Understanding how to effectively educate patients about high blood pressure is not just a task for clinicians—it is a cornerstone of successful long-term hypertension management. As cardiovascular diseases remain a leading cause of death worldwide, addressing hypertension through patient-focused education becomes critical. This article delves into the essential strategies and scientific principles behind effective hypertension patient education, exploring how it can significantly influence treatment adherence, lifestyle changes, and overall cardiovascular health outcomes. The following exploration highlights the vital importance of high blood pressure patient education, and provides a comprehensive look at how tailored communication, structured care plans, and ongoing support can transform the prognosis for individuals living with this silent but deadly condition.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Defining Hypertension and Its Implications for Patients
Hypertension, or high blood pressure, occurs when the force of blood pushing against the arterial walls remains consistently elevated. Often referred to as the “silent killer,” it rarely presents with noticeable symptoms in its early stages but can lead to serious complications such as stroke, heart attack, kidney disease, and heart failure. Educating patients about hypertension is essential because it empowers them with the knowledge needed to manage their condition proactively. High blood pressure care plans that incorporate patient involvement are particularly effective because they promote accountability and encourage behavior change.
For a patient with hypertension, understanding their condition helps to demystify the numbers associated with blood pressure readings. Many individuals are unaware of what their blood pressure should be, or what the numbers even mean. Health education for hypertensive patients must include clear explanations of systolic and diastolic pressure, the significance of these readings, and how lifestyle factors such as diet, physical activity, stress, alcohol, and smoking contribute to their overall cardiovascular risk. Such comprehensive education creates a foundational understanding necessary for informed decision-making and long-term self-management.
The Role of Hypertension Patient Education in Clinical Practice
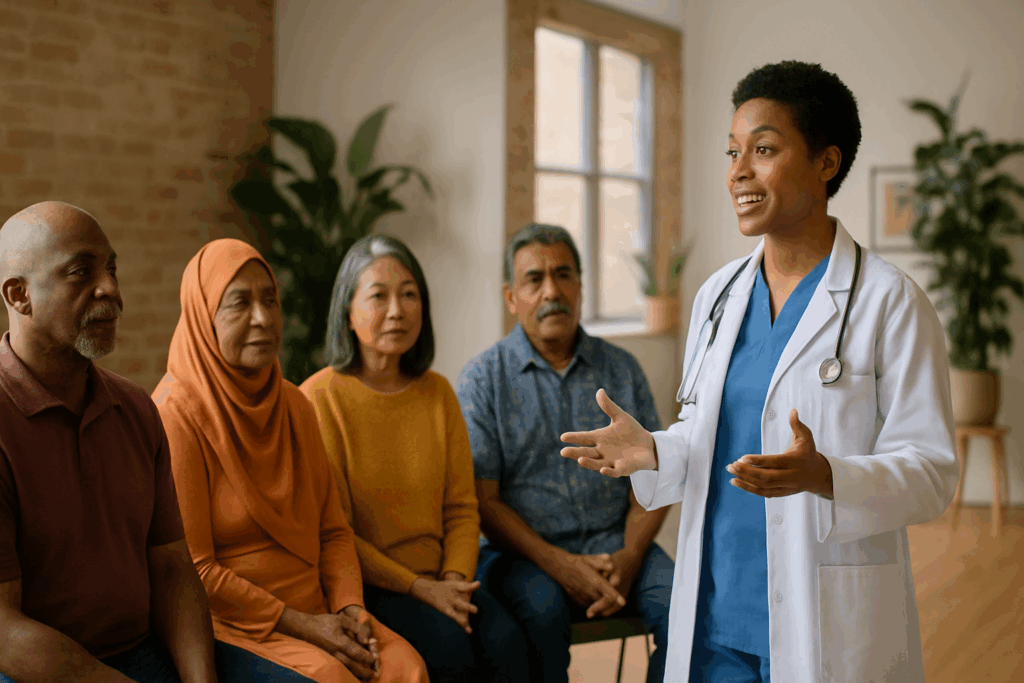
Hypertension patient education is an integral component of primary care, cardiology, and internal medicine practices. It extends beyond handing out pamphlets or offering generic advice; rather, it requires an individualized, patient-centered approach that considers the person’s language, literacy level, cultural background, and readiness to change. A strong protocol for high blood pressure education involves clear, empathetic communication paired with supportive resources that help patients absorb and act on what they learn.
