Description
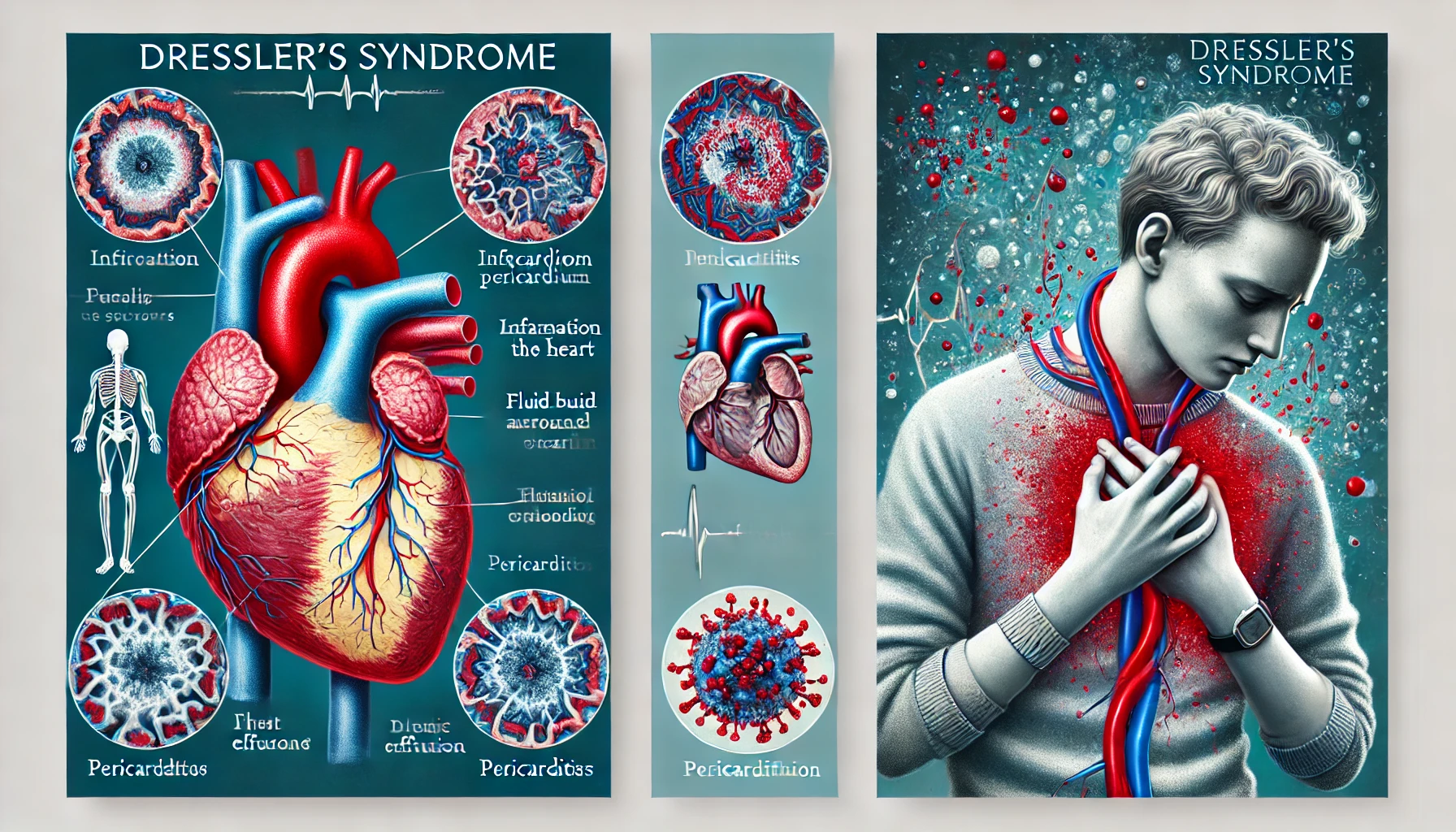
Dressler’s syndrome represents a rare but severe condition that often manifests weeks to months following cardiac surgery or myocardial infarction (MI) and is identified by pleuritis, pericarditis, and fever. It is named after William Dressler, who initially reported it in 1956. Due to the syndrome’s inconsistent clinical presentation and symptoms that frequently coexist with those of other pulmonary and cardiac disorders, diagnosing it can be difficult. The symptoms of Dressler’s syndrome may encompass fever, chest pain, pleuritic pain (i.e., pain during breathing), pleuritis (i.e., swelling of the pleura), and pericarditis (i.e., swelling of the pericardium). Patient complaints about feeling ill and worn out are common.
After an incident of myocardial infarction or heart surgery, the condition may appear sometime between some days and several weeks later. Dressler’s syndrome is thought to be caused by an immunological response brought on by antigens discharged from damaged cardiac or pericardial tissue, though the specific mechanism is still unknown.
