Type 2 diabetes is no longer a distant concern; it has become a global health emergency. Once considered a chronic disease affecting only older adults, this form of diabetes now increasingly impacts younger individuals and even children, primarily due to sedentary lifestyles, poor nutrition, and rising obesity rates. According to the International Diabetes Federation, over 530 million people worldwide live with diabetes, the vast majority of whom have type 2. But here’s the crucial takeaway: type 2 diabetes is largely preventable. Emerging research offers promising insights into how to prevent type two diabetes, shedding light on novel strategies and lifestyle interventions that go far beyond the traditional diet and exercise advice.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
This article dives deep into the scientific breakthroughs and evidence-backed techniques that can help individuals reclaim control over their metabolic health. From microbiome modulation and time-restricted eating to targeted nutraceuticals and precision medicine, these innovations are redefining how to combat type 2 diabetes. We’ll also explore how the latest research validates age-old practices like sleep hygiene, stress management, and plant-based nutrition—reframing them as potent tools for diabetes 2 prevention. Whether you’re at risk for prediabetes or seeking ways to support loved ones, this article offers a comprehensive look at what truly works when it comes to avoiding type 2 diabetes in a modern world.
Understanding the Modern Diabetes Epidemic: Why Prevention Matters Now More Than Ever
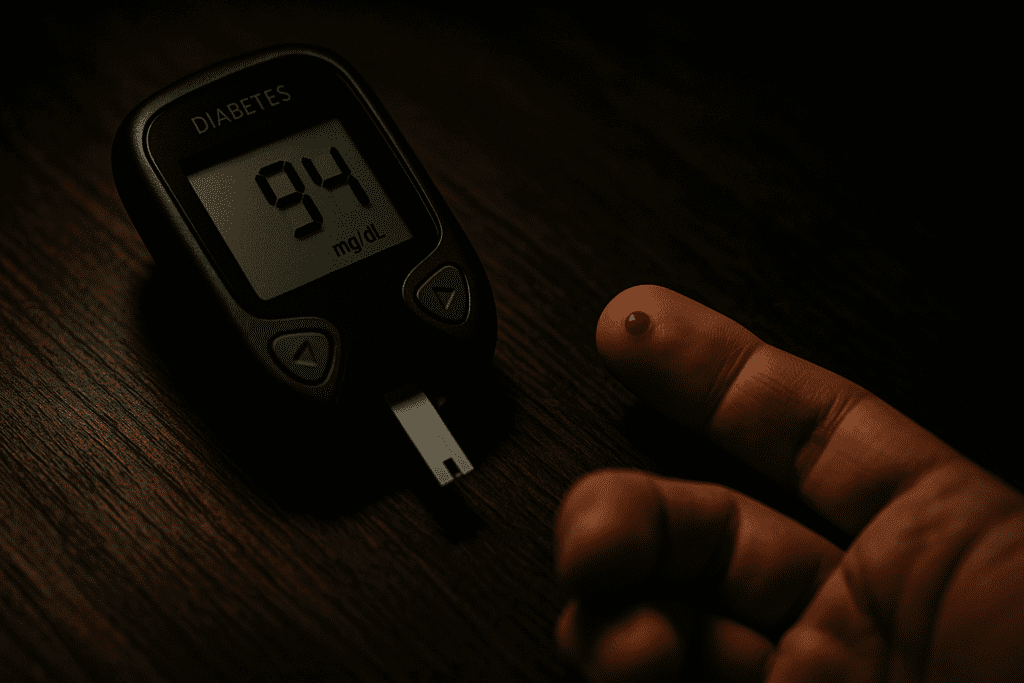
Before diving into prevention strategies, it’s important to understand what makes type 2 diabetes such a complex and growing threat. This condition is characterized by insulin resistance—a state where the body’s cells no longer respond effectively to insulin, leading to elevated blood glucose levels. Over time, the pancreas cannot keep up with insulin demand, resulting in persistently high blood sugar that damages blood vessels, nerves, and organs.
Unlike type 1 diabetes, which is autoimmune in nature, type 2 develops gradually and is strongly linked to modifiable lifestyle factors. That’s what makes the question “is diabetes type 2 preventable?” so critical. The answer from leading medical organizations is a resounding yes. Up to 90% of type 2 diabetes cases can be delayed or prevented altogether through evidence-based lifestyle interventions. While genetics and age play a role, they are often overshadowed by daily habits and exposures that either trigger or shield us from metabolic dysfunction.