Clinicians must recognize that patient teaching on hypertension is not a one-time conversation. Instead, it is an ongoing dialogue that evolves over time. Patients benefit most when they are engaged through teach-back methods, goal-setting exercises, and shared decision-making practices. This dynamic approach helps patients understand not just what to do, but why it matters. For example, explaining how reducing sodium intake can lower blood pressure provides more motivation when tied to personal outcomes, such as decreasing the need for medications or avoiding future hospitalizations.
Furthermore, effective hypertension education includes addressing common misconceptions. Many patients believe that once their blood pressure is controlled with medication, lifestyle changes are no longer necessary. Ongoing education corrects this misunderstanding and reinforces that medications and lifestyle interventions work synergistically. Consistent reinforcement through office visits, digital health tools, and community programs can enhance adherence and prevent relapse.
Designing a Comprehensive High Blood Pressure Care Plan
A well-designed high blood pressure care plan is holistic, involving pharmacologic treatment, behavioral strategies, and patient support mechanisms. Each component should be framed within the context of the patient’s life, values, and goals. For instance, dietary counseling should account for cultural preferences, budget limitations, and cooking habits. Similarly, physical activity recommendations should consider mobility issues, time constraints, and safety concerns.
Education for high blood pressure should be seamlessly integrated into every aspect of the care plan. From explaining how different antihypertensive drugs work, to setting realistic goals for blood pressure targets, each step must include an educational element. Teaching hypertension management skills might involve guiding a patient through how to properly measure their blood pressure at home or recognizing early warning signs of hypertensive crises. These practical skills can drastically improve outcomes when coupled with personalized coaching and follow-up.
Patient teaching for hypertension must also encompass mental and emotional health. Stress is a major contributor to high blood pressure, and patients should be educated about the physiological connection between chronic stress and cardiovascular strain. Techniques such as mindfulness, deep breathing exercises, and time management can be integrated into the care plan as non-pharmacologic strategies for blood pressure control. When patients understand that hypertension is not just a number on a screen but a multifaceted condition affected by the mind and body, they are more likely to engage fully in their care.
Cultural Competency in High Blood Pressure Teaching
Delivering effective high blood pressure teaching requires cultural sensitivity and an awareness of health disparities. Different communities may have varying beliefs about illness, medication, and healthcare providers, which can influence how they receive and interpret hypertension education. For example, in some cultures, there may be a strong reliance on traditional remedies or spiritual practices, which must be acknowledged respectfully while still providing evidence-based guidance.
Language barriers also pose a significant challenge. Providing hypertension education materials in multiple languages, such as translating information about “hipertension arterial” in English for Spanish-speaking patients, can ensure accessibility and inclusivity. However, beyond language, cultural norms about diet, family roles, and health literacy must be taken into account. A culturally competent educator will adapt communication styles and educational tools to resonate with the specific population being served.
Building trust is paramount. Patients are more likely to follow a high blood pressure care plan when they feel respected and understood. Educators should listen attentively, invite questions, and avoid medical jargon that may alienate or confuse patients. Collaborating with community health workers, cultural liaisons, and bilingual professionals can enhance the effectiveness of patient hypertension education and bridge gaps in understanding.
Strategies for Effective Patient Teaching on HTN
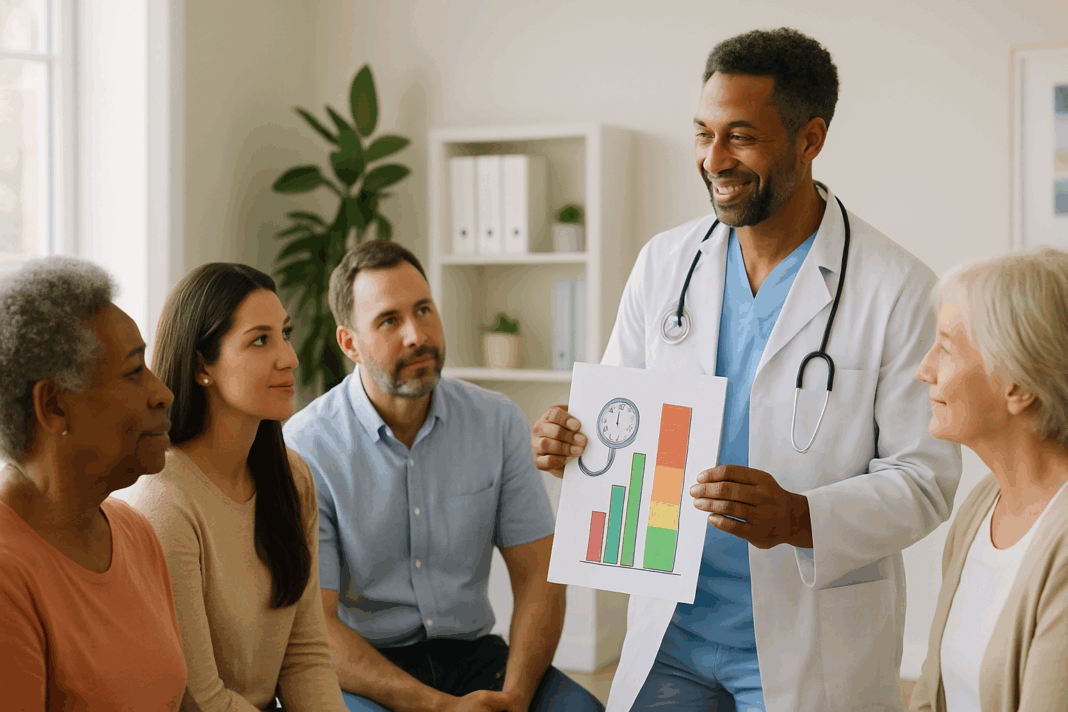
Teaching hypertension effectively means translating complex medical information into actionable insights that patients can apply in their daily lives. One proven strategy is the use of visual aids, such as diagrams showing how high blood pressure damages arteries or illustrations of heart anatomy. These tools can simplify abstract concepts and make learning more engaging.
