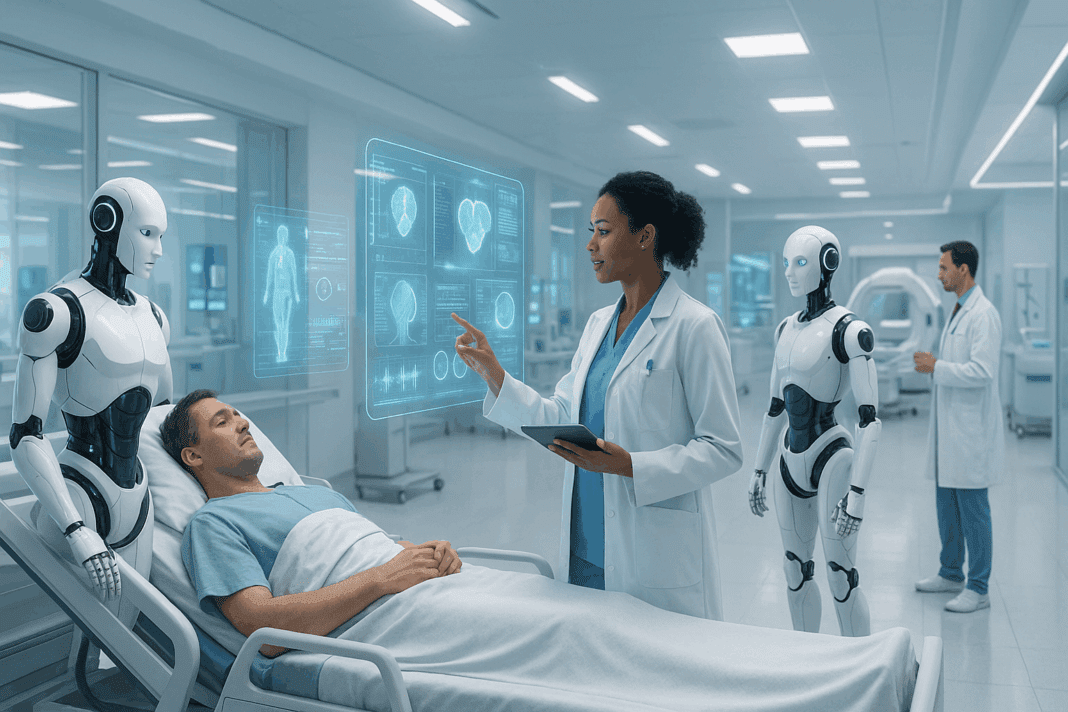
The future of artificial intelligence in healthcare holds unparalleled promise, poised to transform medical practices, patient outcomes, and the very fabric of healthcare delivery. As we stand on the threshold of a digital revolution, AI’s influence is becoming increasingly evident across clinical decision-making, diagnostics, personalized treatment, and operational efficiency. This article delves deep into breakthrough insights and expert predictions about how the evolving landscape of artificial intelligence will redefine healthcare for generations to come.
You may also like: Revolutionizing Healthcare: How AI in Medicine Is Enhancing Diagnosis, Treatment, and Patient Outcomes
Understanding the Future of Artificial Intelligence in Healthcare: Foundations and Evolution
Artificial intelligence has been a topic of intrigue and exploration for decades, but only in recent years has its true potential in healthcare begun to materialize. Initially, AI’s foray into healthcare involved basic automation tasks, such as scheduling and data management. However, today’s advancements extend far beyond administrative duties. Machine learning algorithms now assist physicians in diagnosing complex diseases, predicting patient deterioration, and even recommending treatment pathways tailored to an individual’s unique genetic profile. The integration of big data, electronic health records, and AI has catalyzed a shift towards predictive and precision medicine, laying the groundwork for transformative change.
The future of artificial intelligence in healthcare is inextricably linked to the evolution of these technologies. As computational power grows and data sources expand, AI systems are becoming smarter, faster, and more adept at interpreting nuanced medical information. This progression is not merely technological but deeply philosophical, prompting the medical community to reconsider traditional models of care in favor of more adaptive, responsive, and data-driven approaches.
