Description
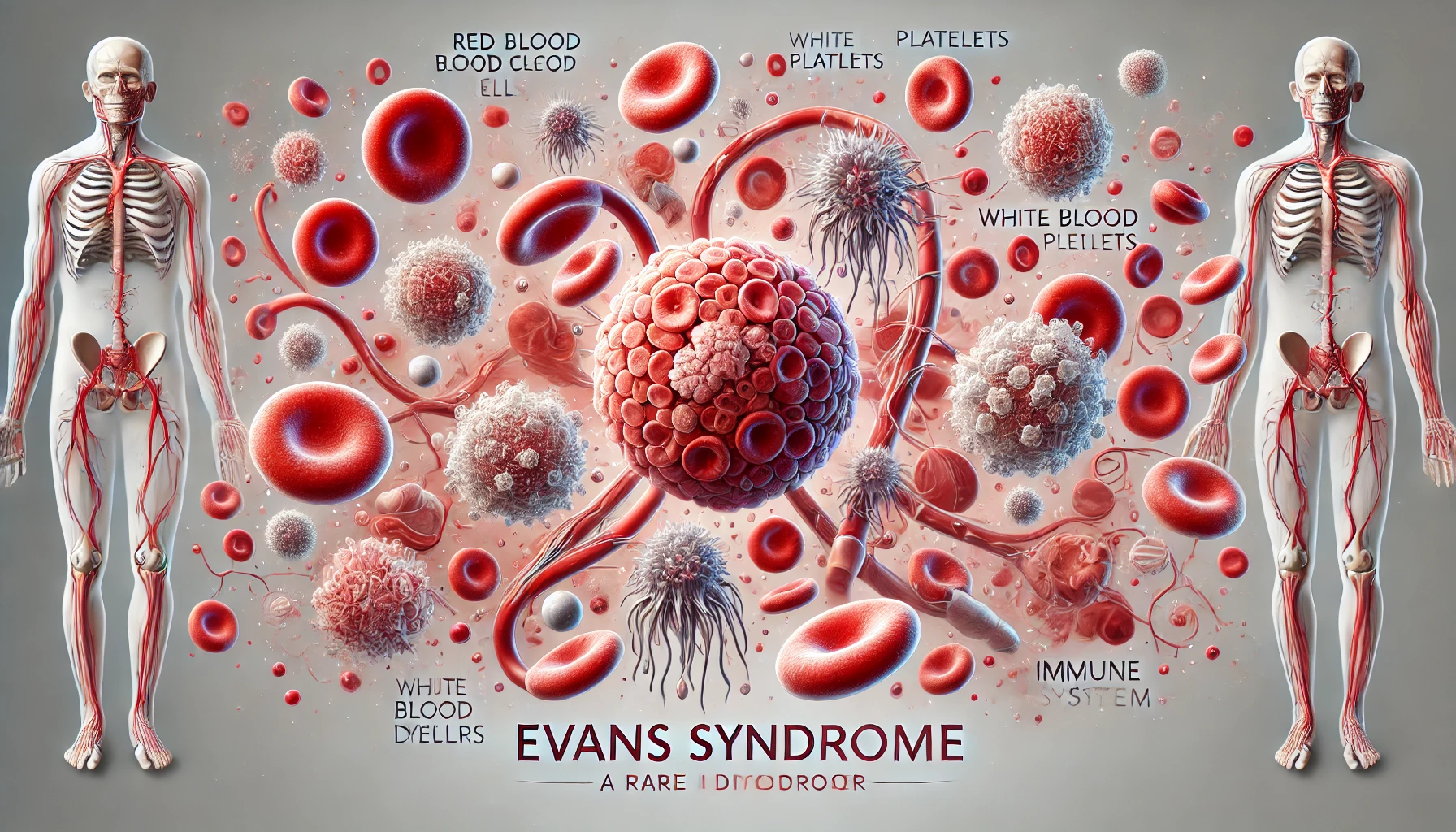
Evans syndrome, an uncommon autoimmune disease, is defined by the confluence of immune thrombocytopenia (ITP) and autoimmune hemolytic anemia (AIHA). Because the immune system is also destroying platelets and red blood cells at the same time, this illness offers a complicated therapeutic scenario. Evans syndrome is thought to be caused by an immune system imbalance, but the exact cause is unknown. Symptoms of Evans syndrome usually include red blood cell and platelet breakdown (AIHA and ITP, respectively). Patients may have jaundice, a pale complexion, purpura, petechiae, and easy bruising, in addition to exhaustion. Depending on the degree of thrombocytopenia and anemia, the symptoms might range in severity from moderate to severe.
