Description
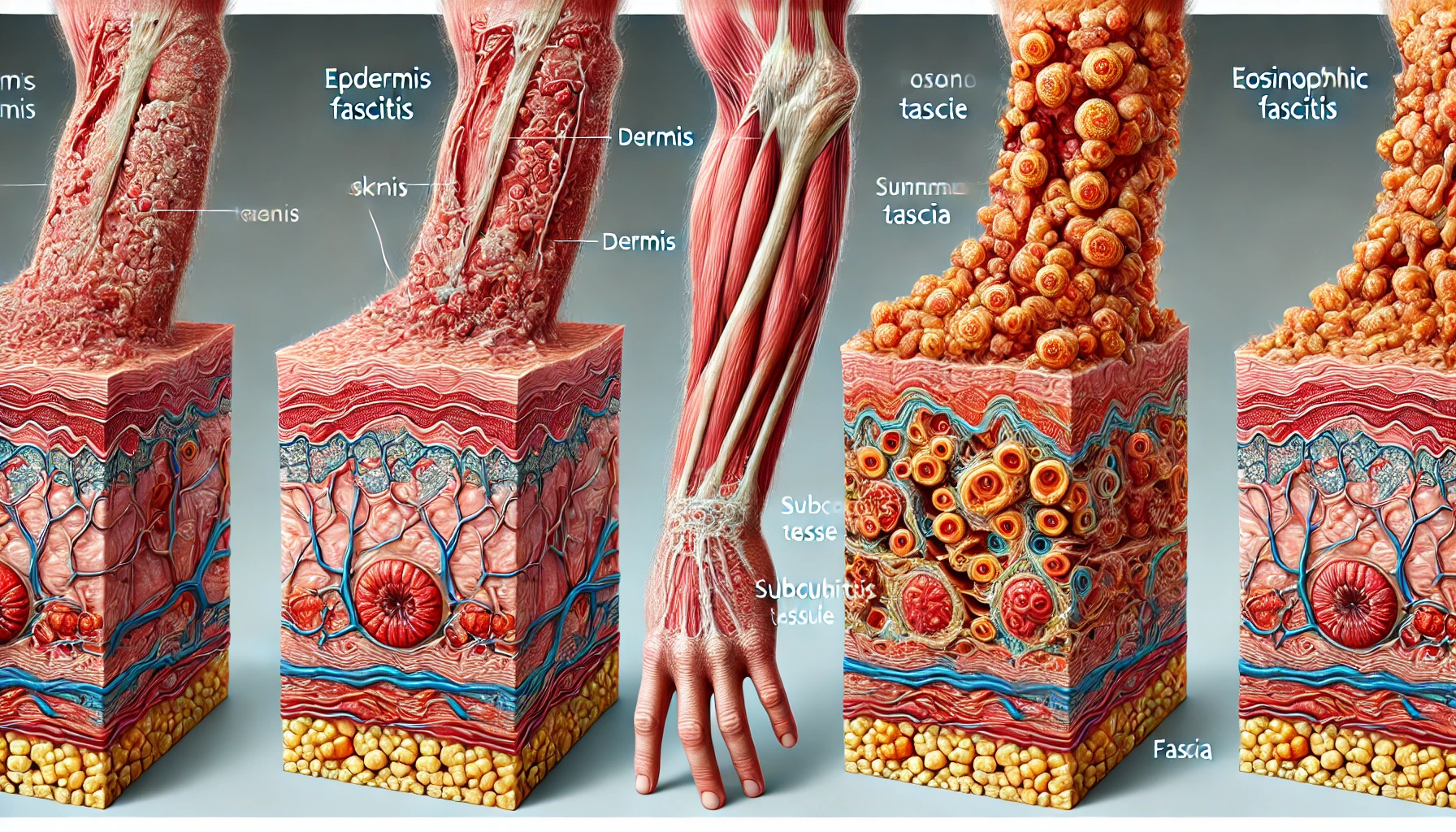
Eosinophilic fasciitis, also referred to as Shulman’s syndrome, is an uncommon connective tissue condition marked by swelling and thickening of the fascia. Fascia is the hard, fibrous tissue that covers muscles, blood vessels, and nerves. It offers structural support and aids in the movement of various tissues. Eosinophilic fasciitis causes a variety of symptoms and consequences as the fascia thickens and swells inside the body. The distinguishing characteristics of eosinophilic fasciitis typically appear gradually and can include:
Skin Changes: The skin over the afflicted area may become constricted, hard, and discolored, frequently having the texture of orange peels.
Localized Swelling: Arms, legs, and even the trunk can all experience inflammation and thickening of the skin along with underlying structures.
Pain and Stiffness: Pain and stiffness are frequently reported by patients in the afflicted areas, which can restrict motion and function.
