Introduction: A New Era in Lung Cancer Treatment
In recent years, the medical community has witnessed a remarkable evolution in the way lung cancer is treated. One of the most promising advances in this domain is the rise of proton therapy for lung cancer. As radiation oncology shifts toward increasingly precise and patient-tailored approaches, proton beam therapy for lung cancer stands out as a beacon of innovation, offering a new standard in targeting tumors while sparing surrounding healthy tissues. This article explores the science, benefits, clinical applications, ongoing research, and future potential of this groundbreaking treatment.
You may also like: Cancer Research Breakthroughs: How Modern Advancements Are Transforming Treatment
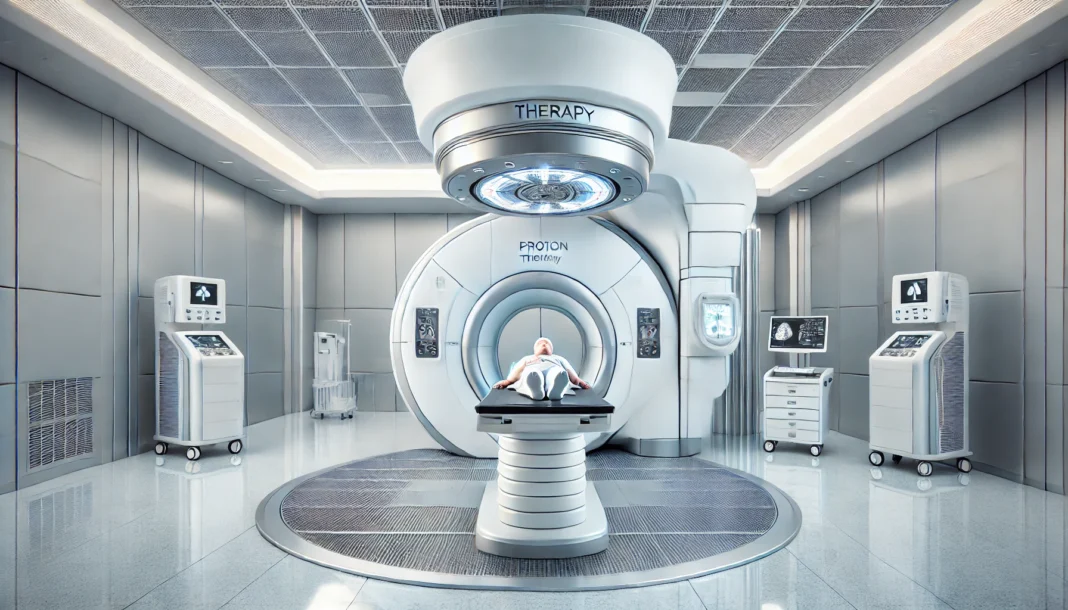
Understanding the Principles Behind Proton Therapy
To appreciate the impact of proton radiation therapy for lung cancer, it is essential first to understand the basic mechanics behind it. Unlike conventional radiation therapy that uses high-energy X-rays, proton therapy employs positively charged particles known as protons. These protons are accelerated to high speeds and directed toward cancerous tissues, delivering energy directly to the tumor. One of the defining characteristics of proton therapy is its ability to deposit maximum energy at a specific depth in the body—a phenomenon known as the Bragg peak.
This distinctive feature enables proton treatment for lung cancer to concentrate its destructive power on the tumor while significantly reducing radiation exposure to nearby organs such as the heart, esophagus, and spinal cord. As a result, proton therapy offers a major advantage over traditional photon therapy for lung cancer, which tends to scatter energy as it passes through the body. This precision translates into fewer side effects, reduced risk of long-term complications, and potentially better outcomes for patients.
Comparing Proton Therapy and Photon Therapy for Lung Cancer
When evaluating proton beam therapy for lung cancer against photon therapy, one must consider both clinical efficacy and quality of life outcomes. Photon therapy, long regarded as the standard of care, uses X-rays that release energy along their entire path through the body. This often means healthy tissues surrounding the tumor receive unintended radiation exposure, leading to increased toxicity.
