Description
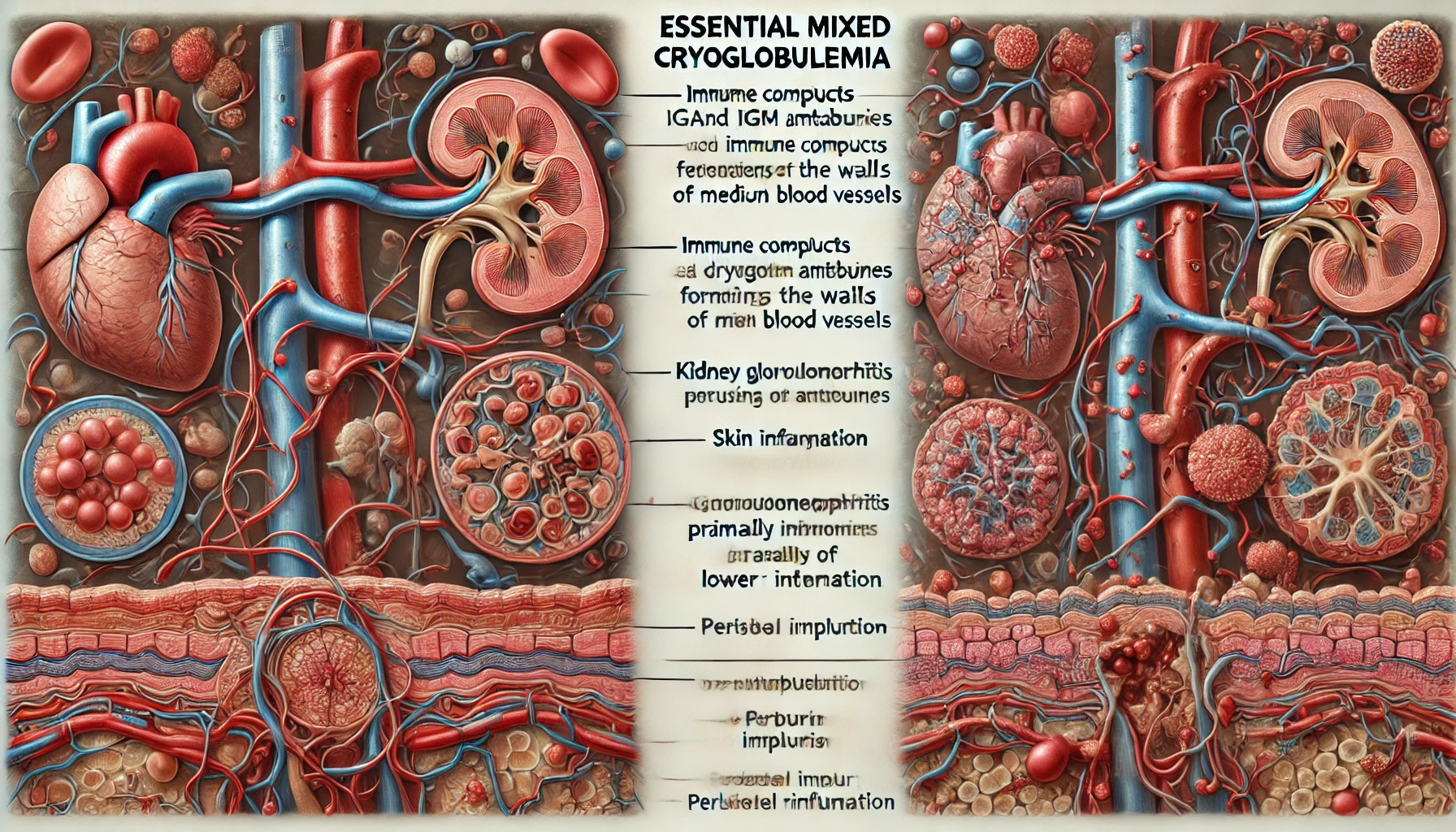
Essential mixed cryoglobulinemia (EMC) refers to a systemic form of vasculitis that mostly impacts tiny and small to medium-sized arteries and veins. Cryoglobulins, aberrant immunoglobulin complexes that are able to precipitate at low temperatures, are present in the blood and serve as a defining characteristic of the condition. EMC frequently manifests with a wide range of clinical symptoms, rendering diagnosis and treatment difficult. Cryoglobulins, usually IgM or mixed IgG or IgM antibodies, develop and lodge in tiny and moderate-sized blood vessels as a result of the systemic autoimmune disease known as EMC.