You May Also Like:
Crohn’s disease (CD): Description, Causes, and Treatment Protocol
IgA nephropathy / Berger’s disease: Description, Causes, and Treatment Protocol
Dressler’s syndrome / postmyocardial infarction / postpericardiotomy syndrome: Description, Causes, and Treatment Protocol is an original (MedNewsPedia) article.
Possible Causes
It is unknown with certainty what causes Dressler’s syndrome, additionally referred to as postpericardiotomy syndrome or postmyocardial infarction syndrome. However, several explanations and causes that have been presented include the following: –
Autoimmunity: The immune system incorrectly attacks self-antigens or proteins secreted from injured cardiac or pericardial tissues in Dressler’s syndrome, it is thought. In simple terms, the immune system views these self-antigens as outside invaders and mounts an immunological attack on them.
Antigen Release: The heart muscle or pericardium suffers tissue damage after cardiac surgery or myocardial infarction (MI). Proteins or antigens from damaged cardiac or pericardial tissues may be released into the bloodstream as a result of this injury. These secreted antigens may cause an immunological reaction, which could result in inflammation and the emergence of Dressler’s syndrome.
Genetic Predisposition: Certain individuals may be genetically predisposed to autoimmune disorders or aberrant immune reactions. Dressler’s syndrome risk may be increased by a family record of autoimmune diseases, indicating that genetics may be involved in its genesis.
Post-Surgical Factors: Following cardiac surgery, especially pericardiotomies (operations to split open or remove a portion of the pericardium), Dressler’s syndrome can develop. The condition may emerge as a result of the pericardium becoming irritated during surgery. The pericardium can leak antigens or cause an inflammatory response when it is surgically altered.
Delayed Immune Response: A delayed immunological reaction against cardiac or pericardial damage can occasionally lead to Dressler’s syndrome. When an immune reaction occurs, it may be stronger and last longer if the immune system’s detection of self-antigens or an inflammatory reaction is delayed.
Immune Dysregulation: Dysregulation of the immune system, or dysfunction of the immune system, might represent a contributing factor. The inflammation observed in Dressler’s syndrome can be brought on by an exacerbated or protracted immunological reaction to tissue injury.

Exacerbating and Mitigating Factors
Dressler’s syndrome, additionally referred to as postpericardiotomy syndrome or postmyocardial infarction syndrome, develops and progresses as a result of aggravating and mitigating variables. Specifically, such factors are thoroughly explained as follows: –
The exacerbating factors include: –
Delayed Immune Response: The chance of getting Dressler’s syndrome can rise if the immune system reacts slowly to cardiac damage. A more potent and protracted inflammatory response may result from the immune system’s delayed detection of self-antigens produced from injured cardiac or pericardial tissues.
Genetic Susceptibility: An autoimmune disease or aberrant immune response may be genetically predisposed in some people. Dressler’s syndrome risk may be increased by an autoimmune disease in the family history.
Extensive Cardiac Injury: The probability and severity of Dressler’s syndrome can vary depending on the degree of the initial cardiac surgery or myocardial infarction (MI). An increased immunological response brought on by a more severe heart injury may exacerbate the condition.

The mitigating factors include: –
Timely Diagnosis and Therapy: Pericardial issues or myocardial infarctions must be diagnosed and treated promptly. By reducing heart tissue damage and inflammation, early management can lower the risk of developing Dressler’s syndrome.
Genetic Testing: The risk of autoimmune illnesses or aberrant immune responses may be determined by identifying genetic predispositions. Although it is not commonly done, genetic testing may be taken into consideration in certain situations where people have a significant family history of autoimmune diseases.
Immunosuppressive Therapy: Immunosuppressive drugs may be prescribed for severe or chronic inflammation. As a result, the intensity of Dressler’s syndrome may be reduced with the aid of these medications.
Stress Reduction: Stress is known to make autoimmune diseases and inflammatory reactions worse. Encouragement of stress-reduction methods like mindfulness practices, relaxation exercises, and counseling may decrease the impact of elevated stress levels on Dressler’s syndrome.
Medication Adherence: Dressler’s syndrome must be managed with strict adherence to recommended drugs like NSAIDs or colchicine. To ensure optimal therapy, patients should heed the advice of their healthcare professionals.
Lifestyle Modifications: Comprehensive cardiovascular health can be influenced by lifestyle choices such as keeping a heart-healthy diet, getting regular exercise, and quitting smoking. These behaviors may decrease the possibility of myocardial infarction, which, in turn, causes Dressler’s syndrome.
Patient Education: Patients who are informed about Dressler’s syndrome’s signs and symptoms and the value of getting help right away following a cardiac surgery or heart attack may benefit from early intervention and fewer consequences.