New studies have even revealed that early metabolic warning signs can appear decades before diagnosis. These include insulin resistance, abdominal obesity, elevated fasting insulin, and chronic low-grade inflammation. Recognizing these red flags early empowers individuals to intervene before glucose levels spiral out of control. This is why understanding how to diabetes prevention works—on a biological, behavioral, and societal level—is one of the most urgent public health priorities of our time.
Rethinking Nutrition: The Science Behind Blood Sugar Stability and Dietary Interventions
One of the most researched and effective approaches to diabetes 2 prevention is dietary modification. But this doesn’t simply mean “cutting carbs” or adopting a generic low-sugar diet. Emerging studies suggest that the quality and timing of food intake play a much bigger role in blood sugar regulation than previously thought. For instance, high-fiber diets rich in whole grains, legumes, and vegetables have been shown to improve insulin sensitivity and reduce post-meal glucose spikes. This is due to fiber’s ability to slow gastric emptying and blunt glucose absorption, making it a foundational component of type 2 diabetes home treatment as well as prevention.
But more recent research has shifted attention to the microbiome—the community of trillions of bacteria in our gut. Certain dietary patterns, particularly those rich in polyphenols and prebiotics, can encourage the growth of beneficial microbes that influence glucose metabolism. In randomized clinical trials, individuals consuming a Mediterranean-style diet—abundant in olive oil, nuts, fish, and vegetables—demonstrated significantly lower rates of type 2 diabetes over time. This eating pattern reduces oxidative stress, improves lipid profiles, and dampens inflammation—all of which are implicated in insulin resistance.
Additionally, meal timing is gaining traction as a key factor. Time-restricted eating, a form of intermittent fasting where meals are confined to a specific window (typically 8–10 hours), has been shown to improve insulin sensitivity and reduce fasting glucose even in people without weight loss. This challenges the traditional focus on caloric intake and encourages a broader view of how to avoid diabetes mellitus by respecting the body’s circadian rhythm.
The Role of Physical Activity in Preventing Type 2 Diabetes
Exercise is not a new recommendation for avoiding type 2 diabetes, but recent studies reveal that the timing, intensity, and type of activity may matter more than once believed. Both aerobic and resistance training have profound impacts on glucose utilization, but their benefits go beyond mere calorie burning. High-intensity interval training (HIIT), for example, has been shown to significantly improve insulin sensitivity in as little as two weeks—making it a compelling option for type 2 diabetes home treatment in those with time constraints.
What’s particularly promising is the evidence that even small amounts of daily movement can prevent blood sugar spikes. Walking for just 10 minutes after meals significantly reduces postprandial glucose levels, especially in people with prediabetes. This means you don’t need to spend hours in the gym to protect your metabolic health—simple, frequent bouts of movement can go a long way.
Furthermore, exercise influences muscle glucose uptake independently of insulin. This means that even in states of insulin resistance, active muscles can pull glucose from the bloodstream, reducing blood sugar levels and giving the pancreas a much-needed break. This unique mechanism makes physical activity one of the most powerful non-pharmacologic tools in the fight against type 2 diabetes. Understanding how can we prevent type 2 diabetes through consistent, personalized physical activity is key to building sustainable health habits.
Targeting Visceral Fat: Why Belly Fat Is More Dangerous Than You Think
Among the most consistent predictors of type 2 diabetes risk is the accumulation of visceral fat—fat stored deep within the abdominal cavity around internal organs. Unlike subcutaneous fat, which lies just beneath the skin, visceral fat is highly metabolically active and releases inflammatory cytokines that disrupt insulin signaling. In fact, many researchers now consider visceral adiposity a central driver of insulin resistance, making it a crucial target in how to combat type 2 diabetes strategies.
Emerging imaging techniques have allowed researchers to assess visceral fat more precisely, linking even moderate increases to elevated glucose and insulin levels. Fortunately, visceral fat is also responsive to lifestyle interventions. Studies show that modest weight loss—just 5% to 10% of body weight—can produce dramatic improvements in insulin sensitivity and glycemic control, especially when fat is lost from the abdominal region.
Interestingly, not all weight loss approaches are equally effective in reducing visceral fat. Resistance training and low-carbohydrate diets tend to reduce visceral stores more efficiently than aerobic exercise alone. Integrating these strategies with intermittent fasting or calorie cycling may further enhance results. Thus, if you’re wondering how to prevent type two diabetes, reducing visceral fat through tailored nutrition and exercise is a vital place to start.