A class of proteins known as cryoglobulins precipitate at low temperatures and dissolve at high ones, frequently causing vasculitis. The clinical presentation might differ greatly amongst patients with this disorder, which mainly impacts the joints, skin, and numerous organs. Purpura (or skin rashes), neuropathy, arthralgia (or joint pain), and renal dysfunction are among the common symptoms of EMC. Organ damage and other potentially fatal complications can result in severe cases.
You May Also Like:
Cold agglutinin disease: Description, Causes, and Treatment Protocol
Henoch-Schönlein purpura / IgA vasculitis: Description, Causes, and Treatment Protocol
Essential mixed cryoglobulinemia: Description, Causes, and Treatment Protocol is an original (MedNewsPedia) article.
Possible Causes
Although the precise etiology of EMC is still unknown, many factors are thought to have played a role in its emergence. These factors consist of the following:
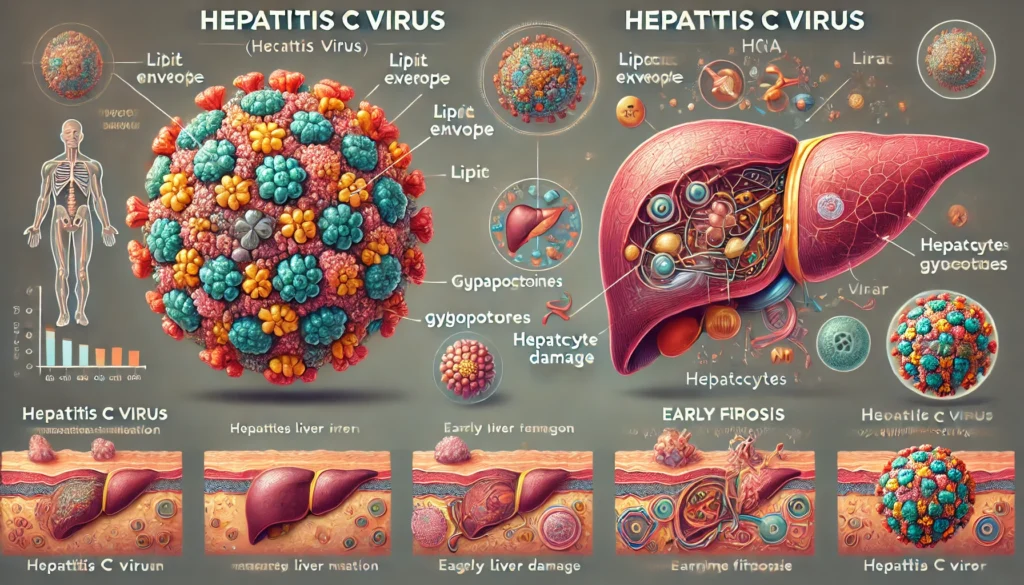
Infectious Agents: As many as 90% of individuals with EMC have previous experiences of acute hepatitis C virus (HCV) infections. Cryoglobulins may develop as a result of an autoimmune reaction brought on by the virus.
Immunological Aberrations: It is believed that the pathophysiology of EMC is significantly influenced by immune system dysregulation. When T-cells are dysfunctional, immunological complexes can develop and accumulate in blood vessels, and B lymphocytes can create aberrant cryoglobulins.
Genetic Predisposition: Given that EMC appears to be passed down in families, genetic factors may make a person more susceptible to the condition. Undoubtedly connected genetic risk factors for EMC are still unknown.
Environmental Factors: The symptoms of the illness may worsen when exposed to specific environmental variables, like cold temperatures, which may cause cryoglobulins to precipitate.