Proton therapy mitigates this concern by confining the majority of its radiation dose to the tumor itself. Several studies have demonstrated that proton radiation for lung cancer can result in fewer cases of radiation pneumonitis, esophagitis, and cardiac toxicity. Moreover, for patients with compromised lung function or coexisting cardiac conditions, this precision becomes more than a technological luxury—it becomes a medical necessity.

The Clinical Application of Proton Radiation for Lung Cancer
Clinicians are increasingly turning to proton therapy for lung cancer as a frontline or adjunctive treatment, particularly in complex cases. Non-small cell lung cancer (NSCLC), the most common type of lung cancer, has shown favorable responses to proton-based regimens. Studies from leading cancer centers have revealed that proton beam therapy for lung cancer can be effective as both a definitive and neoadjuvant treatment, especially when combined with chemotherapy.
Another key area of application is in reirradiation scenarios. Patients who have previously undergone photon therapy and experienced disease recurrence often have limited options due to cumulative radiation toxicity. Proton radiation therapy for lung cancer offers a viable solution in such situations, allowing oncologists to target recurrent tumors while minimizing further damage to previously irradiated tissues.
Reducing Long-Term Side Effects and Enhancing Recovery
The long-term health of lung cancer survivors is increasingly being prioritized as survival rates improve. One of the major goals in oncologic care today is to not only prolong life but also to enhance its quality. Proton radiation for lung cancer aligns perfectly with this objective by offering a reduced side-effect profile.
Traditional radiation methods can lead to chronic complications, including fibrosis, chronic cough, and cardiac dysfunction. With proton therapy, the collateral impact on surrounding structures is significantly reduced, allowing patients to maintain better pulmonary and cardiovascular function post-treatment. This advantage is especially relevant for elderly patients or those with underlying lung disease, who may not tolerate the cumulative effects of photon therapy as well.
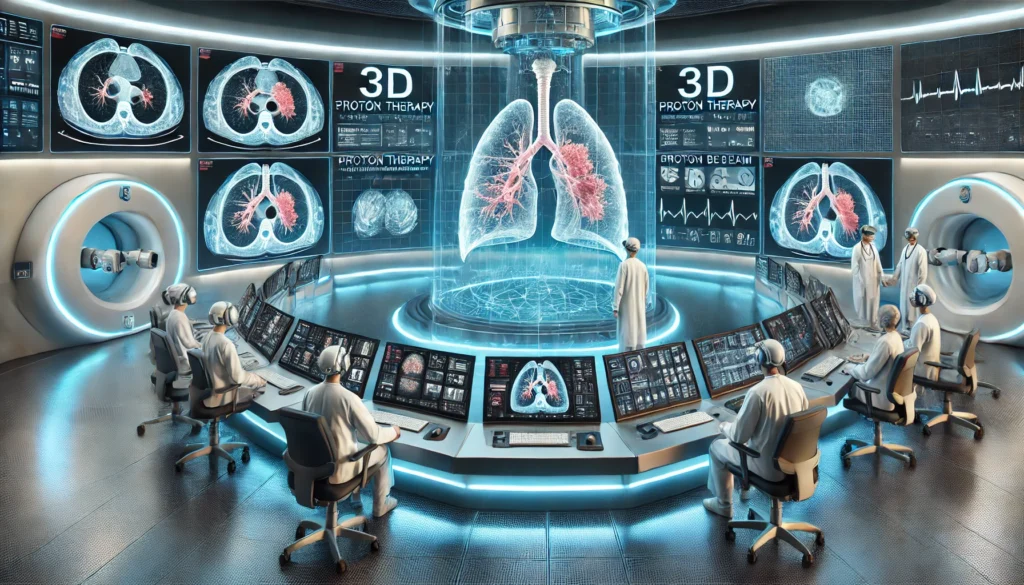
Technological Advancements Driving Proton Therapy
The current landscape of proton beam therapy for lung cancer is being shaped by rapid technological innovation. The development of pencil beam scanning (PBS), for instance, has elevated the precision of proton delivery by allowing clinicians to sculpt radiation doses in three dimensions. This technique enables adaptive treatment planning that accounts for respiratory motion, tumor shrinkage, and anatomical changes throughout the course of therapy.