Muscle Weakness: Patients may have muscle weakness in the afflicted area as the thickening of the fascia affects the underlying muscles.
Systemic Symptoms: Generalized indications like exhaustion and fever may occasionally be observed.
Limited Range of Motion: Common symptoms include restricted joint mobility and difficulties extending or bending the joints.
You May Also Like:
CREST syndrome | Limited cutaneous systemic sclerosis: Description, Causes, and Treatment Protocol
Eosinophilic fasciitis: Description, Causes, and Treatment Protocol is an original (MedNewsPedia) article.
Possible Causes
It is still unclear what causes eosinophilic fasciitis exactly. However, academics and medical professionals have recognized a number of possible causes that might be involved in its emergence. Such aspects include:
Genetic Predisposition: Eosinophilic fasciitis occasionally runs in families, thus there may be a hereditary component to its development. Research is still ongoing to identify specific genetic factors that raise a person’s risk for the illness.
Autoimmune Dysfunction: In autoimmune disorders, the immune system unintentionally targets healthy tissue, such as eosinophilic fasciitis. Genetic traits and environmental triggers might be involved even though the specific cause of this autoimmune reaction is unknown.
Environmental Factors: Eosinophilic fasciitis may develop in susceptible people as a result of exposure to specific environmental variables, such as chemicals or allergens.
Infections: In people who are predisposed, certain diseases, like bacterial or viral infections, can cause eosinophilic fasciitis. Inflammation and the emergence of the illness can result from an immunological reaction to the infection.

Exacerbating and Mitigating Factors
Effective management of eosinophilic fasciitis may depend on an understanding of the elements that cause or prevent the illness. The aggravating and alleviating elements are listed below:
Exacerbating factors may include:
Infections: Eosinophilic fasciitis can be aggravated or brought on by infections. Infections must be avoided and treated right away if they do happen.
Stress: Experiencing anxiety can make autoimmune diseases like eosinophilic fasciitis worse. Stress can be managed by relaxation methods or therapy, which may decrease its effects.
Medications: Certain therapies, like nonsteroidal anti-inflammatory medications (NSAIDs), may render eosinophilic fasciitis worse. To find secure substitutes, patients should speak with their medical professionals.
Environmental Exposures: Reduced exposure to allergens and environmental stimuli may help minimize flare-ups.
Mitigating factors may include:
Physical Therapy: Physical activity can assist in preserving joint mobility and muscular strength, reducing the influence of eosinophilic fasciitis affecting bodily functions. Exercises can be created by physical therapists to fit a person’s demands and restrictions.
Stress Management: Stress-related worsening of the illness can be lessened by using stress-reduction strategies including mindfulness, meditation, deep breathing techniques, or receiving guidance from a counselor or psychologist.
Self-Care: Eosinophilic fasciitis can affect daily living, but it can be lessened by maintaining general health through restful sleep, a nutritious diet, adequate hydration, and frequent exercise to the extent that is possible for the patient.
Continual Monitoring: Regular follow-up appointments with a healthcare professional enable the tracking of the condition’s development and any necessary alterations to treatment schedules. This makes it possible to maintain the treatment’s efficacy and relevance.
Pain Management: Appropriate pain management techniques can greatly reduce discomfort. A healthcare professional may advise using non-opioid painkillers to alleviate pain.
Medication Compliance: For the management of eosinophilic fasciitis, adherence to the recommended medications and treatment schedule is essential. Patients should abide by the dosage and administration instructions given by their doctor.
Environmental Awareness: Taking steps to lessen exposure to environmental triggers or allergies that have been reported as aggravating factors can be helpful.

Standard Treatment Protocol
The main goals of the typical eosinophilic fasciitis treatment plan are to control inflammation and the autoimmune response. It might incorporate the following:
Corticosteroids: Eosinophilic fasciitis is often treated with oral corticosteroids like prednisone. These drugs have strong anti-inflammatory effects and aid in reducing the autoimmune reaction that causes fascia inflammation. Usually, a high first dose is given, then the dose is gradually reduced as soon as symptoms abate. The best dosage for each individual must be determined by routine monitoring.
Immunosuppressant Medications: Healthcare professionals may recommend immunosuppressant drugs like azathioprine, methotrexate, or mycophenolate mofetil when corticosteroids alone are ineffective or poorly tolerated. These medications can help manage the autoimmune response since they function by reducing immune system activity.
Physical Therapy: To effectively treat eosinophilic fasciitis, physical therapy is essential. To keep joints mobile, muscles strong, and functional abilities, therapists create individualized exercise routines. In addition to reducing muscular weakness, this can assist patients in regaining and maintaining their ability to move.
Wound Care: Wound treatment and monitoring are critical for people with major skin changes to avoid complications like ulcers. The use of moisturizers, maintaining clean skin, and shielding the skin from abrasions or injuries are all components of proper wound care.
