Description
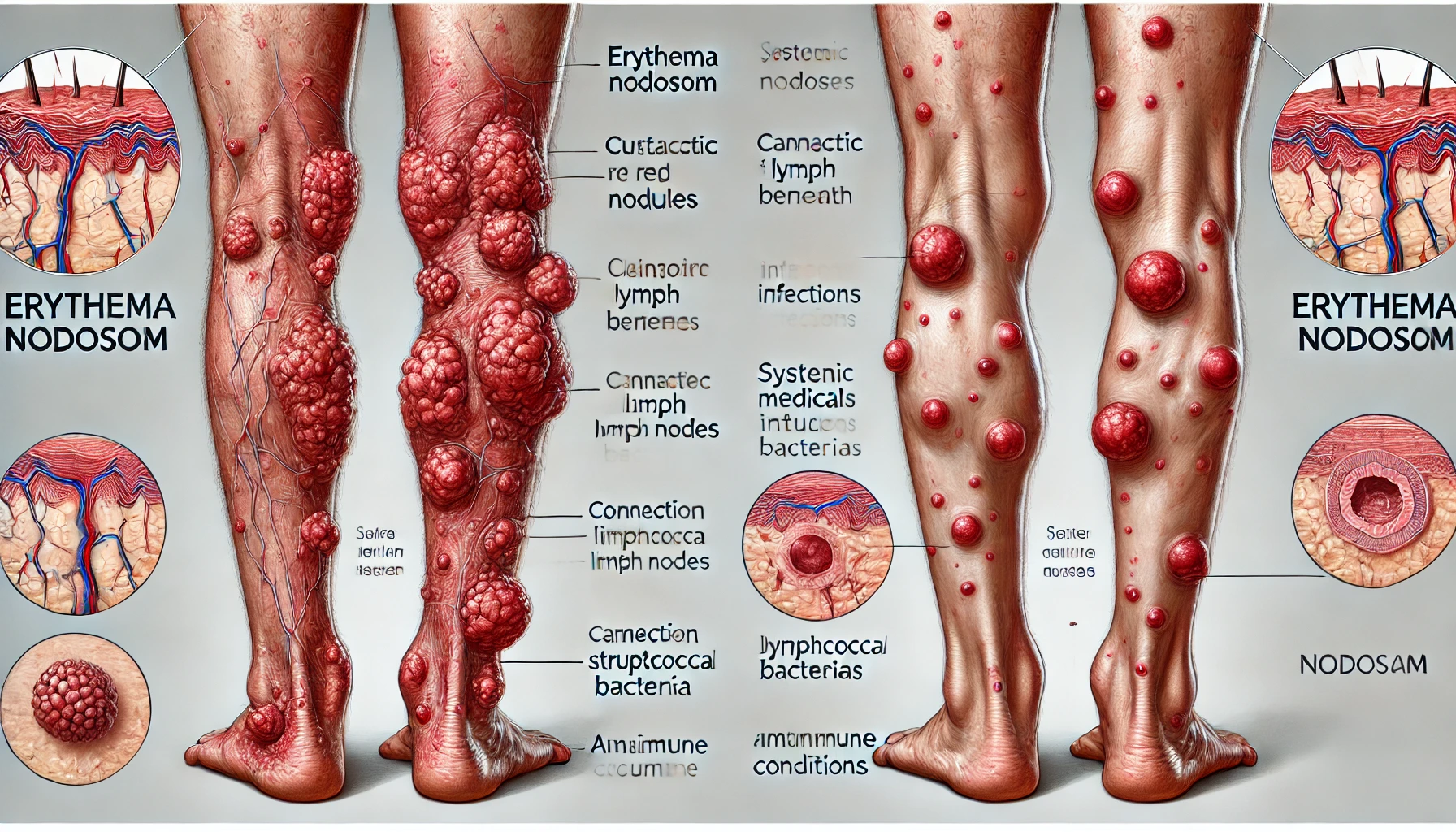
Erythema nodosum (EN) represents a specific form of panniculitis that is defined by the emergence of painful, erythematous, and enlarged subcutaneous nodules, which are most frequently located on the anterior regions of the lower part of the body. Although it is frequently linked to systemic diseases or infections, this disorder might be idiopathic. Erythema nodosum typically affects the shins, though it can also occur on the thighs, arms, or trunk.