Advanced imaging tools, such as 4D CT scans and MRI-guided planning systems, have also enhanced the accuracy of proton treatment for lung cancer. These tools allow for real-time tracking of tumor motion caused by breathing, which is particularly important for lung tumors that shift position during inhalation and exhalation. By synchronizing radiation delivery with the respiratory cycle, clinicians can further reduce the dose to healthy tissues.
Artificial intelligence and machine learning are beginning to play a pivotal role in optimizing proton therapy workflows. AI algorithms are being used to predict tumor responses, adjust treatment plans dynamically, and streamline quality assurance processes. These innovations are helping to make proton radiation therapy for lung cancer more efficient, individualized, and accessible.
Integrating Proton Therapy into Multimodal Lung Cancer Treatment
Lung cancer treatment is rarely a single-modality endeavor. The integration of proton radiation therapy for lung cancer into multimodal regimens—including surgery, chemotherapy, and immunotherapy—has become an area of active investigation. For instance, several trials are exploring the synergy between proton therapy and immune checkpoint inhibitors, examining whether the reduced inflammation from proton treatment may enhance immune responses.
In surgical candidates, preoperative proton therapy can be used to shrink tumors and facilitate less invasive procedures. Conversely, in inoperable cases, proton therapy can serve as a definitive modality, providing high-dose radiation to tumors that cannot be removed surgically. Combining proton beam therapy for lung cancer with systemic treatments also opens new avenues for controlling micrometastatic disease and reducing the likelihood of recurrence.
Personalized treatment planning is essential to the success of these multimodal strategies. By tailoring radiation protocols to the individual biology and tumor characteristics of each patient, clinicians can optimize outcomes while minimizing toxicity. This patient-centered approach exemplifies the future of precision oncology.
Patient Perspectives and Quality of Life Outcomes
Beyond the technical and clinical dimensions, the patient experience with proton therapy for lung cancer deserves special attention. Studies and patient testimonials consistently highlight the improved tolerability and reduced side effects associated with proton therapy compared to photon-based alternatives. Many patients report fewer symptoms during treatment, such as fatigue, nausea, and skin irritation.
Maintaining the ability to work, care for family members, and engage in daily activities can significantly impact a patient’s emotional well-being and overall recovery. Proton treatment for lung cancer has been associated with lower rates of treatment interruptions, which not only benefits patients’ physical health but also their psychological resilience.
Patient satisfaction metrics and quality of life surveys are increasingly being incorporated into clinical trials, underscoring the importance of holistic outcomes in cancer care. These data reinforce the value of proton radiation therapy not only as a curative tool but also as a means of supporting patients’ dignity and autonomy during a challenging period of their lives.
Frequently Asked Questions: Proton Therapy for Lung Cancer
1. Can proton therapy be used for early-stage lung cancer, or is it only for advanced cases?
Proton therapy for lung cancer is increasingly being used across a broad spectrum of disease stages, including early-stage cases. While it is most commonly applied in complex or advanced-stage scenarios, researchers are now exploring its potential in early-stage tumors, especially for patients who are not good candidates for surgery due to age or comorbidities. In early-stage settings, proton beam therapy for lung cancer can serve as a highly targeted treatment, delivering curative doses with minimal damage to surrounding tissues. Emerging evidence suggests that proton radiation for lung cancer could offer superior local control and fewer side effects compared to traditional approaches, particularly for tumors near sensitive structures. This expanding role in early-stage care demonstrates the growing flexibility and precision of proton radiation therapy for lung cancer.
