Introduction
Carotid artery disease is a significant yet often overlooked health concern that can lead to life-threatening complications such as strokes. The carotid arteries, also known as the neck arteries, play a crucial role in supplying oxygen-rich blood to the brain. When these arteries become narrowed due to plaque buildup, a condition known as carotid artery stenosis, the risk of stroke increases dramatically. Understanding the early warning signs of carotid artery blockage is essential for early intervention and effective management. This article provides an in-depth exploration of the symptoms, risks, diagnostic methods, and treatment options for carotid artery disease.
You may also like: How to Naturally Reverse 20 Years of Arterial Plaque: Science-Backed Strategies for a Healthier Heart
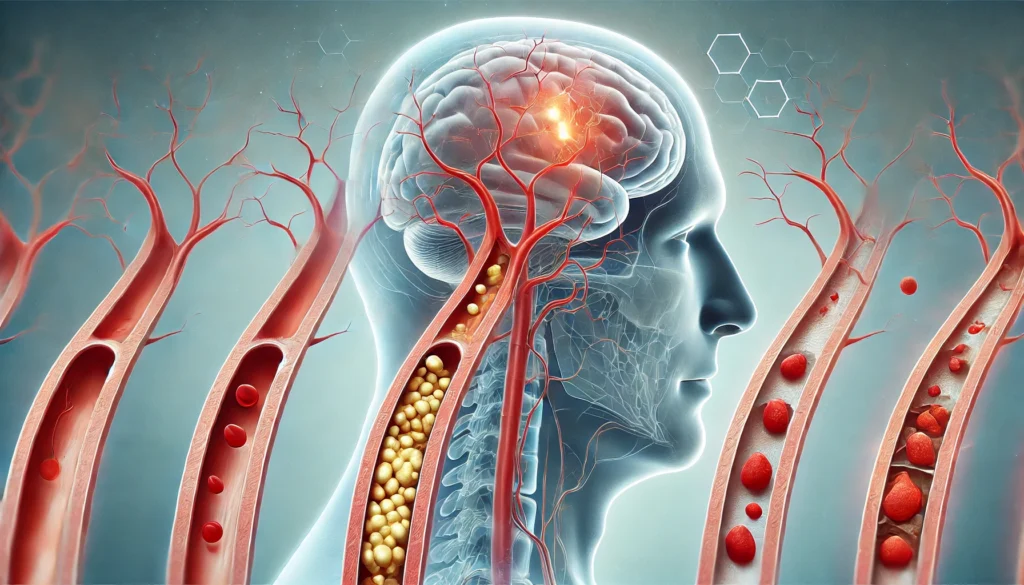
Understanding Carotid Artery Disease
The carotid arteries are two large blood vessels that run along either side of the neck, supplying oxygenated blood to the brain, face, and scalp. Carotid artery disease occurs when these arteries become narrowed or blocked due to the accumulation of plaque, which consists of fatty deposits, cholesterol, calcium, and other substances. This condition, known as carotid artery stenosis, can significantly reduce blood flow to the brain, increasing the risk of ischemic stroke.
Causes of Carotid Artery Stenosis
Carotid artery stenosis primarily develops due to atherosclerosis, a condition characterized by the gradual buildup of plaque within the arteries. Risk factors for atherosclerosis include high blood pressure, smoking, diabetes, high cholesterol levels, obesity, and a sedentary lifestyle. Additionally, genetic predisposition and advancing age contribute to the likelihood of developing carotid artery disease. Other factors, such as chronic inflammation and autoimmune conditions, can further accelerate arterial narrowing.