It manifests as red, warm, painful, and sensitive nodules or plaques. The diameter of these nodules normally ranges from 1 to 5 cm. They are frequently symmetrical, and as they age, they may take on a bruise-like look. Stretched, glossy, and warm, the skin above may change. With a high occurrence in people between the ages of 20 and 30, EN is largely a medical illness of young adults. Men are less likely to be afflicted than women, and EN often varies seasonally, with more cases being reported during the cooler months.
You May Also Like:
Cold agglutinin disease: Description, Causes, and Treatment Protocol
CREST syndrome | Limited cutaneous systemic sclerosis: Description, Causes, and Treatment Protocol
Erythema nodosum: Description, Causes, and Treatment Protocol is an original (MedNewsPedia) article.
Possible Causes
Erythema nodosum etiology is intricate and frequently complicated. It is typically linked to an underlying disease or trigger, even though the exact reason is not always evident. Several of the possible explanations and connections include:
Inflammatory Diseases: EN is frequently linked to autoimmune and inflammatory disorders such as inflammatory bowel disease (ulcerative colitis and Crohn’s disease), sarcoidosis, and Behçet’s disease.
Infections: The development of EN has been associated with a number of illnesses, like streptococcal pharyngitis, TB, and fungal infections.
Medications: Oral contraceptives, sulfa medicines, and nonsteroidal anti-inflammatory medications (NSAIDs) have all been found to occasionally act as EN triggers.
Malignancies: EN may occasionally be connected to lymphomas or hematological malignancies.
Pregnancy: Although the precise cause is unknown, EN can occasionally happen during pregnancy.

Exacerbating and Mitigating Factors
Numerous aggravating and alleviating factors can affect the intensity and length of EN. These factors comprise the following: –
The exacerbating factors include:
Hot Water Baths: Warm baths or showers may make EN symptoms worse, resulting in more suffering. Vasodilation and inflammation can be encouraged by hot water. The usual recommendation for patients is to bathe in lukewarm water to prevent the problem from getting worse.
Constant Exposure to the Root Cause: Continual exposure to the root problem, like an autoimmune disease or streptococcal infection, can keep EN from getting better when it constitutes a secondary disorder caused by that cause. For EN symptoms to be relieved, the underlying illness must be addressed and treated.
Trauma or Pressure: EN can be made worse by applying too much pressure on the skin or causing direct harm to the affected areas. The discomfort and swelling in the nodules may be exacerbated by even slight pressure, like rubbing or friction. As a result, people with EN are frequently advised to take precautions and refrain from engaging in risky activities like playing aggressive sports or wearing restrictive clothing.

The mitigating factors include:
Cool Compresses: The skin can be soothed, pain can be reduced, and inflammation can be decreased through the application of cold packs or cool compresses to the nodules. Cool compresses are an easy at-home cure that can bring about immediate comfort.
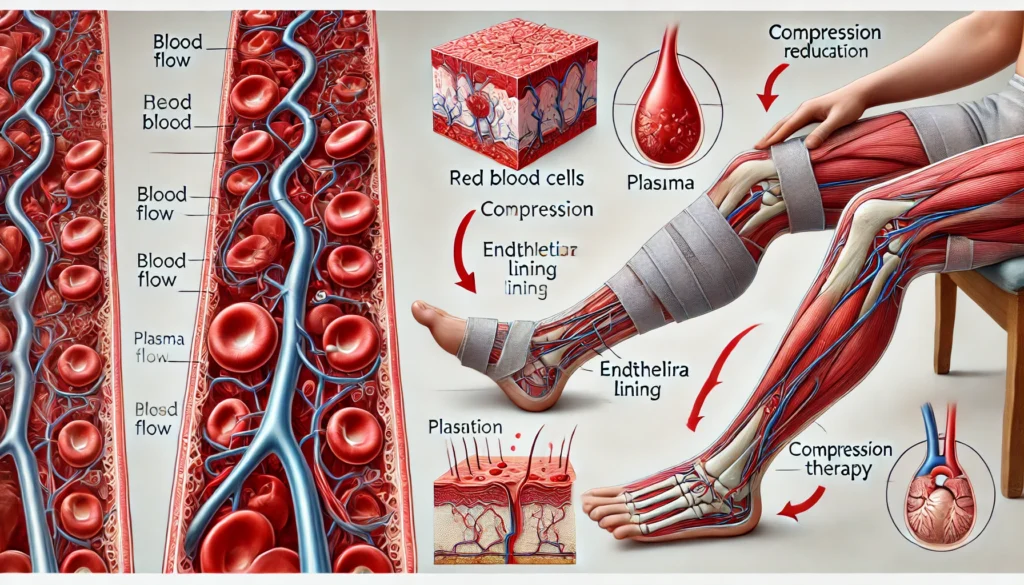
Rest and Elevation: EN can be made less severe by elevating and resting the limbs that are afflicted. Elevation promotes blood flow, lessens edema, and eases discomfort. When feasible, patients are advised to relax while keeping their legs elevated, particularly during episodes of aggravation.