The Power of Sleep and Stress Management in Blood Sugar Control
It may come as a surprise, but sleep and stress are potent regulators of metabolic health—and neglecting either one can sabotage even the most disciplined efforts at diabetes 2 prevention. Numerous studies have linked short sleep duration and poor sleep quality with insulin resistance, elevated cortisol, and increased appetite for refined carbohydrates. These factors can accelerate the progression from prediabetes to full-blown type 2 diabetes.
Chronic stress also contributes to dysregulated blood sugar through its impact on cortisol, the body’s primary stress hormone. When cortisol levels remain elevated, glucose is continuously released into the bloodstream in anticipation of a “fight-or-flight” response, even if no actual physical danger is present. This leads to a constant state of hyperglycemia and inflammation, which undermines insulin’s effectiveness over time.
Mind-body interventions like yoga, meditation, breathwork, and tai chi have been shown to lower fasting glucose and improve insulin sensitivity in high-risk populations. Improving sleep hygiene—such as establishing a consistent bedtime, avoiding blue light at night, and managing sleep apnea—has also demonstrated protective effects. These findings reinforce that understanding how to diabetes prevention works involves more than food and exercise. Emotional and circadian wellness are equally essential to metabolic balance.
Exploring Nutraceuticals and Supplements in Diabetes Prevention
While lifestyle remains the cornerstone of how to prevent diabetes mellitus type 2, research into nutraceuticals—compounds derived from food that provide health benefits—is uncovering promising new adjuncts. Certain supplements, when used appropriately, can help regulate glucose metabolism and reduce diabetes risk. Among the most studied are magnesium, berberine, alpha-lipoic acid, and vitamin D.
Magnesium plays a crucial role in insulin receptor function and glucose transport. Studies show that low magnesium intake is associated with a higher risk of developing type 2 diabetes, and supplementation can improve insulin sensitivity, particularly in those who are deficient. Berberine, a compound found in several plants, has demonstrated effects comparable to metformin in lowering blood glucose and improving lipid profiles. Unlike pharmaceuticals, however, it may offer additional benefits in modulating the gut microbiota and reducing systemic inflammation.
Alpha-lipoic acid is another potent antioxidant that enhances insulin sensitivity and reduces oxidative stress, while vitamin D has been linked to improved beta-cell function and lower rates of insulin resistance. Though these compounds are not substitutes for lifestyle changes, they may serve as powerful allies for those looking to bolster their defenses. For individuals seeking ways to prevent type 2 diabetes or complement existing strategies, evidence-based nutraceuticals may hold promise—when used under medical supervision.
Precision Medicine and the Future of Diabetes Prevention
The future of diabetes prevention is becoming increasingly personalized. Advances in genomics, metabolomics, and digital health are enabling clinicians to create customized prevention plans based on an individual’s genetic risk, metabolic profile, and lifestyle habits. For example, genetic testing can identify polymorphisms associated with insulin resistance or impaired beta-cell function, allowing for earlier interventions tailored to one’s unique biology.
Wearable devices and continuous glucose monitors (CGMs) are also revolutionizing how we understand blood sugar dynamics. By tracking glucose in real time, users can identify which foods or habits cause spikes and adjust accordingly. This form of biofeedback fosters better decisions and a more nuanced understanding of how to avoid diabetes mellitus in daily life. Digital coaching platforms, AI-driven diet recommendations, and app-based lifestyle interventions are making personalized prevention more accessible than ever before.
Even the microbiome may soon be used to predict diabetes risk and inform prevention strategies. Some companies are already offering microbiome-based dietary advice to optimize metabolic health. These advancements underscore a pivotal shift: is diabetes a preventable disease? For most people, the answer increasingly lies in leveraging data to drive precision interventions that are both proactive and sustainable.
Redefining Prevention Through Public Health and Policy
While individual strategies for how to prevent type two diabetes are essential, real progress will also depend on broader systemic changes. Socioeconomic status, food access, healthcare disparities, and urban planning all influence diabetes risk at a population level. Policies that promote active transportation, regulate processed food marketing, and increase access to healthy food are just as important as individual behavior change.