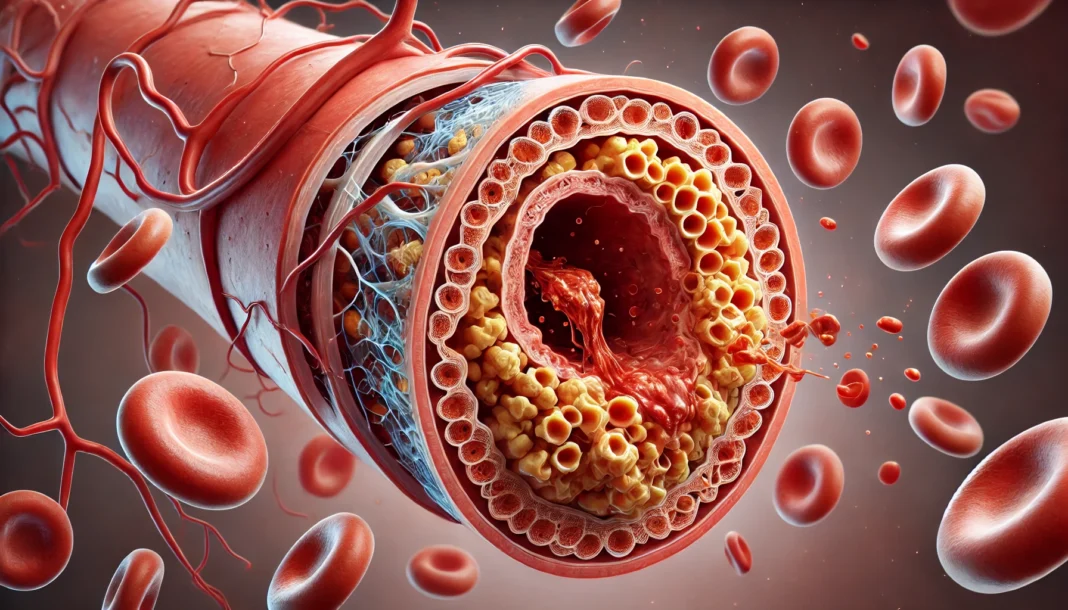
How Plaque Leads to Blockage
Plaque buildup within the carotid arteries can lead to significant narrowing, restricting blood flow to the brain. Over time, this process can result in a complete blockage, known as an occluded carotid artery, which dramatically increases the risk of a stroke. Additionally, plaque can rupture, causing blood clots to form and travel to smaller arteries in the brain, leading to an ischemic event. Understanding how to clear plaque from the carotid artery is crucial in preventing severe complications.
Recognizing the Early Symptoms of Carotid Artery Blockage
Carotid artery disease often progresses silently, without noticeable symptoms, until a severe event such as a transient ischemic attack (TIA) or stroke occurs. However, some early warning signs can indicate reduced blood flow to the brain. Recognizing these symptoms and seeking prompt medical attention can prevent a catastrophic event.
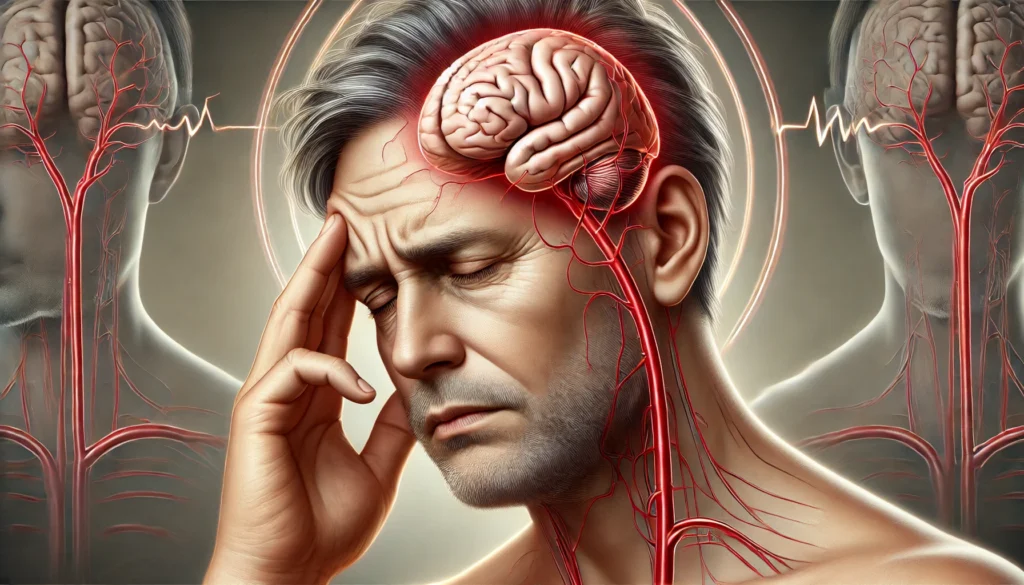
Transient Ischemic Attack (TIA): A Warning Sign
A transient ischemic attack, also referred to as a “mini-stroke,” occurs when blood flow to the brain is temporarily interrupted. TIAs serve as an early warning sign of carotid artery disease and should never be ignored. Common symptoms of a TIA include sudden weakness or numbness in one side of the body, temporary loss of vision in one eye, slurred speech, dizziness, and confusion. While TIAs typically resolve within a few minutes to hours, they are a strong indicator of an impending stroke.
