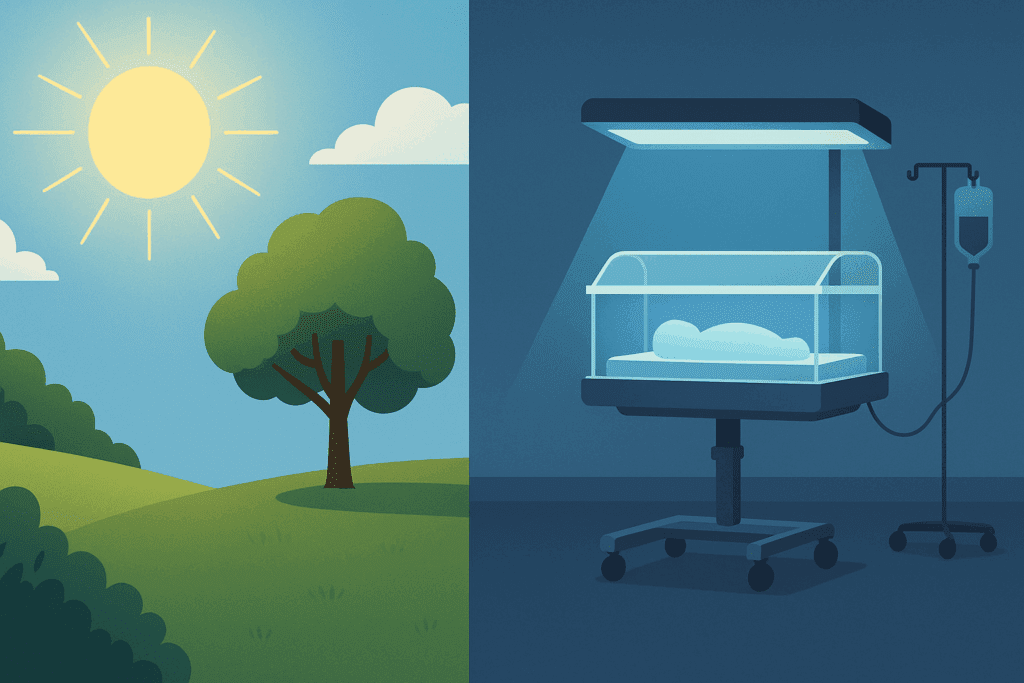
In the modern era, the role of sunlight in dermatology has been formalized through the development of phototherapy. Phototherapy involves controlled exposure to UVB or UVA light under medical supervision and is a standard treatment for severe or refractory eczema. This evolution in practice has contributed to the renewed interest in natural sunlight exposure, as many wonder whether time outdoors can mimic the controlled effects of phototherapy. Therefore, the question “does sunlight help eczema?” is not merely anecdotal but grounded in longstanding therapeutic traditions.