2. How does the recovery process differ after proton therapy compared to photon therapy?
Recovery after proton therapy for lung cancer is often smoother and faster than recovery after photon therapy for lung cancer. Because proton radiation minimizes exposure to healthy tissues, patients typically experience less fatigue, fewer respiratory complications, and a quicker return to daily activities. This can be especially important for patients who need to maintain employment or caregiving responsibilities during or after treatment. In contrast, photon therapy for lung cancer may lead to more prolonged inflammation or collateral tissue damage, potentially lengthening recovery time. While every patient’s experience is unique, clinical trends show that proton radiation therapy for lung cancer is generally associated with a more favorable post-treatment recovery profile.
3. Are there long-term cognitive or psychological effects associated with proton radiation for lung cancer?
Although the lungs are distant from the brain, long-term cognitive and psychological effects of cancer treatment—including anxiety, depression, and “chemo brain”—are increasingly being recognized. With proton radiation for lung cancer, reduced systemic inflammation and lower toxicity levels may help preserve overall neurological well-being. Some patients report fewer neurocognitive disruptions when treated with proton beam therapy for lung cancer, likely because their bodies are less stressed by inflammation or prolonged physical recovery. Mental health support and cognitive rehabilitation remain essential, but proton treatment for lung cancer may allow patients to better maintain psychological resilience. Future studies may further quantify these benefits and validate the role of proton therapy in supporting both physical and cognitive recovery.
4. How does proton therapy impact fertility or hormonal health in younger lung cancer patients?
Though lung cancer primarily affects older adults, younger patients may still face unique concerns related to fertility and hormonal health. Proton therapy for lung cancer offers a potential advantage in this regard by minimizing radiation exposure to distant organs, including reproductive structures and endocrine glands. In contrast, photon therapy for lung cancer may expose the body to more scatter radiation, which, over time or in high doses, could impact hormonal balance. For adolescent or premenopausal women with thoracic tumors, proton radiation therapy for lung cancer could reduce the risk of premature menopause or hormonal disruption. While fertility preservation remains a complex issue, the precision of proton radiation helps make future family planning more viable for younger survivors.
5. Can patients with pacemakers or implanted cardiac devices undergo proton treatment safely?
Patients with pacemakers or implantable cardioverter-defibrillators (ICDs) often face challenges when receiving radiation, as electromagnetic interference or radiation scatter can affect device function. Proton therapy for lung cancer may be safer for such individuals because of its ability to limit stray radiation exposure. Compared to photon therapy for lung cancer, which may deliver unintended doses to cardiac regions, proton beam therapy offers a more controlled and confined radiation field. Institutions with proton radiation therapy for lung cancer expertise often have protocols to protect device integrity while ensuring therapeutic efficacy. Collaboration between radiation oncologists and cardiologists is essential to customize treatment and monitor device function throughout the process.
6. What are the environmental and safety considerations for proton therapy facilities?
Proton therapy centers require advanced infrastructure, including cyclotrons or synchrotrons to accelerate particles. These facilities must adhere to strict safety standards due to the energy levels involved, but modern engineering has made them remarkably secure for both patients and medical staff. Unlike photon therapy machines, which produce radiation as a byproduct of electricity, proton treatment for lung cancer uses a highly focused beam that is precisely modulated and controlled. Shielding, maintenance protocols, and real-time safety monitoring are integral to the operation of proton radiation therapy centers. From an environmental perspective, proton therapy produces no radioactive waste, making it a cleaner alternative to some other radiation modalities.
7. Are there nutritional or lifestyle recommendations specific to proton therapy patients?
While no exclusive diet is required, patients receiving proton radiation for lung cancer often benefit from anti-inflammatory and immune-supportive diets. Foods rich in antioxidants—like berries, leafy greens, and omega-3 fatty acids—can support tissue repair and reduce oxidative stress during treatment. Staying hydrated and maintaining adequate protein intake also helps the body recover more efficiently from proton radiation therapy for lung cancer. Unlike some chemotherapy protocols, proton beam therapy for lung cancer typically does not cause severe nausea or taste changes, allowing patients to better adhere to nutritional plans. Moderate physical activity, stress reduction techniques, and sleep hygiene are also encouraged to support overall resilience during proton treatment for lung cancer.