Exacerbating and Mitigating Factors
When aberrant immunological proteins known as cryoglobulins are present in the blood, a rare autoimmune illness known as essential mixed cryoglobulinemia (EMC) develops, which can cause a variety of symptoms and consequences. Exacerbating and moderating factors that can affect EMC severity include the following:
The exacerbating factors include:
Hepatitis C Virus (HCV) Infections: Nearly 90% of EMC patients have previous episodes of HCV infection, indicating a close correlation between the two conditions. When HCV causes an autoimmune reaction, cryoglobulins are produced, which exacerbates the autoimmune condition.
Cold Exposure: Exposure to chilly temperatures significantly worsens EMC. In response to cold, cryoglobulins can precipitate, activating the immune system and creating immunological complexes. Specifically, skin rashes, joint discomfort, and systemic inflammation may be made worse by this.
Infections: Other infections, besides HCV, can make EMC worse. Infections can amplify the production of cryoglobulins and lead to more serious consequences by stimulating the immune system. Infections must be controlled and treated quickly.
Medication Interactions: Some drugs may interact poorly with EMC, particularly those that weaken the body’s immune system or affect liver function. These interactions may make the problem worse and cause consequences.
Stress: Stress on the physical and emotional levels might exacerbate EMC symptoms. Stress can boost immunological function, which raises inflammatory mediators and exacerbates autoimmune symptoms. Techniques for reducing stress are crucial for controlling EMC successfully.

The mitigating factors include:
HCV Eradication: Eliminating the HCV virus is the main and most efficient strategy to lessen the symptoms of the condition in those with HCV-associated EMC. The symptoms of EMC may disappear with effective HCV treatment.
Avoidance of Cold: People are urged to wear warm clothing and stay out of the cold because EMC is sensitive to cold. The key to controlling the illness and lowering symptom aggravation is preventing the formation of cryoglobulins.
Infection Management: It is critical in EMC to treat infections promptly and effectively. Taking care of infections as soon as they arise lessens immune system activity and the condition’s aggravating effects.
Immunosuppressive Therapy: In EMC, immunosuppressive drugs like rituximab and corticosteroids can help to lessen inflammation and the autoimmune response. Both symptom relief and immune system regulation are the goals of these drugs.
Dietary Modifications: For some EMC sufferers, dietary adjustments may be advantageous. A low-protein or low-salt diet may assist those with renal involvement in controlling their proteinuria (increased protein levels in the urine) and blood pressure, reducing the symptoms associated with their kidneys.
Stress Reduction: Stress can affect the immune system and general well-being, but it can also be managed through mindfulness, relaxation methods, and stress management approaches, potentially reducing symptom flare-ups.
Standard Treatment Protocol
Depending on the symptoms and root causes of each patient, particularly if the illness is linked to hepatitis C virus (HCV) infections, the treatment of EMC often entails a variety of methods. The main objectives are to control symptoms, reduce inflammation, and, if necessary, address the underlying cause:
HCV Eradication: The initial and most significant phase in treating those suffering from HCV-associated EMC is to use direct-acting antiviral medications, like sofosbuvir and ledipasvir, to address the underlying viral infections. EMC symptoms may go away after effective HCV elimination.
Immunosuppressive Therapy: These are as follows:
Corticosteroids
In order to reduce inflammation and its symptoms, including skin rashes, joint pain, and peripheral neuropathy, corticosteroids (like prednisone) are frequently administered.
Rituximab
When corticosteroids are ineffective or there are severe circumstances, the monoclonal antibody rituximab, which targets B cells, can be explored.
Plasma Exchange: Plasmapheresis, or therapeutic plasma exchange, can be utilized to eliminate cryoglobulins from the bloodstream and treat symptoms in severe, quickly advancing EMC cases with considerable organ involvement.
Pain Management: They consist of the following:
NSAIDs
Non-steroidal anti-inflammatory medicines (NSAIDs), like ibuprofen, can be used to treat inflammation and manage joint discomfort.
Opioids
Opioids may be recommended for chronic pain, but due to possible adverse effects, their usage should be properly monitored.
Symptomatic Treatment: These are listed below:
Antihistamines
Antihistamines can be used to treat particular symptoms, including itching.