Does Sunlight Help Eczema? Evidence from Clinical and Observational Studies
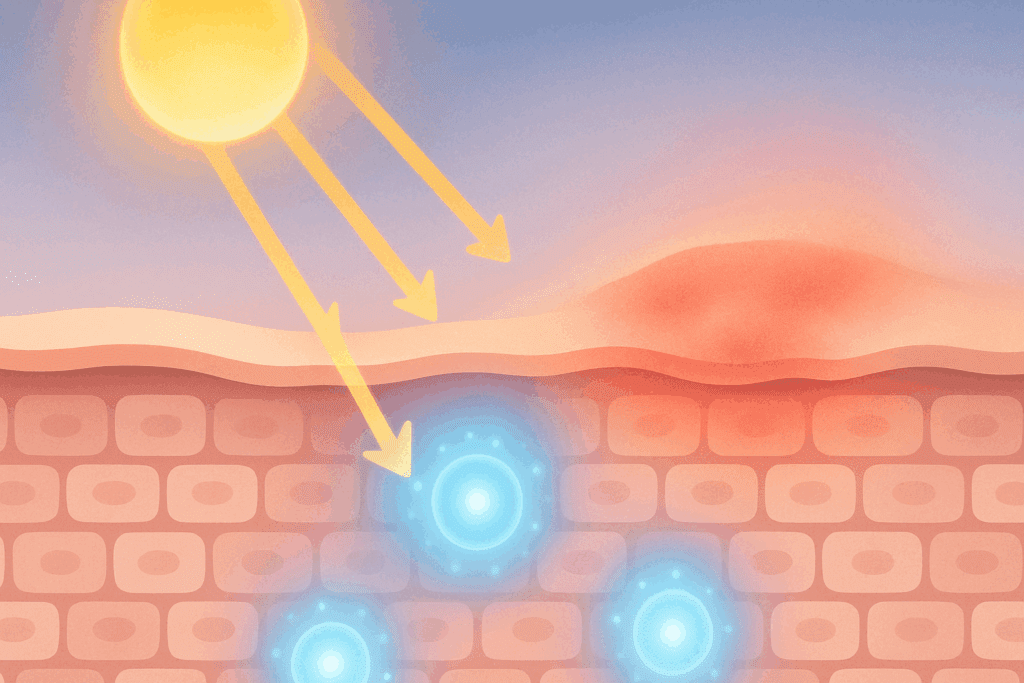
Several studies have addressed the potential benefits of sunlight on eczema symptoms. Controlled clinical trials and observational studies alike suggest that limited exposure to natural sunlight can yield therapeutic effects for some individuals with eczema. The UVB component of sunlight, in particular, has been shown to modulate immune responses in the skin, reducing the activity of overactive T-cells and decreasing inflammation.
One clinical trial published in the Journal of the American Academy of Dermatology found that narrowband UVB phototherapy significantly improved eczema symptoms in adults and children with moderate to severe atopic dermatitis. Although this form of UVB exposure is more precise than sunlight, the findings support the idea that UVB light—which is also present in sunlight—can provide relief from eczema.
Moreover, observational studies conducted in various geographical regions have noted that individuals with eczema often experience seasonal improvements in symptoms during sunnier months. While other factors like humidity and outdoor activity levels may also contribute, the consistency of these findings across diverse populations lends credence to the notion that sunlight plays a beneficial role. Thus, answering the query, “does sun help eczema?” leads us to cautiously affirm its potential, provided exposure is moderate and medically guided.
How Sunlight Affects the Skin’s Immune and Barrier Function
To understand why sunlight may alleviate eczema, it is essential to examine how UV radiation interacts with the skin. UVB light, in particular, penetrates the epidermis and modulates the immune system by suppressing inflammatory pathways. It reduces the proliferation of Langerhans cells and decreases the expression of pro-inflammatory cytokines, both of which are implicated in eczema pathogenesis.
In addition to its immunomodulatory effects, sunlight may aid in repairing the skin barrier. Controlled UV exposure can stimulate the production of antimicrobial peptides and ceramides, which are crucial for maintaining skin hydration and resilience. By strengthening the barrier function, sunlight may reduce trans-epidermal water loss and prevent allergens from triggering flare-ups.
Furthermore, the sun is a natural source of vitamin D, which plays a pivotal role in immune regulation and skin health. Low levels of vitamin D have been associated with increased eczema severity, and supplementation has shown promise in reducing flare-ups. Although more research is needed, the synergy between UV-induced vitamin D synthesis and immune modulation provides a plausible mechanism through which sunlight can benefit eczema.