Pain Management: Since the fascia is inflamed and changing, patients frequently experience pain and discomfort. Non-steroidal anti-inflammatory medications (NSAIDs) or acetaminophen are examples of non-opioid painkillers. Although they can sometimes make the illness worse, using NSAIDs should be evaluated by a healthcare professional.
Observation and Follow-Up: Keeping track of treatment outcomes, determining if drug dosages need to be changed, and addressing any new symptoms or concerns all require periodic visits to a healthcare professional.

Treatment Options
In order to supplement traditional therapies and increase the effectiveness of treatment, patients and healthcare professionals may look into adjunct treatment choices. Prescription drugs, over-the-counter cures, dietary supplements, herbal treatments, and natural remedies are some of the choices available. Following are a few additional therapies:
Prescription Medications: These include the following:
Biologic Therapies
In some circumstances, biologic drugs such as tocilizumab or rituximab are utilized to selectively target immune system components, thereby lowering inflammation.
Immunosuppressant Medications
As previously indicated, when corticosteroids are insufficient, immunosuppressant drugs such as azathioprine, mycophenolate, or mofetil methotrexate, might be administered to moderate the autoimmune reaction.
Topical Steroids
To treat localized skin complaints and inflammation along with oral corticosteroids, doctors might recommend topical steroid ointments or creams.
Over-the-counter Formulations: Acetaminophen and non-steroidal anti-inflammatory medications (NSAIDs), which are non-opioid pain relievers, can help control pain and discomfort. Their application should be reviewed with a healthcare professional, though, as they occasionally may make the situation worse.
Nutritional Supplements: These are as follows:
Vitamin D
According to certain research, taking vitamin D supplements may help control immunological responses. Before beginning any supplements, it is crucial to speak with a healthcare professional to establish the proper amounts and monitoring.
Probiotics
An immune system boost from a balanced gut flora may be possible with the aid of probiotic supplements. Nevertheless, since everyone’s reaction to probiotics may be different, speaking with a doctor is advised.
Omega-3 Fatty Acids
People with eosinophilic fasciitis may benefit from taking omega-3 supplements, which are present in fish oils or flaxseed oils and have anti-inflammatory qualities. With the help of a healthcare professional, the correct dosage should be decided.
Natural Remedies: These are listed below:
Turmeric
The main ingredient in turmeric, curcumin, has anti-inflammatory qualities and may help minimize inflammation brought on by eosinophilic fasciitis. One may think about taking turmeric supplements or including turmeric in their diet.

Aloe Vera
Applying aloe vera gel topically helps relieve skin alterations and lessen itching, relieving symptoms associated with the skin.
Boswellia
Supplements containing boswellia, which are made from the resins produced by the boswellia tree, possess anti-inflammatory qualities and may be useful for treating symptoms. In conversation with a healthcare professional, one can learn more about these supplements.
Arnica
Arnica constitutes a topical cream or gel that is employed in natural medicine to treat pain and discomfort, particularly for localized symptoms.
Herbal Remedies: These involve the following:
Ayurvedic Medicine
To rebalance the body and alleviate inflammation, ayurvedic doctors may advise herbal treatments and dietary modifications. The use of particular Ayurvedic herbs and mixtures may be advised.
Traditional Chinese Medicine (TCM)
Individualized herbal formulations may be suggested by TCM practitioners to deal with the underlying imbalances considered to be responsible for eosinophilic fasciitis.
Nevertheless, it is crucial to stress that, despite the possibility of advantages, these supplemental therapy alternatives should not take the place of the mainstay of the usual treatment regimen, which includes corticosteroids and immunosuppressant drugs. To successfully manage this uncommon ailment and enhance the patient’s general quality of life, a thorough, tailored approach to treatment, overseen by healthcare professionals with knowledge of eosinophilic fasciitis, is necessary.
Conclusion
Eosinophilic fasciitis is a rare yet complex connective tissue disorder that requires a comprehensive and individualized approach to treatment. Early diagnosis and intervention are crucial to managing symptoms and preventing long-term complications. While corticosteroids and immunosuppressants remain the cornerstone of treatment, adjunct therapies such as physical therapy, dietary supplements, and natural remedies can provide additional relief and improve overall well-being. Ongoing monitoring and collaboration with healthcare professionals are essential to tailoring treatments to the patient’s needs and achieving the best outcomes. With a holistic and proactive management plan, individuals with eosinophilic fasciitis can experience significant improvements in quality of life and functionality.
Additional resources for further reference
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5324994
https://www.sciencedirect.com/science/article/pii/S1323893019300218
https://www.tandfonline.com/doi/full/10.1080/1744666X.2022.2078309
https://www.mdpi.com/1422-0067/24/3/1982
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.