Community-level interventions—such as group-based diabetes prevention programs, employer wellness initiatives, and culturally tailored education—have shown measurable success in reducing incidence rates. When supported by healthcare providers, insurance systems, and policy makers, these efforts scale far beyond what any single person can achieve alone. Understanding how can we prevent type 2 diabetes must therefore include a collective vision rooted in equity, accessibility, and shared responsibility.

Frequently Asked Questions: Emerging Research on How to Prevent Type Two Diabetes
1. What role does psychological resilience play in type 2 diabetes prevention?
Psychological resilience, or the ability to adapt to stress, plays a surprisingly important role in how to combat type 2 diabetes. Chronic psychological stress can elevate cortisol levels, leading to prolonged blood sugar imbalances and eventual insulin resistance. Resilience-focused interventions—such as cognitive behavioral therapy (CBT), mindfulness-based stress reduction, and self-compassion training—can lower stress hormone levels and improve glycemic regulation. People with high resilience also tend to adhere more effectively to diet and exercise routines, which strengthens their overall diabetes 2 prevention strategy. Incorporating mental wellness practices is a lesser-known yet highly effective part of how to diabetes prevention, especially in high-stress environments.
2. Can living at higher altitudes reduce the risk of developing type 2 diabetes?
Interestingly, epidemiological data show that people living at moderate altitudes may experience a reduced risk of type 2 diabetes compared to those living at sea level. This appears to be due to several mechanisms: reduced oxygen levels at altitude can enhance mitochondrial efficiency and increase insulin sensitivity. Moreover, cold exposure and increased physical exertion from mountainous environments may also contribute to more stable glucose metabolism. While not a mainstream strategy, environmental factors like altitude hint at novel directions in ways to prevent type 2 diabetes. It’s a compelling example of how lifestyle and location intersect in subtle but impactful ways when examining how to avoid diabetes mellitus.
3. How do oral health and gum disease affect type 2 diabetes risk?
Emerging evidence shows that poor oral health—particularly periodontal disease—can increase systemic inflammation, which plays a central role in insulin resistance. Gum infections allow bacteria to enter the bloodstream, triggering inflammatory responses that negatively impact glucose regulation. Regular dental care and treating gum disease early have been associated with improved glycemic control and even reduced HbA1c levels. This adds an unexpected layer to how to prevent diabetes mellitus type 2, highlighting oral hygiene as a practical and underappreciated preventive tool. Including dental evaluations in your broader metabolic health strategy may offer added protection in avoiding type 2 diabetes over time.
4. Are there specific sleep disorders that increase the risk of type 2 diabetes?
Yes, obstructive sleep apnea (OSA) is strongly linked to insulin resistance and higher risk of developing type 2 diabetes. When sleep is disrupted by repeated apneic episodes, oxygen levels drop, and stress hormones spike, which interferes with glucose metabolism. Continuous positive airway pressure (CPAP) therapy has been shown to improve insulin sensitivity and reduce fasting glucose in people with both OSA and prediabetes. Addressing sleep disorders is often overlooked in discussions about how to prevent type two diabetes, but treating them early can be a form of type 2 diabetes home treatment and a major preventive strategy. Prioritizing sleep assessments may be key for those experiencing chronic fatigue, snoring, or nighttime awakenings.
5. How do social determinants of health influence diabetes prevention efforts?
Social determinants—such as access to healthcare, income, education, housing, and food security—heavily shape a person’s ability to implement ways to prevent type 2 diabetes. Someone who lacks access to fresh produce or safe spaces for exercise may find it harder to follow conventional advice. Preventive interventions must therefore account for these broader socioeconomic conditions to be truly effective. Community-based programs, culturally adapted diets, and policy-level changes are critical components of how can we prevent type 2 diabetes at the population level. Recognizing the role of social inequity helps contextualize why is diabetes a preventable disease isn’t just a medical question—it’s also a societal one.
6. Are there technological tools that can help track progress in diabetes prevention?
Yes, a growing number of wearables and digital health platforms are helping individuals monitor real-time biomarkers related to glucose control. Devices like continuous glucose monitors (CGMs) allow users to see how their blood sugar responds to specific meals, sleep patterns, or stress triggers. Personalized feedback encourages behavior change and helps users make data-driven decisions—one of the most innovative methods in how to combat type 2 diabetes. Apps that track dietary intake, physical activity, and sleep also enable users to design comprehensive plans for diabetes 2 prevention. These technologies are transforming how we approach type 2 diabetes home treatment and enabling proactive, personalized care.