Nonsteroidal Anti-Inflammatory Medications (NSAIDs): EN-related pain and inflammation can be reduced by over-the-counter NSAIDs such as ibuprofen or naproxen. During flare-ups, these drugs relieve the patient’s symptoms and provide comfort.
Compression Stockings: The management of EN may benefit from the use of support clothing or compression stockings. By promoting blood flow and lowering swelling, compression clothing helps ease discomfort caused by the condition.
Corticosteroids (Prescription): Medical professionals may recommend systemic corticosteroids such as prednisone in circumstances of extreme pain and inflammation. Although the use of these drugs should be carefully supervised because of their possible side effects, they can successfully reduce the symptoms.
Avoiding Potential Triggers: It is essential for those suffering from recurrent EN to avoid any triggers or exacerbating circumstances. This entails keeping up with proper cleanliness, being watchful around infectious agents, and according to any advice given by a healthcare professional.
Regular Monitoring: The problem can be lessened with periodic examinations with a healthcare professional who can track EN’s development and modify treatment programs as needed. People who have chronic or persistent EN should pay special attention to this.
Treatment for the Underlying Issue: The best method for minimizing EN is to address and treat its underlying causes. Treating the underlying cause of EN frequently leads to its resolution, whether it be an autoimmune disorder, an infection, or another trigger.
Standard Treatment Protocol
Erythema nodosum (EN) is a disorder that can be treated to relieve symptoms as well as the underlying cause. Depending on the cause of EN, different approaches to treatment may be taken, however, the following elements are typically included in a conventional protocol:
Detecting and Addressing the Root Causes: These include the following:
- Infections: This is associated withstreptococcal infections. Penicillin or amoxicillin are among the medications that are recommended to treat bacterial infections like streptococcal pharyngitis or other bacterial infections when EN is involved. Effective nodule resolution requires completing this step.
- Inflammatory Diseases: These are listed below:
Sarcoidosis: Treatment options for EN linked to sarcoidosis involve corticosteroids or alternative immunosuppressant drugs.
Inflammatory Bowel Disease (IBD): When ulcerative colitis or Crohn’s disease is involved, controlling the underlying IBD becomes the main priority. When necessary, drugs including corticosteroids, 5-aminosalicylates, immunomodulators (for example, azathioprine), or biologics (for instance, infliximab) are utilized.
Behçet’s Disease: If Behçet’s illness is the cause of EN, systemic corticosteroids and colchicine are frequently used in treatment.
Symptomatic Relief: These are as follows:
- Pain and Inflammation: This entails using NSAIDs that are available without a prescription to treat pain and inflammation, such as ibuprofen and naproxen. Particularly during the acute stage of EN, they aid in managing discomfort.
- Local Care: This involves the following:
Rest and Elevation: Encouragement to rest and raise the injured limbs can lessen pain, minimize swelling, and speed up recovery.
Cool Compresses: Inflammation and irritation can be reduced by applying cold packs and cool compresses on the nodules to calm the skin.
- Severe Cases: Systemic corticosteroids are linked to this. Healthcare professionals may recommend systemic corticosteroids including prednisone in instances of EN that are severe, persistent, or especially painful. These reduce inflammation and sometimes provide relief right away. Nevertheless, due to possible negative effects, their usage is strictly regulated, and prolonged use is often avoided.
Observation and Intervention: Patients with EN require routine follow-up visits with a healthcare professional. This helps check for any indications of a condition worsening, complications, or treatment-related side effects while also ensuring that the disease is properly controlled.

Treatment Options
When managing EN, several adjunct therapies and alternate treatment approaches may be taken into consideration in addition to the normal course of treatment. Despite the fact that each person’s effectiveness may differ, they can be helpful in enhancing general well-being:
Nutritional Supplements: These are as follows:
- Vitamin D: The immune system and general health both depend on adequate vitamin D levels. Vitamin D supplementation may be helpful for people having inflammatory bowel disease (IBD), as EN is frequently related to these diseases.