ACEs or ARBs
Angiotensin receptor blockers (ARBs) or angiotensin-converting enzyme (ACE) inhibitors can be recommended for EMC patients who suffer from kidney dysfunction to treat hypertension and improve proteinuria.
Treatment Options
To supplement traditional treatment and enhance the overall health of EMC patients, a variety of supplemental therapies and alternative methods can be taken into consideration:
Prescription Medications: The following is a list of them:
Interferon-alpha
Interferon-alpha, frequently in conjunction with ribavirin, may be administered to stop viral replication and lessen cryoglobulin formation in certain HCV-associated EMC patients. Given the potential negative effects, this medication should be closely monitored.
Cyclophosphamide
Cyclophosphamide can be administered as an immunosuppressive drug in severe instances of EMC with extensive organ involvement. Due to possible negative effects, it is usually only taken briefly.
Over-the-Counter Formulations: These are as follows:
Topical Steroids
Creams containing hydrocortisone that are sold over the counter might help relieve itching and skin rashes.
Non-steroidal anti-inflammatory Medications (NSAIDs)
NSAIDs sold over the counter can reduce joint discomfort and swelling. If using a medication for a prolonged period of time, patients should adhere to the authorized dosages and seek medical advice.
Nutritional Supplements: These include the following:
B Vitamins and Folate
The effects of some drugs may be lessened and overall health may be supported by these supplements.
Vitamin D
Optimal vitamin D intake promotes bone health and the immune system, which may be of special importance for people taking immunosuppressive medicines.
Omega-3 Fatty Acids
Fish oil and other omega-3 supplements can reduce inflammation, which may be advantageous for EMC patients.
Natural Remedies: Here are some of them:
Turmeric
Turmeric’s main ingredient, curcumin, has anti-inflammatory qualities and may help decrease inflammation in EMC. However, if consuming blood-thinning drugs, curcumin supplements ought to be used with caution.

Ginger
Ginger possesses anti-inflammatory and antioxidant qualities that may help to reduce joint pain. Supplementing with ginger or including ginger in food can be beneficial.
Herbal Remedies: Among them are the following:
Echinacea
EMC patients may benefit from echinacea’s immune system support and its ability to lessen the severity and frequency of infections.
Milk Thistle
Commonly used to improve liver health, milk thistle can be helpful in EMC linked to HCV.
Physical Treatment and Exercise: These encompass the following:
Low-Impact Exercise
Tai chi, swimming, and other gentle exercises can enhance well-being by maintaining joint flexibility and general health.
Physical Therapy
Patients with EMC who receive physical therapy can better manage their joint discomfort, increase their mobility, and keep their muscles strong. An exercise regimen can be created by a physical therapist.
However, individual reactions to treatments and possible interactions with other medicines or diseases can vary. Therefore, it is important for people with EMC to examine these additional treatment choices with their healthcare professionals. To offer complete therapy for individuals with EMC, a multidisciplinary approach comprising hepatologists (in the states of HCV-associated EMC), rheumatologists, and other experts is frequently required.
Conclusion
Essential mixed cryoglobulinemia (EMC) is a complex autoimmune condition that requires a comprehensive and multidisciplinary approach for effective management. While its causes remain diverse and multifactorial, addressing underlying factors such as hepatitis C virus (HCV) infections, minimizing cold exposure, and managing infections are crucial in mitigating symptoms and disease progression. Standard treatments, including immunosuppressive therapy, plasma exchange, and pain management, alongside supportive measures such as dietary modifications and stress management, can significantly improve quality of life for individuals with EMC. Complementary therapies, though not a substitute for medical treatment, may offer additional relief and symptom management. Given the condition’s variability in presentation and response to treatment, ongoing consultation with healthcare professionals is essential to tailor an individualized care plan. With advances in understanding and treatment options, there is hope for improved outcomes and symptom relief for those living with EMC.

Additional resources for further reference
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2569912
https://www.sciencedirect.com/topics/medicine-and-dentistry/cryoglobulinemia
https://www.ncbi.nlm.nih.gov/books/NBK557606
https://www.researchgate.net/publication/23262156_Mixed_cryoglobulinemia
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.