Another technique is motivational interviewing, which helps patients explore their ambivalence about change and identify their own reasons for improving blood pressure control. When educators adopt a coaching mindset rather than a directive one, patients are more likely to internalize the importance of lifestyle changes. Asking open-ended questions like, “How might you educate a patient about high blood pressure if you were in my shoes?” can foster empathy and encourage personal reflection.
Repetition and reinforcement are key. Blood pressure education for patients should not rely on a single conversation or handout. Instead, concepts should be revisited regularly during follow-up visits, with adjustments made based on the patient’s progress and feedback. Digital platforms, such as patient portals and mobile apps, can support ongoing education by offering reminders, tracking tools, and interactive modules.
Involving family members can also enhance learning. Family dynamics often influence health behaviors, and including spouses or caregivers in the teaching process ensures that the patient has a strong support system. This is especially valuable in elderly populations or individuals with cognitive impairments who may need assistance with medication adherence or appointment scheduling.

Preventive Approaches and HTN Education
HTN prevention begins with awareness, and education is the foundation of prevention efforts. Many people are unaware they have high blood pressure until complications arise, making early screening and proactive teaching crucial. Public health campaigns and school-based programs can play a significant role in educating communities about the risk factors for hypertension and promoting heart-healthy habits.
HTN education should emphasize primary prevention strategies such as maintaining a healthy weight, eating a low-sodium diet, exercising regularly, limiting alcohol consumption, and avoiding tobacco use. These lifestyle choices are often shaped by environmental and socioeconomic factors, so educational efforts must also advocate for systemic changes that make healthy living accessible to all.
Educators must help patients understand that even small changes can yield significant health benefits. For example, losing just 10 pounds can lower blood pressure in overweight individuals. Framing goals as achievable and rewarding can increase motivation and adherence. Teaching hypertension prevention should begin early in life and continue across the lifespan, adapting to different stages and life events that may influence risk, such as pregnancy or menopause.
Clinical Guidelines and Protocols for High Blood Pressure Management
Standardized clinical guidelines serve as the backbone for high blood pressure management and education. Organizations like the American Heart Association and the American College of Cardiology provide evidence-based protocols that clinicians can follow to ensure consistency and quality in patient care. These protocols for high blood pressure address when to initiate pharmacologic treatment, how to monitor response, and when to escalate care.
Patient teaching for hypertension should include a discussion of these guidelines, especially when patients are prescribed new medications or require changes in their treatment regimen. Explaining the rationale behind guideline-based decisions increases transparency and trust, helping patients understand that recommendations are grounded in scientific evidence rather than arbitrary judgment.
Furthermore, protocols emphasize the importance of home monitoring. Teaching patients how to use automated blood pressure cuffs correctly, and how to interpret their readings, empowers them to participate actively in their care. Incorporating self-monitoring into the high blood pressure care plan fosters accountability and allows for early detection of any issues that might require medical attention.

Using Technology to Enhance Blood Pressure Education
Digital health technology is rapidly transforming the landscape of patient education. Mobile apps, wearable devices, and telehealth platforms offer innovative ways to deliver tailored information and support behavior change. For patients with limited access to in-person visits, these tools can be especially valuable.