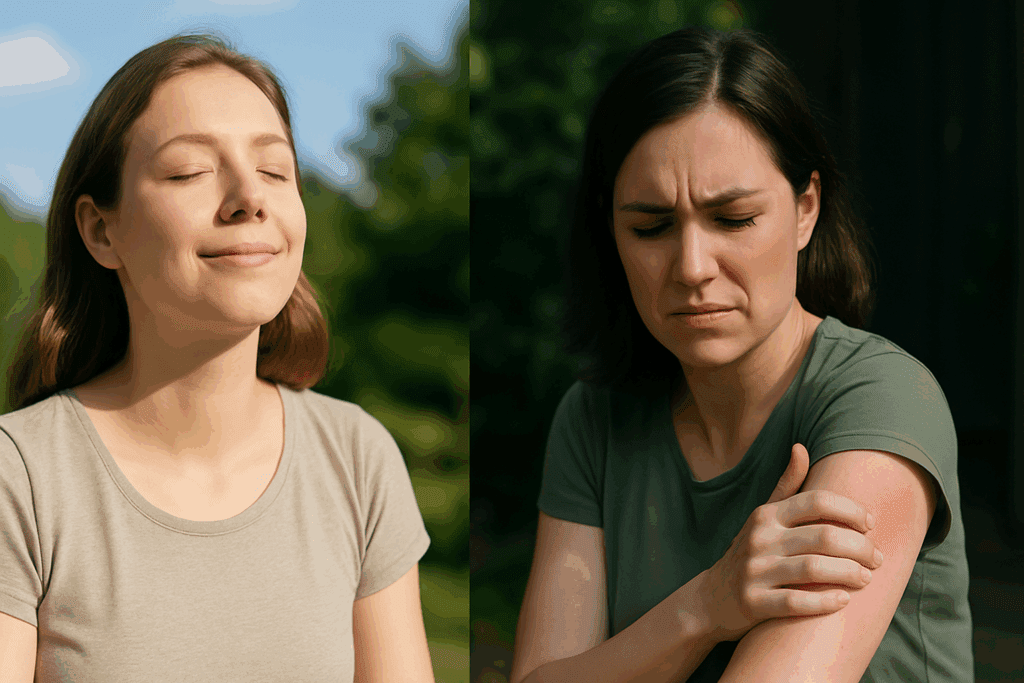
Is Sun Good for Eczema All the Time? Understanding Individual Variability
Despite the potential benefits, not all eczema patients respond to sunlight in the same way. For some individuals, especially those with sun-sensitive skin types or certain genetic predispositions, sunlight can act as a trigger rather than a remedy. A condition known as “sun eczema” or polymorphic light eruption (PMLE) can mimic or exacerbate atopic dermatitis, especially after sudden or intense sun exposure.
In such cases, the immune response to UV radiation becomes exaggerated, leading to itchy, red, and inflamed skin. This paradoxical reaction highlights the importance of personalized treatment strategies. Individuals with a history of photosensitivity or those on medications that increase sun sensitivity should consult a dermatologist before using sunlight therapeutically.
Additionally, excessive sun exposure can lead to sunburn, hyperpigmentation, and long-term risks such as skin cancer and photoaging. These risks underscore the importance of moderation and protection when using sunlight as part of eczema management. Protective strategies include timing sun exposure during low UV index hours, wearing hats and clothing, and using non-irritating mineral-based sunscreens on unaffected areas.
Natural Sunlight Versus Phototherapy: Weighing the Pros and Cons
A crucial distinction must be made between natural sunlight and medically supervised phototherapy. While both share UVB as a common component, the former is unregulated and influenced by factors such as latitude, time of day, weather, and ozone levels. This variability can make it difficult to achieve consistent therapeutic outcomes with sunlight alone.
In contrast, phototherapy offers controlled dosages, targeted wavelength ranges, and medical supervision, significantly reducing the risk of overexposure and adverse effects. For patients with moderate to severe eczema, phototherapy may offer a more reliable and safer alternative to natural sunlight, especially when self-guided sun exposure is impractical or potentially harmful.
That said, for individuals with mild symptoms or those seeking adjunctive strategies, brief, regular sessions of natural sunlight may still hold value. Incorporating sunlight into a holistic approach that includes moisturization, allergen avoidance, and nutritional support can help maximize therapeutic outcomes without relying solely on pharmacologic interventions.