Breakthrough Applications of AI in Diagnostics and Early Detection
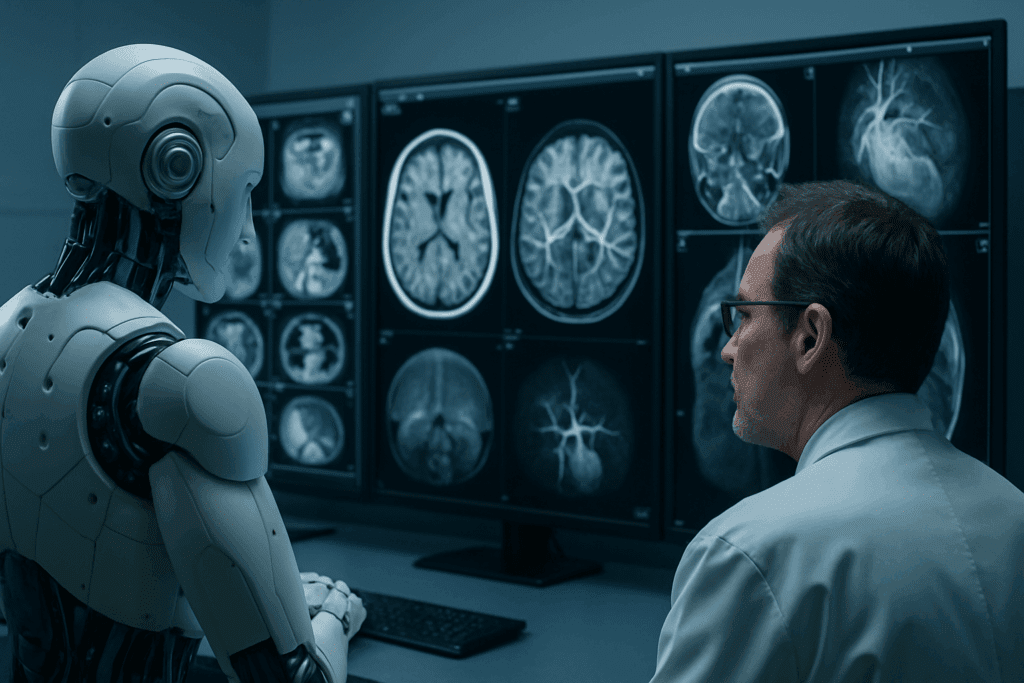
One of the most remarkable breakthroughs driven by AI is its application in medical diagnostics and early disease detection. In radiology, AI-powered imaging analysis tools can detect abnormalities in X-rays, CT scans, and MRIs with a level of accuracy that rivals or even surpasses human experts. Such capabilities are critical for identifying conditions like cancer, cardiovascular disease, and neurological disorders at their earliest, most treatable stages.
Pathology, too, has witnessed revolutionary changes with AI-enhanced analysis of tissue samples. Algorithms can now identify cancerous cells with extraordinary precision, reducing diagnostic errors and expediting the initiation of appropriate treatments. Moreover, wearable devices equipped with AI sensors are increasingly capable of detecting early signs of chronic diseases such as diabetes or atrial fibrillation, often before a patient experiences any noticeable symptoms.
The future of AI in medicine will likely see further refinements in diagnostic tools, integrating multimodal data streams—from imaging to genomics to patient-reported outcomes—to create comprehensive health profiles. Such integration will enable physicians to move from reactive to proactive care, fundamentally shifting the paradigm towards prevention rather than cure.