Evans syndrome is diagnosed by clinical assessment and laboratory testing, thus ruling out other illnesses that have similar symptoms. Important tests for diagnosis consist of:
- Using blood smears, anomalies in blood cells can be observed
- Red blood cell, hemoglobin, and platelet counts can be determined by a complete blood count, or CBC
- Aspiration of the bone marrow to measure platelet production and determine the reason for thrombocytopenia
- Using the Direct Coombs test for checking antibodies on red blood cell surfaces
An aberrant immune response is part of the underlying pathogenesis of Evans syndrome. In the bloodstream and reticuloendothelial system, autoantibodies, particularly IgG and IgM, target platelets and red blood cells, causing them to be destroyed. Viral infections, other environmental variables, and genetic predispositions may contribute to an autoimmune reaction, but the exact cause is unknown.
You May Also Like:
Cold agglutinin disease: Description, Causes, and Treatment Protocol
Henoch-Schönlein purpura / IgA vasculitis: Description, Causes, and Treatment Protocol
Evans syndrome: Description, Causes, and Treatment Protocol is an original (MedNewsPedia) article.
Possible Causes
Although the specific reasons for Evans syndrome cannot be entirely understood, the following elements have been suggested as possible contributors to the condition’s development:
Viral Infections: Evans syndrome has been associated with viral diseases, including hepatitis, cytomegalovirus (CMV), and Epstein-Barr virus (EBV). Autoantibody generation is believed to be a possible outcome of these disorders causing an abnormal immunological response.
Genetic Factors: Even while Evans syndrome’s genetic cause is still unknown, some research points to a hereditary propensity. Evans syndrome risk may be raised by an autoimmune disease-related family history.
Environmental Factors: The emergence of autoimmune illnesses may be influenced by environmental variables, like exposure to specific chemicals or toxins. Evans syndrome’s precise causes are yet unknown, though.
Autoimmunity: Evans syndrome is considered an autoimmune illness, implying that self-cells are incorrectly recognized as foreign by the immune system. A defining feature of this illness is the generation of autoantibodies that target platelets and red blood cells.

Exacerbating and Mitigating Factors
The degree of Evans syndrome and the efficacy of treatment are largely dependent on aggravating and mitigating circumstances. These elements may have an impact on how Evans Syndrome patients experience the condition and their general quality of life. These are a few of them:
The aggravating factors consist of:
Infections: Evans syndrome may be brought on by infections, particularly viral infections. Autoantibodies can result from viral diseases like hepatitis, cytomegalovirus (CMV), and Epstein-Barr virus (EBV) that cause an aberrant immune response. The autoimmune assault on platelets and red blood cells can be made worse by infections.
Stress: Anxiety can aggravate autoimmune diseases such as Evans syndrome, regardless of its duration. Cortisol is one of the stress hormones released when under stress, and it can affect immunity. Excessive stress can exacerbate the autoimmune invasion of platelets and red blood cells and trigger heightened inflammatory reactions.
Enhance antioxidant protection and support blood health with Turmeric—Balance Naturally, Shop Now!

Medications: Certain drugs may make immune-related conditions like Evans syndrome worse. Antibiotics and other medications can disrupt the immune system, which may cause or exacerbate autoimmune reactions. To prevent drug-induced exacerbations, people with Evans syndrome must disclose to their healthcare practitioners all medications they take.
The mitigating factors consist of:
Infection Prevention: Evans syndrome management primarily entails preventing infections, especially viral infections. To reduce the chance of infection-triggered exacerbations, people with the illness should maintain proper cleanliness, follow advised immunization regimens, and stay away from sick people in close quarters.
Stress Management: For those who have Evans syndrome, stress management is crucial. Practices that can lower stress levels and minimize the chance of exacerbations include deep breathing exercises, yoga, mindfulness, and meditation.
Lifestyle Modifications: Positive lifestyle modifications can lessen Evans syndrome’s symptoms and severity. These adjustments might consist of:
Balanced diet
A diet high in minerals and vitamins can boost general health and strengthen the immune system.
Regular exercise
In addition to boosting immunity, physical activity can enhance general well-being.
Support Systems: The emotional and physical difficulties of living with Evans syndrome can be easier for people to handle if they have a strong support network that consists of family, friends, and support groups. Stress reduction and enhanced health can be attributed to receiving emotional support.
Medication Management: Immunosuppressants and other medications administered for Evans syndrome must be properly managed. One way to keep diseases under control and reduce exacerbations is by adherence to medication schedules and routine follow-up visits with healthcare professionals.