Does Sunlight Help Eczema in Children? Pediatric Considerations and Safety Tips
Parents often wonder whether sunlight exposure is safe and beneficial for children with eczema. Pediatric eczema presents unique challenges, including sensitive skin, smaller body surface area, and greater susceptibility to environmental triggers. Nonetheless, emerging evidence suggests that children, like adults, can benefit from moderate sunlight exposure under careful supervision.
Vitamin D synthesis through sun exposure is particularly relevant in children, who are at higher risk for deficiencies due to indoor lifestyles and excessive sunscreen use. Low vitamin D levels have been correlated with higher eczema prevalence in pediatric populations, and supplementation has shown modest but statistically significant improvements in symptom control.
However, sun safety must be prioritized. Children should never be exposed to intense midday sun, and sessions should be brief—ideally no more than 10 to 15 minutes a few times per week. Lightweight clothing, wide-brimmed hats, and safe sunscreens can provide additional protection. Consultation with a pediatric dermatologist can help tailor sun exposure recommendations to the child’s specific needs and sensitivities.
Lifestyle and Environmental Strategies That Complement Sunlight Exposure
While sunlight can be a helpful component in managing eczema, it is not a standalone solution. Lifestyle modifications and environmental interventions can enhance its effectiveness and prevent flare-ups. One key strategy is optimizing indoor humidity levels, as dry air can exacerbate skin barrier dysfunction. Using humidifiers during winter months or in air-conditioned environments can help maintain skin hydration.
Stress management is another important aspect. Chronic stress has been shown to impair the skin barrier and exacerbate inflammatory responses, both of which can worsen eczema. Techniques such as mindfulness, yoga, and cognitive-behavioral therapy may contribute to better symptom control.
Dietary interventions may also complement sun exposure. Anti-inflammatory diets rich in omega-3 fatty acids, antioxidants, and probiotics have been linked to improvements in skin health. Although more research is needed to establish definitive dietary guidelines, emerging evidence supports the role of nutrition in eczema prevention and management. Together, these lifestyle strategies form a comprehensive approach that supports both the internal and external factors influencing eczema.
Does Sunlight Help Eczema in Different Climates? The Role of Geography and Seasonality
Geographical location and seasonal variation significantly influence how sunlight affects eczema. People living in higher latitudes often experience prolonged winters with reduced UV exposure, leading to vitamin D deficiency and potential worsening of eczema symptoms. Conversely, those in tropical or equatorial regions may receive more consistent sun exposure year-round, which could have a stabilizing effect on skin inflammation.
Studies comparing eczema prevalence across different climates have found lower rates in sun-rich areas, though socioeconomic and genetic factors also play a role. Seasonality is another important factor; many individuals report flares during the winter and improvement during summer. This seasonal pattern aligns with changes in UV exposure, humidity, and indoor heating, all of which affect skin health.
For those living in climates with limited sun exposure, vitamin D supplementation and light therapy devices can serve as alternatives. Portable narrowband UVB lamps, when used under medical supervision, may offer therapeutic benefits similar to natural sunlight. Understanding the interplay between climate and eczema allows for more personalized and context-specific management strategies.
Incorporating Sunlight Safely into an Eczema Care Routine
Developing a sunlight routine requires careful planning and awareness. The goal is to reap the anti-inflammatory benefits of UVB exposure while minimizing the risk of burns and long-term skin damage. Start with short exposures—around 5 to 10 minutes—in the early morning or late afternoon when the UV index is lower. Gradually increase duration based on tolerance and skin response.
Apply a thick, fragrance-free moisturizer before and after sun exposure to maintain hydration and prevent barrier disruption. Avoid using photosensitizing medications or products before going outside, as they can increase the risk of sunburn. Monitor the skin for any signs of irritation, redness, or worsening symptoms, and adjust your routine accordingly.
Keeping a sun exposure journal can be helpful in tracking what works best for your skin. Record the time of day, duration, weather conditions, and any subsequent skin changes. This personalized data can inform future strategies and help you and your healthcare provider optimize your care plan.
Frequently Asked Questions: Natural Sunlight and Eczema Management
How does seasonal sunlight variation affect eczema patterns year-round?