Personalized Medicine: The Role of AI in Tailoring Treatments
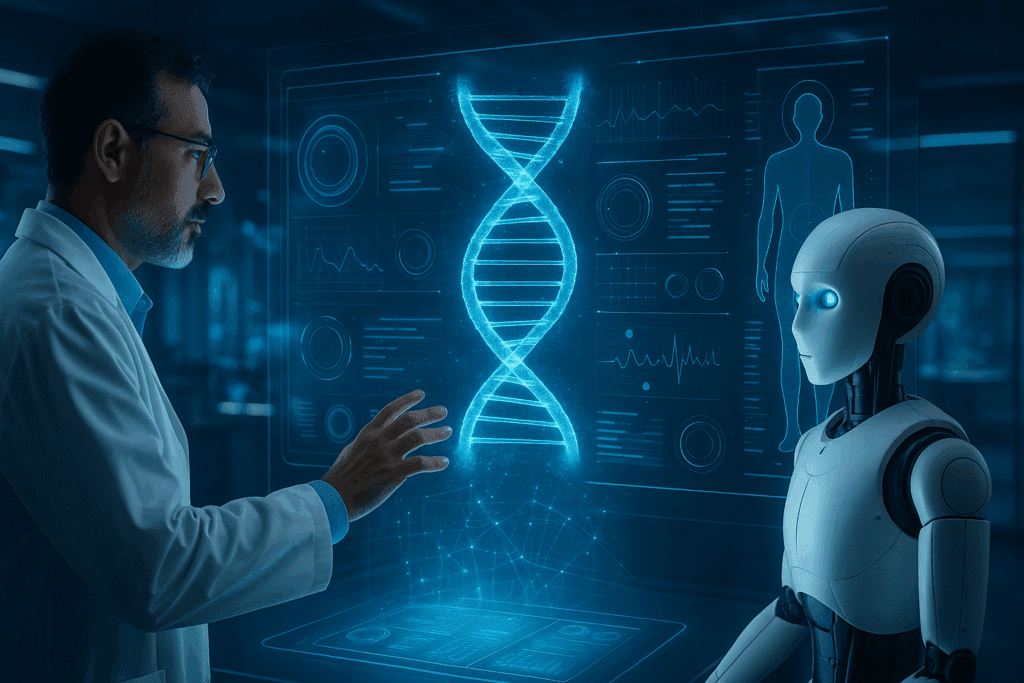
Another profound area where the future of artificial intelligence in healthcare shines is in the realm of personalized medicine. Traditional treatment protocols often adopt a one-size-fits-all approach, but AI is changing that narrative by enabling the development of customized therapeutic regimens based on an individual’s genetic makeup, lifestyle, and environmental factors.
Through machine learning models trained on vast datasets encompassing genomics, proteomics, and metabolomics, AI can identify biomarkers that predict how a patient will respond to a particular drug or therapy. For instance, AI-driven platforms can help oncologists select the most effective chemotherapy agents for a cancer patient based on the molecular characteristics of their tumor. This not only improves outcomes but also minimizes unnecessary side effects.
The future of AI in medicine envisions a world where treatments are dynamically adjusted in real-time based on continuous monitoring of a patient’s response. Wearable devices, smart implants, and remote patient monitoring tools will feed data back to AI systems, allowing for rapid course corrections and ensuring optimal therapeutic efficacy.

Revolutionizing Healthcare Operations with Artificial Intelligence
Beyond the clinical realm, AI is set to revolutionize healthcare operations, making them more efficient, cost-effective, and patient-centric. Administrative tasks, often a significant burden on healthcare providers, can be streamlined through AI-driven automation. Natural language processing (NLP) technologies can transcribe and summarize physician-patient interactions, reducing the time clinicians spend on documentation and allowing them to focus more on patient care.
In hospital settings, predictive analytics can optimize resource allocation, from managing bed occupancy rates to forecasting medication inventory needs. AI algorithms can anticipate patient admissions and discharges, enabling better staff scheduling and reducing bottlenecks in emergency departments.
Furthermore, chatbots and virtual health assistants powered by AI are enhancing patient engagement by providing 24/7 access to health information, appointment scheduling, and basic triage services. As these technologies become more sophisticated, they will play an increasingly vital role in reducing healthcare disparities by offering accessible support to underserved populations.

Ethical Considerations and Challenges in the Future of Artificial Intelligence in Healthcare
While the potential of AI in healthcare is vast, it is accompanied by a complex array of ethical considerations and challenges. One of the primary concerns revolves around data privacy and security. Healthcare data is inherently sensitive, and ensuring its protection from breaches or misuse is paramount. AI developers and healthcare institutions must implement robust cybersecurity measures and transparent data governance frameworks.
Bias in AI algorithms is another pressing issue. If training data is not representative of diverse populations, AI models can inadvertently perpetuate health disparities. Addressing algorithmic bias requires deliberate efforts to diversify datasets and implement fairness auditing mechanisms.