Symptoms of Carotid Artery Blockage
Symptoms of carotid artery blockage often resemble those of a stroke and may include sudden weakness or paralysis in the face, arms, or legs, particularly on one side of the body. Other warning signs include difficulty speaking, vision disturbances, severe headaches, and loss of coordination. In some cases, individuals may experience symptoms of a clogged carotid artery in the form of brief episodes of dizziness or fainting. These symptoms indicate that blood flow to the brain is compromised and require immediate medical attention.
Risk Factors Associated with Carotid Artery Disease
Certain risk factors significantly increase the likelihood of developing carotid artery disease. While some factors, such as aging and genetic predisposition, cannot be controlled, many lifestyle-related risk factors can be managed through preventive measures.
Modifiable Risk Factors
Modifiable risk factors for carotid artery disease include smoking, high blood pressure, diabetes, high cholesterol levels, and obesity. Smoking is particularly harmful as it damages the lining of the blood vessels, promoting plaque buildup. Additionally, poorly managed diabetes and high blood pressure accelerate the progression of atherosclerosis, increasing the risk of carotid artery stenosis.
Non-Modifiable Risk Factors
Non-modifiable risk factors include age, gender, and family history. Individuals over the age of 60 are at a higher risk of developing carotid artery disease. Men are generally more susceptible to carotid artery stenosis at a younger age, although postmenopausal women also face increased risks due to hormonal changes. A family history of cardiovascular diseases further predisposes individuals to carotid artery disease.
Diagnostic Methods for Carotid Artery Stenosis
Early detection of carotid artery disease is crucial in preventing severe complications. Various diagnostic tools help assess the severity of carotid artery stenosis and determine the appropriate course of action.
Carotid Ultrasound
A carotid ultrasound is a non-invasive imaging test that uses sound waves to create detailed images of the carotid arteries. This test helps detect the presence of plaque buildup and assesses blood flow, making it a standard tool for diagnosing carotid artery stenosis.
CT and MRI Angiography
Computed tomography (CT) angiography and magnetic resonance imaging (MRI) angiography provide detailed images of the carotid arteries. These advanced imaging techniques help detect arterial blockages and evaluate the extent of stenosis.
Physical Examination and Auscultation
During a physical examination, a physician may use a stethoscope to listen for abnormal sounds, known as bruits, in the carotid arteries. The presence of a bruit suggests turbulent blood flow, indicating potential narrowing or blockage.
Treatment Options for Carotid Artery Blockage
Treatment for carotid artery stenosis depends on the severity of the blockage and the presence of symptoms. Options range from lifestyle modifications to surgical interventions.
Lifestyle Changes and Medication
For individuals with mild to moderate carotid artery disease, lifestyle changes and medications can help slow the progression of arterial narrowing. Adopting a heart-healthy diet, engaging in regular physical activity, and quitting smoking are essential steps in managing carotid artery stenosis. Medications such as antiplatelet drugs, cholesterol-lowering statins, and blood pressure-lowering medications are commonly prescribed to reduce stroke risk.