7. Can exposure to environmental toxins increase the risk of developing type 2 diabetes?
Yes, studies have begun linking long-term exposure to endocrine-disrupting chemicals (EDCs)—like bisphenol A (BPA), phthalates, and certain pesticides—with increased insulin resistance and beta-cell dysfunction. These substances interfere with hormonal regulation and glucose metabolism, subtly contributing to the onset of metabolic syndrome. Reducing exposure through safer plastics, filtered water, and organic produce may support how to avoid diabetes mellitus, especially when combined with other preventive practices. While more research is needed, environmental detoxification is gaining attention as a novel aspect of how to prevent diabetes mellitus type 2 in modern industrialized settings. This adds depth to our understanding of how to diabetes prevention in a polluted world.
8. What role does meal sequencing play in managing insulin response?
Meal sequencing refers to the order in which different types of food are consumed during a meal. Recent studies show that starting a meal with protein or fiber—such as vegetables or legumes—can blunt the glucose spike caused by carbohydrates consumed later. This strategy enhances satiety, reduces insulin demand, and has been effective even in those with impaired glucose tolerance. Meal sequencing is a practical, everyday tactic in how to prevent type two diabetes, requiring no calorie counting or restrictive dieting. For people exploring type 2 diabetes home treatment, optimizing food order could serve as a subtle yet powerful intervention.
9. How does menopause affect a woman’s risk of developing type 2 diabetes?
Menopause is associated with hormonal changes—particularly a drop in estrogen—that can lead to increased abdominal fat, reduced muscle mass, and insulin resistance. These shifts place postmenopausal women at heightened risk for type 2 diabetes, especially if they already exhibit features of metabolic syndrome. Hormone replacement therapy (HRT), when used judiciously, has been shown to improve insulin sensitivity and lipid profiles in some women. Understanding these gender-specific risks is essential for tailoring ways to prevent type 2 diabetes in midlife and beyond. For women in this life stage, how to combat type 2 diabetes may involve a multi-layered approach that includes both lifestyle changes and hormonal assessments.
10. Can intermittent fasting lead to long-term metabolic benefits beyond blood sugar control?
Absolutely. Intermittent fasting has been linked to improved autophagy, reduced inflammation, and enhanced mitochondrial function—all of which support broader metabolic health. These benefits may protect against not only type 2 diabetes but also cardiovascular disease, neurodegeneration, and certain cancers. Over time, fasting may help reprogram how the body stores and uses energy, contributing to sustained weight loss and insulin sensitivity. For individuals committed to avoiding type 2 diabetes, incorporating fasting into a balanced lifestyle could offer long-term advantages far beyond glucose regulation. It’s one of the most promising frontiers in how to diabetes prevention, particularly when guided by clinical support.
Conclusion: Empowering Yourself with Science-Backed Strategies to Prevent Type 2 Diabetes
In the face of a growing global epidemic, the science is clear: type 2 diabetes is preventable. From microbiome-friendly nutrition and strategic exercise to stress reduction, sleep optimization, and precision medicine, a wealth of evidence now supports a comprehensive, personalized approach to how to combat type 2 diabetes before it starts. As more people begin to ask questions like “is diabetes a preventable disease?” and explore how to prevent diabetes mellitus type 2, it becomes increasingly clear that early action makes all the difference.
Whether you’re seeking practical steps for yourself, guiding a loved one, or influencing public health policy, now is the time to act on the latest science. The path to avoiding type 2 diabetes is no longer shrouded in mystery—it is paved with real, actionable strategies supported by decades of research and modern innovation. Embracing these tools and applying them consistently can help not only delay or prevent type 2 diabetes but also foster a life of greater vitality, clarity, and resilience.
prediabetes reversal strategies, insulin resistance treatment, metabolic syndrome prevention, blood sugar control tips, healthy pancreas function, reversing early diabetes, insulin sensitivity improvement, glucose metabolism support, natural blood sugar remedies, cardiometabolic health tips, anti-inflammatory lifestyle, plant-based nutrition for diabetes, smart carbohydrate choices, circadian rhythm and metabolism, functional fitness for blood sugar, gut health and insulin response, mindful eating habits, lifestyle medicine for diabetes, personalized nutrition plans, digital health tools for diabetes
Further Reading:
Promising new treatment strategy for type 2 diabetes
Healthy lifestyle can prevent diabetes (and even reverse it)
Diabetes Breakthroughs Focus on Making Daily Life Easier
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