- Omega-3 Fatty Acids: Fish oil capsules and other omega-3 supplements may have anti-inflammatory qualities. They might aid in reducing inflammation and accelerating skin healing.
- Zinc: According to certain research, zinc supplementation may speed up the recovery from skin disorders like EN. Zinc aids in wound healing and immune system strengthening.
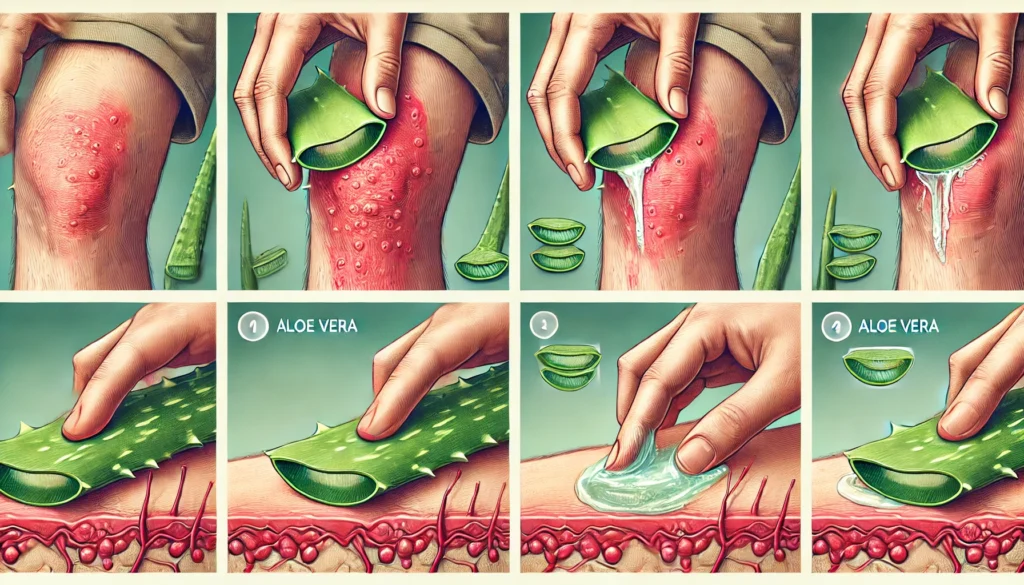
Herbal and Natural Remedies: These include the following:
- Turmeric (Curcumin): Curcumin, a naturally occurring substance with anti-inflammatory effects, is present in turmeric. By adding turmeric to the diet or using curcumin supplements, EN-related inflammation may be decreased.
- Calendula: The marigold plant, from which calendula cream or ointment is made, has calming properties that may benefit the skin. Calendula can ease discomfort and alleviate skin irritation when applied topically to affected regions.
- Aloe Vera: The calming and anti-inflammatory qualities of aloe vera gel are well known. To relieve pain and minimize skin redness, it may be topically applied to the regions that are affected.
- Echinacea: The immune system is thought to be supported by echinacea, which may also aid the body in combating infections linked to EN. Although there is not much proof of its efficacy, echinacea capsules and tea may be considered.
However, to develop a thorough and individualized treatment plan, patients with EN should make open contact with their healthcare professionals a priority. While resolving the root cause of the condition is essential to effective care, these supplemental therapies can help patients with erythema nodosum reduce their symptom burden and enhance their overall standard of life.
Conclusion
Erythema nodosum (EN) is a multifaceted condition often linked to underlying systemic diseases, infections, or triggers. While it primarily manifests as painful nodules on the lower limbs, its successful management depends on identifying and addressing its root cause, whether it be infections, inflammatory conditions, or medication-related triggers. Symptomatic relief through NSAIDs, rest, elevation, and topical remedies, combined with targeted treatments for the underlying condition, can significantly alleviate discomfort and promote recovery. Adjunct therapies such as nutritional supplements and natural remedies may offer additional support. However, individualized care and regular monitoring by healthcare professionals remain essential for achieving the best outcomes. With a holistic approach to treatment, individuals with EN can experience improved quality of life and effective symptom management.
Additional resources for further reference
https://www.ncbi.nlm.nih.gov/books/NBK470369
https://www.mdpi.com/2227-9067/9/4/511
https://link.springer.com/article/10.1007/s40257-021-00592-w
https://www.healthdirect.gov.au/erythema-nodosum
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.