Apps designed for hypertension management can track blood pressure readings, remind patients to take their medications, and offer tips on nutrition, exercise, and stress reduction. Interactive features such as goal setting, progress tracking, and educational videos make learning more engaging and user-friendly. This form of high blood pressure teaching meets patients where they are, offering support in real-time and in the comfort of their own homes.
Telehealth visits provide an opportunity for virtual patient teaching on HTN, especially for those in rural or underserved areas. Video consultations can replicate the personal connection of in-office visits while allowing for greater convenience and flexibility. These sessions can include visual demonstrations, screen sharing of educational materials, and collaborative development of care plans.
As digital tools become more sophisticated, the integration of artificial intelligence and machine learning may allow for even more personalized education. By analyzing patient data, these systems can identify learning needs and deliver customized content. However, educators must ensure that technology supplements rather than replaces human interaction, maintaining empathy and understanding as central components of care.
Evaluating the Impact of Hypertension Education on Health Outcomes
Measuring the effectiveness of hypertension education is essential for continuous improvement. Metrics such as medication adherence rates, blood pressure control, hospital readmissions, and patient satisfaction can provide insight into the success of educational interventions. Regular assessment allows clinicians to refine their teaching methods and address any gaps in understanding.
Qualitative feedback from patients is equally important. Understanding how patients perceive the education they receive, and how it influences their behavior, can inform future strategies. Focus groups, surveys, and individual interviews are useful tools for gathering this information.
Collaborative care models that include nurses, pharmacists, dietitians, and health educators tend to yield better outcomes. These interdisciplinary teams can deliver comprehensive education that addresses all aspects of hypertension management. For example, a pharmacist may focus on medication adherence while a dietitian provides guidance on sodium intake, all reinforcing the same core messages.
Ultimately, the goal of hypertension patient education is not just to lower blood pressure numbers, but to improve quality of life, reduce complications, and empower patients to take ownership of their health. When education is personalized, evidence-based, and delivered with compassion, it can be a powerful tool in the fight against cardiovascular disease.
Frequently Asked Questions: Advanced Insights on Hypertension Patient Education
1. What are the psychological barriers that may affect a patient’s ability to follow a high blood pressure care plan?
Many individuals with hypertension struggle with psychological resistance to long-term treatment, particularly when the condition appears symptomless. This disconnect between perception and medical reality can reduce a patient’s motivation to adhere to a high blood pressure care plan. Emotional states such as denial, anxiety, or learned helplessness may also interfere with behavior change. Effective hypertension education should acknowledge these psychological dynamics and provide coping strategies tailored to individual emotional profiles. By embedding psychological support into blood pressure education for patients, clinicians can build trust and encourage a more resilient mindset around chronic disease management.
2. How might cultural values influence patient teaching for hypertension in diverse populations?
Cultural beliefs significantly shape how individuals interpret medical advice and respond to hypertension education. For example, dietary recommendations may conflict with traditional cuisine, or there may be reliance on herbal remedies in lieu of prescribed medications. To improve the effectiveness of patient teaching for hypertension, educators should approach cultural differences with sensitivity and curiosity rather than judgment. Integrating familiar concepts or community influencers into health education for hypertensive patients can help bridge the gap between medical guidelines and personal beliefs. This culturally informed approach to high blood pressure teaching fosters a collaborative, respectful dynamic that enhances outcomes.
3. In what ways can family involvement enhance education for high blood pressure?
Family members often play a pivotal role in shaping daily habits and supporting medical adherence. When education for high blood pressure is extended to include a patient’s immediate support system, the likelihood of sustained behavior change increases. For instance, family members can assist with medication reminders, dietary adjustments, and emotional encouragement. Patient hypertension education that acknowledges the family context enables caregivers to become proactive allies rather than passive observers. Educating the family reinforces shared accountability, improves health literacy across the household, and may even serve as a form of HTN prevention for at-risk relatives.
4. How does socioeconomic status impact access to effective hypertension education?
Socioeconomic factors often determine whether a patient receives comprehensive hypertension patient education. Those living in under-resourced communities may face barriers such as limited access to clinics, healthy food options, or insurance coverage. For these individuals, a standard protocol for high blood pressure may be insufficient without practical solutions that account for financial and environmental constraints. Creative approaches like community health outreach programs, sliding-scale services, or mobile clinics can help democratize patient teaching on HTN. Equity-focused blood pressure education for patients ensures that information is not just available, but truly accessible and actionable.