8. How does proton therapy interact with emerging forms of immunotherapy?
The relationship between radiation and the immune system is an exciting frontier in oncology. Proton therapy for lung cancer may work synergistically with immunotherapy agents by reducing tumor burden while preserving the immune system’s functionality. Some researchers believe that the reduced inflammation and collateral damage from proton radiation may actually enhance immune surveillance and response. In contrast, photon therapy for lung cancer may provoke broader systemic inflammation, potentially interfering with immune modulation. Clinical trials are currently evaluating how proton radiation therapy for lung cancer can be timed and dosed alongside immune checkpoint inhibitors for optimal results. These combinations could redefine the landscape of non-invasive, curative-intent lung cancer treatment.
9. Are there differences in patient outcomes between community hospitals and academic centers offering proton therapy?
Outcomes for proton treatment for lung cancer may vary depending on institutional experience, access to advanced imaging, and availability of multidisciplinary teams. Academic and NCI-designated cancer centers often have more robust protocols and specialized staff trained specifically in proton beam therapy for lung cancer. These centers are also more likely to participate in clinical trials, offer adaptive radiation planning, and integrate supportive services like nutritional counseling and psychosocial care. However, community hospitals with proton facilities are increasingly closing the gap by adopting best practices and collaborating with larger institutions. Patients should evaluate factors such as team experience, technology, and patient support when choosing a center for proton radiation therapy for lung cancer.
10. What are some of the most promising future innovations in proton therapy for lung cancer?
The future of proton therapy for lung cancer includes technological and biological innovations that could drastically improve outcomes. FLASH proton therapy, which delivers ultra-high dose rates in milliseconds, is under investigation for its potential to kill tumors while further reducing side effects. Imaging-guided adaptive planning will continue to evolve, allowing clinicians to adjust treatment in real time based on tumor movement or shrinkage. Personalized dosing algorithms based on genetic or molecular tumor profiling may optimize the effectiveness of proton beam therapy for lung cancer. Moreover, advances in telemedicine and AI-driven planning are making proton radiation therapy for lung cancer more accessible and cost-effective. These breakthroughs represent a future where precision, convenience, and efficacy coalesce to transform the patient experience.

Conclusion: Why Proton Therapy for Lung Cancer Is Poised to Revolutionize Patient Outcomes
The emergence of proton therapy for lung cancer represents a transformative shift in radiation oncology—one that holds the promise of improved outcomes, fewer side effects, and more personalized care. As the technology continues to advance and access expands, the clinical community is poised to redefine the standard of care for many patients.
While challenges related to cost, accessibility, and long-term data remain, the momentum behind proton beam therapy for lung cancer is undeniable. From enhancing survival in advanced cases to preserving quality of life in survivors, proton radiation therapy offers a beacon of hope in a field where innovation is urgently needed.
Looking ahead, continued research, patient advocacy, and technological refinement will be key to unlocking the full potential of proton treatment for lung cancer. As clinicians, researchers, and patients converge around this promising modality, a new chapter in lung cancer care is being written—one defined by precision, compassion, and a steadfast commitment to better outcomes.
advanced lung cancer treatment, precision radiation therapy, non-invasive cancer treatment, targeted radiation therapy, lung tumor management, cancer survivorship care, radiation side effects reduction, high-dose radiation therapy, thoracic oncology innovations, personalized lung cancer care, radiation therapy advancements, lung cancer radiation options, cancer treatment recovery, radiation-induced toxicity, multidisciplinary cancer treatment, emerging cancer therapies, reirradiation techniques in oncology, high-risk lung cancer patients, novel cancer treatment technologies, cancer care quality of life
Further Reading:
4 advances in radiation therapy for lung cancer treatment
Proton Therapy: The New Weapon to Fight Cancer
Treating Lung Cancer with Proton Therapy
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.