Seasonal sunlight changes can significantly influence the frequency and intensity of eczema flare-ups. During winter months, lower UV levels and decreased outdoor activity often lead to drier skin and more frequent inflammation. In contrast, warmer months typically bring increased sun exposure, which can have a stabilizing effect for some individuals due to UVB’s immunomodulatory benefits. However, seasonal allergies and sweat-induced irritation during summer may counterbalance these benefits for others. It’s important for people managing eczema to adapt their skincare and sun exposure habits to seasonal shifts, considering both environmental triggers and potential therapeutic gains from natural sunlight.
Are there specific times of day when sunlight exposure is safest and most effective for eczema?
The safest and most effective times to receive sunlight are typically early in the morning or late in the afternoon, when UV intensity is lower. These timeframes help reduce the risk of sunburn while still offering sufficient exposure to UVB rays, which can benefit eczema by reducing skin inflammation. Midday sun exposure, while higher in UVB, carries a greater risk for damage and should be limited or avoided unless specifically guided by a healthcare provider. Additionally, using a UV index app can help identify ideal times for safe sun therapy based on your geographical location. Incorporating these practices aligns with both the goals of F4. Skin Conditions & Dermal Health and overall sun safety.
Can vitamin D supplements replicate the benefits of natural sunlight for eczema?
While vitamin D supplements can help address deficiencies that may exacerbate eczema symptoms, they do not fully replicate the effects of natural sunlight. Sunlight, particularly UVB exposure, offers localized immune modulation in the skin that oral supplements cannot mimic. Supplements are useful in winter or for individuals who cannot tolerate sun exposure due to photosensitivity or geographic limitations. However, the full spectrum of benefits linked to sunlight—including mental health improvements and the synthesis of other photoproducts—is more comprehensive than what a capsule can deliver. Therefore, a combined approach using supplements and moderate sun exposure may offer the best outcomes for those managing eczema under the F. Common Conditions & Everyday Ailments category.
Does sunlight help eczema in individuals with darker skin tones?
Yes, but the response can vary. People with darker skin tones have more melanin, which naturally filters UV radiation and may require longer sun exposure to achieve the same vitamin D synthesis as those with lighter skin. This filtering effect can also mean that the therapeutic impact of UVB on eczema symptoms might be less intense unless sun exposure is slightly prolonged. However, darker skin provides more natural protection against sunburn, making sun therapy safer in some respects. It’s still essential for all individuals, regardless of skin tone, to start with brief exposure and gradually increase time in the sun while monitoring for signs of irritation. Managing eczema across diverse populations requires nuanced approaches that reflect both dermatological needs and cultural practices, in line with the ethos of F4. Skin Conditions & Dermal Health.
Are there wearable technologies that help manage sun exposure for eczema therapy?
Recent advancements in wearable tech have introduced UV sensors that can help eczema patients monitor and manage their sun exposure with precision. These small, often wrist-worn devices track cumulative UV exposure and send alerts to mobile apps, empowering users to stay within safe thresholds. Some models also integrate humidity and temperature data, offering a more holistic view of environmental conditions that affect eczema. This personalized data enables users to make informed decisions and avoid both underexposure, which may limit benefits, and overexposure, which increases the risk of sunburn. As these devices gain traction, they are becoming a valuable tool in managing F. Common Conditions & Everyday Ailments through proactive self-care.
Does sunlight help eczema that appears on the face or other sensitive areas?
Facial eczema and flare-ups on sensitive areas like the neck or eyelids require extra caution when using sunlight for therapeutic purposes. The skin in these regions is thinner and more prone to damage, so sun exposure should be minimal and indirect. Hats with wide brims and physical sunscreens made from zinc oxide or titanium dioxide can offer selective protection, allowing safe exposure to unaffected areas. Some dermatologists may recommend patch-testing sunlight exposure on a small area to gauge response before expanding to other regions. Incorporating such targeted strategies aligns well with F4. Skin Conditions & Dermal Health by promoting safe and effective interventions for delicate skin zones.