Surgical Interventions
Severe carotid artery stenosis may require surgical intervention to restore normal blood flow. Carotid endarterectomy is a procedure in which surgeons remove plaque buildup from the carotid artery. Alternatively, carotid artery stenting involves the placement of a stent to keep the artery open and improve blood flow.

Frequently Asked Questions About Carotid Artery Blockage
1. What are the early warning signs of carotid artery blockage, and how do they differ from a stroke?
Carotid artery blockage often develops silently, with symptoms appearing only when blood flow is significantly restricted. Unlike a full-blown stroke, early warning signs of carotid stenosis may include transient ischemic attacks (TIAs), also known as mini-strokes. Symptoms of carotid artery blockage include brief episodes of weakness or numbness on one side of the body, vision disturbances such as temporary blindness in one eye, difficulty speaking, and dizziness. These symptoms often resolve within minutes to hours, making them easy to dismiss, but they serve as a critical warning of an impending stroke. Recognizing these signs early allows for medical intervention, significantly reducing the risk of permanent brain damage or a life-threatening stroke.
2. How can I check if I have carotid artery stenosis before symptoms appear?
Carotid artery stenosis is frequently detected during routine medical examinations before symptoms become apparent. Physicians often listen for abnormal sounds, known as bruits, using a stethoscope over the throat artery, which can indicate turbulent blood flow. Diagnostic tests such as carotid ultrasound, computed tomography angiography (CTA), or magnetic resonance angiography (MRA) provide detailed imaging of the arteries and can detect the extent of narrowing. People with high-risk factors, including high cholesterol, smoking, and hypertension, should proactively request screening. Early detection of carotid artery disease allows for lifestyle modifications and medical management to prevent progression.
3. Can carotid artery disease be reversed through lifestyle changes alone?
While carotid artery disease cannot be fully reversed through lifestyle changes alone, its progression can be significantly slowed, and in some cases, minor improvements may occur. Adopting a heart-healthy diet rich in fiber, omega-3 fatty acids, and antioxidants can help reduce cholesterol levels, which contribute to plaque buildup. Regular physical activity improves circulation and helps maintain arterial health, while smoking cessation dramatically reduces the risk of further artery stenosis. Blood pressure and blood sugar control are crucial in preventing additional damage to the artery walls. In cases of mild carotid artery stenosis, these measures, combined with medication, can effectively prevent worsening and reduce stroke risk.
4. What medical treatments are available for carotid artery stenosis?
Carotid artery stenosis treatment varies depending on the severity of the blockage. In mild to moderate cases, lifestyle changes and medications such as statins, antiplatelet drugs, and blood pressure medications can help manage the condition. For severe carotid artery blockage, surgical interventions may be necessary. Carotid endarterectomy is a procedure that removes plaque buildup directly from the artery to restore normal blood flow. Another option is carotid artery stenting, which involves placing a small mesh tube within the artery to keep it open. The choice of treatment depends on individual health factors and the extent of the blockage.
5. Is bilateral carotid artery stenosis more dangerous than unilateral stenosis?
Bilateral carotid artery stenosis, in which both carotid arteries are narrowed, poses a greater risk than unilateral (one-sided) stenosis. This condition reduces the brain’s ability to compensate for reduced blood flow, increasing the likelihood of a stroke. Symptoms of occluded carotid artery in both sides may include cognitive impairments, balance problems, and frequent TIAs. Bilateral stenosis also complicates treatment decisions, as surgical procedures on both arteries require careful planning to avoid reducing cerebral blood supply. Individuals diagnosed with bilateral carotid artery stenosis should undergo frequent monitoring and aggressive risk factor management to prevent severe complications.