Vaccination: In certain scenarios, immunization against specific infectious pathogens may help lower the possibility of inducing autoimmune reactions that can worsen Dressler’s condition. As a healthcare professional, though, this strategy should be reviewed.
Standard Treatment Protocol
Dressler’s syndrome is normally treated with an assortment of therapeutic techniques that target inflammation control, pain management, and problem avoidance. The typical treatment regimen may involve: –
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs, like indomethacin or ibuprofen, are frequently recommended to treat Dressler’s syndrome-related pain and inflammation. These drugs offer pericarditis and pleuritis treatment by reducing the inflammatory response.
Colchicine: A common anti-inflammatory drug utilized to treat gout, colchicine has also shown promise in treating Dressler’s syndrome-related recurrent pericarditis. It is typically administered along with NSAIDs.
Corticosteroids: Corticosteroids like prednisone can be considered in cases of major inflammation that fails to respond well to NSAIDs or colchicine. These drugs offer strong anti-inflammatory benefits, but due to possible adverse effects, they are normally only used in more severe instances.
Analgesics: Treatment for Dressler’s condition must include pain control. To relieve discomfort and chest pain, it may be advised to use over-the-counter analgesics, including acetaminophen (paracetamol).
Cardiac Monitoring: To identify and treat any possible issues, like arrhythmias or heart failure, continuous monitoring is necessary.
Pericardiocentesis: A pericardiocentesis technique can be required if the situation does not improve with medical treatment or if there is a large pericardial effusion that compromises hemodynamics. To relieve strain on the heart, excess fluid in the pericardial area must be drained.
Bed Rest: To regulate heart strain and alleviate symptoms, enough rest is frequently prescribed. Until symptoms go away, patients might need to restrict their physical activities.

Treatment Options
Some people diagnosed with Dressler’s syndrome could investigate adjunct treatment alternatives together with the conventional course of care to aid their recovery. The following are potential supplemental therapies: –
Vitamin D: The health of the immune system depends on optimal vitamin D levels. Getting enough vitamin D may help the body’s immunological response. If a vitamin D shortage is found, it can be treated with supplements, sunshine exposure, or food sources.
Omega-3 Fatty Acids: Anti-inflammatory qualities are present in omega-3 supplements that are made from fish oil capsules. They could assist in minimizing the inflammatory reaction linked to Dressler’s syndrome.
Probiotics: Probiotics may aid in immune system regulation and inflammation reduction, according to certain research. Probiotic-rich meals and supplements may be thought of as a way to support general health.
Bromelain: An enzyme generated from pineapples called bromelain has anti-inflammatory qualities and may help relieve pain and inflammation. It is available as a supplement.
Turmeric (Curcumin): A component of turmeric called curcumin contains natural anti-inflammatory properties and may help with symptom relief. It may be consumed as a supplement or as a component of a diet.
Ginger: In order to relieve discomfort, ginger can be ingested as a supplement, added to food, or drunk as tea.
Arnica: Arnica, a supplement that can be taken orally or applied topically, is thought to have anti-inflammatory properties that might assist with pain relief. Carefully following dose directions is imperative.
Mind-Body Practices: By enhancing overall health, stress-reduction methods like meditation, yoga, and deep breathing exercises can complement standard treatments. Dressler’s syndrome might make stress management more crucial because stress can make symptoms worse.
However, it is essential to stress that, despite the possibility of advantages, these adjunct therapies should not be utilized in place of regular medical care. Before beginning any new therapy or supplement regimen, patients should always speak with their healthcare physician. Individual reactions to these adjunct therapies can also vary, making it crucial to closely monitor symptoms and communicate with a healthcare professional to ensure proper treatment for Dressler’s syndrome.
Conclusion
Dressler’s syndrome, or post-myocardial infarction/post-pericardiotomy syndrome, remains a rare yet significant condition that requires prompt recognition and effective management. Characterized by immune-mediated inflammation following cardiac injury or surgery, its timely diagnosis is essential to prevent complications and enhance patient outcomes. Standard treatment protocols, including NSAIDs, colchicine, and corticosteroids, are highly effective in managing symptoms and inflammation, while adjunct therapies such as omega-3 fatty acids, probiotics, and stress management techniques may provide additional support.
A tailored, patient-centered approach that incorporates timely medical intervention, lifestyle modifications, and ongoing monitoring can significantly alleviate symptoms and improve quality of life. Collaboration between patients and healthcare providers is critical in ensuring optimal care and preventing recurrence. For those experiencing symptoms of Dressler’s syndrome, seeking early medical advice and adhering to prescribed treatments remains the cornerstone of effective management.

Additional resources for further reference
https://www.sciencedirect.com/science/article/pii/S2666602221000665
https://www.sciencedirect.com/science/article/pii/S0147956397900777
https://www.tandfonline.com/doi/abs/10.1080/08916930290028166
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.