5. What role do wearable technologies play in supporting hypertension education outside the clinic?
Wearables, such as smartwatches and fitness trackers, have introduced a new dimension to HTN education. These devices allow patient hypertension monitoring in real-time, offering instant feedback on heart rate, physical activity, and even sleep patterns. When integrated into a high blood pressure care plan, wearable technology can reinforce daily engagement with lifestyle goals and medication adherence. Educators can use the data collected from these tools to tailor hypertension education based on actual behaviors, rather than estimates or assumptions. This real-time interaction empowers patients with a deeper understanding of how daily decisions affect their blood pressure control.
6. Can community-based education programs contribute to long-term hypertension management?
Yes, grassroots-level hypertension patient education can be instrumental in managing the condition, especially in high-risk or underserved populations. Community health programs can provide group education sessions, blood pressure screenings, and referrals in a culturally relevant and trusted setting. These programs often employ lay health workers or peer educators, who can communicate complex medical information using relatable language and local context. By embedding high blood pressure teaching within community frameworks, these initiatives foster greater engagement and continuity than clinical interventions alone. Such initiatives also promote HTN prevention by creating widespread awareness and encouraging early detection.
7. How can clinicians assess whether their patient teaching on HTN is actually effective?
It is not enough to deliver education—clinicians must ensure it is understood and retained. One effective method is the “teach-back” approach, where patients explain in their own words what they have learned. This technique helps identify gaps in knowledge and reinforces comprehension in real time. Clinicians can also track biometric data, such as home blood pressure logs, alongside behavioral markers like medication adherence and lifestyle changes. Feedback forms and satisfaction surveys may further reveal how patients perceive the quality and clarity of blood pressure education. Regularly revisiting and adapting the hypertension education strategy based on these insights ensures a personalized, results-driven approach.
8. What are emerging trends in digital health that support blood pressure education for patients?
The digital health landscape is rapidly evolving to support hypertension education through mobile apps, telehealth, and AI-driven coaching. Some platforms now use gamification to keep users engaged, while others provide tailored reminders for medication and activity tracking. Advanced systems even analyze user data to deliver customized suggestions aligned with a patient’s high blood pressure care plan. For patients managing hipertension arterial in English or other languages, multilingual interfaces make these tools even more inclusive. This evolution toward personalized, tech-enabled HTN education marks a promising step toward broader public health impact.
9. How might you educate a patient about high blood pressure in a time-constrained clinical setting?
In fast-paced clinical environments, concise yet impactful communication is key. Prioritizing the most critical aspects of patient teaching on HTN—such as the importance of medication adherence, dietary changes, and self-monitoring—can be achieved in just a few minutes with the right tools. Handouts, QR codes linking to videos, or digital follow-up messages can extend the conversation beyond the appointment. Clinicians might ask, “How might you educate a patient about high BP if you had only five minutes?” and tailor their delivery accordingly. Even brief hypertension education sessions, when focused and strategic, can spark meaningful changes and motivate deeper engagement.
10. What should health educators know about addressing language diversity in hypertension education?
Language can be a powerful enabler or barrier in high blood pressure patient education. When communicating with non-native English speakers, translating terms like “hipertension arterial” into English is only the first step. True comprehension requires adapting the tone, idioms, and examples to fit the patient’s cultural and linguistic context. Bilingual educators, translated materials, and medical interpreters are essential resources in this process. Moreover, education for high blood pressure should consider the literacy levels of patients and avoid overly technical language. A patient-centered approach to language ensures that blood pressure education for patients is both linguistically and conceptually accessible, ultimately improving health outcomes.
Conclusion: Empowering Patients Through Evidence-Based Hypertension Education
High blood pressure is one of the most common yet controllable cardiovascular conditions. Through effective, personalized, and culturally competent patient hypertension education, clinicians can help individuals navigate the complexities of diagnosis, treatment, and long-term management. When education for high blood pressure is integrated seamlessly into the patient experience, it fosters understanding, encourages behavior change, and builds the foundation for sustained wellness.
From designing a high blood pressure care plan to incorporating digital tools and following clinical protocols, the key to successful management lies in how well patients are taught to engage with their health. Whether through structured office visits, telehealth sessions, or community outreach programs, the importance of health education for hypertensive patients cannot be overstated. Thoughtfully delivered patient teaching on HTN promotes trust, reduces disparities, and improves outcomes across diverse populations.
As we look toward the future of cardiovascular care, investing in comprehensive blood pressure education for patients will remain a top priority. This approach not only supports immediate clinical goals but also contributes to long-term public health efforts aimed at reducing the global burden of hypertension. Empowered patients, guided by evidence-based teaching, are better equipped to take control of their blood pressure and their lives.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Guideline-Driven Management of Hypertension: An Evidence-Based Update
Guideline-Driven Management of Hypertension: An Evidence-Based Update