6. What is the role of inflammation in carotid artery disease?
Chronic inflammation plays a crucial role in the development and progression of carotid artery disease. Inflammatory processes contribute to the formation of plaques that narrow the arteries and increase the risk of rupture. Conditions such as rheumatoid arthritis, lupus, and chronic infections can accelerate arterial inflammation. Blood markers like C-reactive protein (CRP) levels are often elevated in individuals with significant artery stenosis, indicating ongoing vascular inflammation. Managing inflammation through dietary changes, anti-inflammatory medications, and controlling underlying conditions can help slow the progression of carotid artery blockage.
7. What are the best dietary strategies to prevent carotid artery disease?
A diet that supports vascular health can help prevent and slow the progression of carotid artery disease. Consuming foods rich in omega-3 fatty acids, such as salmon, flaxseeds, and walnuts, helps reduce arterial inflammation. High-fiber foods like oats, beans, and whole grains help lower cholesterol levels, reducing the risk of artery stenosis. Antioxidant-rich fruits and vegetables support endothelial function, maintaining arterial flexibility. Reducing saturated fats, trans fats, and processed sugars prevents excessive plaque formation in the throat artery. Hydration and proper electrolyte balance also support optimal blood viscosity, reducing the likelihood of clot formation.
8. How effective are natural remedies in managing carotid artery stenosis?
Natural remedies can support overall cardiovascular health but should not replace medical treatments for carotid artery stenosis. Supplements such as omega-3 fatty acids, garlic extract, and Coenzyme Q10 may help lower cholesterol and reduce inflammation, but their effectiveness varies among individuals. Certain herbal compounds, like turmeric and green tea, contain antioxidants that support arterial function. However, these remedies should be used in conjunction with prescribed medications and lifestyle changes rather than as stand-alone treatments. Consulting with a healthcare provider before starting any supplements ensures safety and effectiveness, especially for individuals on blood-thinning medications.
9. Can carotid artery blockage lead to cognitive decline?
Yes, carotid artery blockage can contribute to cognitive decline due to reduced blood flow to the brain. Chronic hypoperfusion, or insufficient blood supply, affects brain function, leading to memory problems, difficulty concentrating, and slowed mental processing. Studies suggest that individuals with significant internal carotid artery stenosis have a higher risk of developing vascular dementia. Addressing carotid artery disease through medical management, lifestyle modifications, and, if necessary, surgical intervention can help preserve cognitive function. Early diagnosis and treatment are essential in preventing long-term neurological complications associated with artery stenosis.
10. What are the latest advancements in carotid artery stenosis treatment?
Advancements in carotid artery stenosis treatment continue to improve patient outcomes and reduce procedural risks. New-generation stents with drug-eluting properties help prevent re-narrowing of the artery after placement. Minimally invasive techniques, such as transcarotid artery revascularization (TCAR), reduce the risk of complications compared to traditional carotid endarterectomy. Emerging research explores the potential of gene therapy and targeted molecular treatments to reduce plaque buildup in the carotid arteries. Artificial intelligence and machine learning are also being integrated into diagnostic tools, improving the accuracy of carotid artery disease detection. These innovations offer promising options for individuals seeking effective and less invasive carotid stenosis treatment.
Conclusion
Carotid artery disease is a serious but preventable condition that requires early detection and intervention. Recognizing the early warning signs of carotid artery blockage, understanding the associated risk factors, and seeking timely medical attention can significantly reduce the risk of stroke. By adopting a healthy lifestyle and following medical recommendations, individuals can protect their vascular health and reduce the likelihood of severe complications.
vascular health, cerebrovascular disease, stroke prevention tips, arterial plaque buildup, brain blood flow, ischemic stroke risk, cardiovascular wellness, cholesterol and arteries, blood circulation improvement, hypertension management, heart disease prevention, vascular surgery options, neurovascular health, transient ischemic attack signs, healthy arteries diet, medical imaging diagnostics, atherosclerosis treatment, lifestyle changes for heart health, cerebrovascular disorders, blood clot prevention
Further Reading:
Carotid Artery Disease (Carotid Artery Stenosis)
What to know about carotid artery disease
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.