Standard Treatment Protocol
The goals of the conventional Evans syndrome treatment plan are to suppress the immune system, control the autoimmune response, and address the loss of platelets and red blood cells. Depending on the extent and reaction of each patient, the particular treatment plan may change, although the following therapies are frequently used:
Intravenous Immunoglobulin (IVIG): Immunoglobulins from healthy donors are infused intravenously as part of IVIG therapy. IVIG can enhance red blood cell and platelet counts, reduce autoantibodies, and regulate immunological response. When corticosteroids by themselves are inadequate or poorly tolerated, it is usually utilized.
Corticosteroids: Evans syndrome is frequently treated initially with corticosteroids, which include prednisone. Their mechanisms of action include lowering inflammation, stopping the thinning of platelets and red blood cells, and decreasing the immune system’s aberrant reaction.
Immunosuppressive Agents: Immunosuppressive drugs may be used in situations where IVIG and corticosteroids are insufficient. Cyclosporine, mycophenolate mofetil, and azathioprine are popular options. These medications function by lowering the synthesis of autoantibodies and inhibiting the immune system.
Rituximab: When other treatments are ineffective, rituximab, a type of monoclonal antibody, is utilized. It selectively targets and destroys B-cells, which are necessary for the synthesis of autoantibodies. The autoimmune reaction is suppressed by getting rid of these cells.
Splenectomy: A splenectomy, or an operation to remove the spleen, may be considered in situations involving refractory disease when previous treatments have failed to provide relief. Interaction between immune cells and the potential for platelet destruction occurs in the spleen.
Thrombopoietin Receptor Agonists: Eltrombopag and romiplostim are examples of thrombopoietin receptor agonists that increase platelet production. When it comes to treating Evans syndrome’s immune thrombocytopenia (ITP) component, they are especially successful.
Treatment Options
Along with the customary treatment plan, adjunct therapies such as dietary supplements, home cures, and lifestyle adjustments may be taken into consideration to enhance conventional treatment and promote general health. To make sure adjunct therapies are safe and suitable for a given patient, it is crucial to confer with medical professionals before implementing any. The following are a few choices for adjunctive therapy:
Nutritional Supplements: These are listed below:
Iron and Folate
To treat anemia brought on by the degeneration of red blood cells, supplements containing folate and iron could be required. For the body to produce hemoglobin, adequate iron consumption is required.
Vitamin B12
The production of blood cells can be supported and anemia may be reduced with the use of vitamin B12 supplements.
Natural Remedies: These consist of the following:
Turmeric
An anti-inflammatory substance called curcumin is found in turmeric. By taking pills or including turmeric in their diet, some people experience relief from the symptoms of autoimmune diseases.

Echinacea
Exacerbation of disease may be avoided as echinacea is thought to improve immune function and decrease the frequency and intensity of infections.
Astragalus
Traditional Chinese medicine frequently uses the herb astragalus to strengthen the immune system. In autoimmune disorders, it might aid in controlling immunological responses.
Dietary Modifications: A few dietary adjustments may assist with immune system support and inflammation management. It may be advantageous to consume fewer processed meals and more antioxidant-rich fruits and vegetables.
Regular Exercise: Regular physical activity helps enhance general well-being and maintain a strong immune system. For individualized exercise advice, people should speak with a healthcare provider.
Stress Management: By boosting inflammatory reactions, long-term stress can make autoimmune diseases worse. Practices that reduce stress, like yoga, meditation, and deep breathing, may decrease symptoms.
Infection Prevention: The management of Evans syndrome depends heavily on preventing infections, especially viral infections. Exacerbation of an illness can be prevented by maintaining proper cleanliness, receiving the required vaccines, and limiting contact with sick people.
However, when creating a complete treatment plan that is tailored to their requirements, people with Evans syndrome must collaborate closely with their medical team. Speaking with medical professionals about adjunct therapies can help to ensure that they do not worsen a patient’s condition or conflict with recommended treatments. To determine the efficacy of treatment and make any required modifications, routine follow-up visits and careful symptom monitoring are also crucial.
Conclusion
Evans syndrome presents a complex challenge due to its dual autoimmune impact on platelets and red blood cells, leading to symptoms ranging from mild to severe. Effective management requires a multifaceted approach combining standard treatments such as corticosteroids, IVIG, and immunosuppressive agents with lifestyle modifications, stress management, and infection prevention. Emerging adjunct therapies, including dietary supplements and natural remedies, can provide additional support when integrated thoughtfully into a personalized treatment plan. Collaborative care between patients and healthcare providers is essential to monitor symptoms, optimize therapies, and improve quality of life for those living with this rare autoimmune condition.
Additional resources for further reference
https://pubmed.ncbi.nlm.nih.gov/30085557
https://www.mdpi.com/2077-0383/9/12/3851
https://www.frontiersin.org/articles/10.3389/fped.2019.00304/full
https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-022-07512-1
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.