How can mental health and stress reduction enhance sunlight’s effects on eczema?
Psychological stress is a well-known trigger for eczema flare-ups, and reducing stress can amplify the benefits of sunlight therapy. Sunlight exposure itself has mood-elevating effects due to the stimulation of serotonin and regulation of circadian rhythms, both of which contribute to improved mental well-being. When combined with stress-reducing activities like mindful walking outdoors, gardening, or nature-based meditation, sunlight can become part of a holistic strategy for managing eczema. This dual benefit—physical and emotional—reinforces the role of lifestyle in the F. Common Conditions & Everyday Ailments category. Patients often find that addressing mental health creates a positive feedback loop, improving their resilience to skin irritants and enhancing recovery during flare-ups.
Does Sunlight Help Eczema More in Natural Environments Like Beaches or Forests?
Natural environments such as beaches and forests can enhance the benefits of sunlight exposure for eczema beyond what’s available in urban settings. Beaches offer a unique combination of saltwater, sunlight, and increased humidity, all of which can soothe the skin and improve moisture retention. Forested areas, while not saline, often feature cleaner air and lower allergen levels, which can reduce skin irritation and support recovery. These settings also encourage relaxation and movement, both of which help reduce stress, a common eczema trigger. Integrating therapeutic sunlight with natural environments reflects a comprehensive understanding of F. Common Conditions & Everyday Ailments and shows how location-specific exposure can enhance symptom relief.
How long does it take to see improvements if sunlight is helping your eczema?
The timeline for seeing results from sunlight therapy varies, but many people report noticeable improvement within two to three weeks of consistent, moderate exposure. The key is maintaining a steady routine—short, frequent sessions are often more effective and safer than occasional long exposures. Factors such as skin type, baseline vitamin D levels, and severity of eczema all influence how quickly benefits emerge. It’s also important to recognize that some individuals may not respond or might even experience worsening symptoms, particularly if sun sensitivity or other underlying conditions are present. Monitoring and documenting your progress can help determine whether sunlight is truly contributing to healing, aligning with best practices in F4. Skin Conditions & Dermal Health.
Does Sunlight Help Eczema as Effectively When Combined with Other Natural Therapies?
Yes, combining sunlight therapy with other natural interventions can yield synergistic effects for eczema management. Practices such as applying oatmeal-based moisturizers, using essential oils like chamomile (after patch testing), or taking probiotic supplements can enhance skin barrier repair and reduce inflammation. These complementary strategies often work best when timed strategically, such as moisturizing immediately after sun exposure to lock in hydration. Including anti-inflammatory foods like turmeric, fatty fish, and leafy greens in your diet can also boost systemic resilience to eczema triggers. This integrative approach demonstrates how multifaceted, nature-aligned strategies can enrich the healing process under the broader umbrella of F. Common Conditions & Everyday Ailments.
Final Thoughts: The Balanced Truth About Sunlight and Eczema Management
So, does sunlight help eczema? The answer is nuanced. While scientific evidence supports the beneficial effects of controlled UV exposure on skin inflammation, immune modulation, and vitamin D synthesis, individual responses can vary widely. For many, sunlight offers a natural, accessible, and cost-effective tool to complement conventional eczema treatments. However, it must be approached with caution, personalization, and medical guidance to prevent adverse effects.
Understanding whether or not the sun is good for eczema depends on a range of factors, including skin type, medical history, climate, and coexisting conditions. It is not a one-size-fits-all solution but rather one piece of a multifaceted strategy that also includes moisturizing routines, dietary support, stress reduction, and sometimes medical therapies.
Ultimately, sunlight holds promise as part of a holistic and proactive eczema management plan. By embracing a balanced approach that respects both the therapeutic potential and risks of UV exposure, individuals with eczema can make informed decisions that improve skin health and quality of life. The ongoing question of “does sunlight help eczema” invites continued research, personalized care, and a deeper appreciation for the complex interplay between nature and the human body.