Additionally, the integration of AI raises questions about accountability and liability. In cases where an AI system’s recommendation leads to an adverse outcome, determining responsibility can be legally and ethically complex. Establishing clear guidelines and regulatory frameworks will be essential to navigate these uncharted waters.

Future of Artificial Intelligence in Healthcare: Training the Next Generation of Medical Professionals
As AI becomes increasingly embedded in healthcare, it is imperative to prepare the next generation of medical professionals for an AI-augmented future. Medical education must evolve to incorporate data literacy, machine learning fundamentals, and ethical considerations related to AI use. Clinicians will need to develop competencies in interpreting AI-generated insights and integrating them into patient care plans.
Interdisciplinary collaboration will be key, with physicians working alongside data scientists, engineers, and ethicists to co-create AI solutions that are clinically relevant and ethically sound. Continuous professional development programs will also play a crucial role in ensuring that practicing clinicians remain abreast of technological advancements.
The future of AI in medicine demands a workforce that is not only technically proficient but also critically reflective about the implications of AI on humanistic aspects of care. Cultivating empathy, communication skills, and ethical reasoning will remain as vital as ever, ensuring that technology enhances rather than diminishes the patient-provider relationship.
Integrating AI into Global Healthcare Systems: Opportunities and Challenges
Globally, the adoption of AI in healthcare presents both immense opportunities and significant challenges. In high-income countries, AI offers the potential to enhance efficiency, reduce costs, and improve patient outcomes. In low- and middle-income countries, AI could help bridge gaps in healthcare access by providing remote diagnostics, telemedicine services, and decision-support tools in resource-constrained settings.
However, disparities in technological infrastructure, regulatory readiness, and workforce capabilities pose hurdles to equitable AI integration. International collaborations, investment in digital health infrastructure, and capacity-building initiatives will be essential to ensure that the benefits of AI are shared broadly and inclusively.
Moreover, cultural considerations must be taken into account when deploying AI solutions across diverse populations. Tailoring AI applications to respect local values, health beliefs, and communication norms will be crucial for their acceptance and effectiveness.
Predictive Analytics and Preventive Care: The New Frontier
One of the most exciting frontiers for the future of artificial intelligence in healthcare lies in predictive analytics and preventive care. By analyzing vast datasets encompassing genetic information, lifestyle factors, and social determinants of health, AI can identify individuals at risk for developing chronic diseases long before symptoms arise.
Predictive models can inform targeted interventions, such as personalized wellness programs, behavioral coaching, and preemptive screenings. For example, AI-driven tools can predict the likelihood of a patient developing Type 2 diabetes based on patterns in their health records, enabling timely lifestyle modifications that could prevent disease onset.
The shift towards preventive care, supported by AI, promises to reduce the burden of chronic diseases, lower healthcare costs, and enhance population health. However, realizing this vision will require robust data-sharing frameworks, patient engagement strategies, and alignment of incentives across healthcare stakeholders.
The Role of AI in Drug Discovery and Development
The pharmaceutical industry stands to benefit immensely from AI, particularly in the domains of drug discovery and development. Traditional drug discovery is a time-consuming, costly endeavor with high rates of failure. AI has the potential to dramatically accelerate this process by identifying promising drug candidates, predicting their efficacy, and optimizing clinical trial designs.
Machine learning models can analyze biological datasets to uncover novel therapeutic targets, design molecules with desired properties, and simulate how new compounds will interact with biological systems. Additionally, AI can enhance patient stratification in clinical trials, ensuring that trials are more efficient and produce more meaningful results.
The future of AI in medicine may see the emergence of fully AI-driven drug discovery pipelines, reducing development timelines from decades to just a few years. Such advancements could bring lifesaving therapies to market faster and at lower costs, benefiting patients worldwide.
AI-Powered Robotics in Surgery and Rehabilitation
Robotic technologies, empowered by AI, are transforming surgical and rehabilitation practices. In the operating room, AI-guided robotic systems can assist surgeons by providing enhanced precision, stability, and real-time decision support. Minimally invasive procedures facilitated by robotics lead to faster recovery times, reduced complications, and improved patient satisfaction.
In rehabilitation, AI-driven exoskeletons and assistive devices are helping patients regain mobility and independence after injuries or neurological events such as strokes. These devices adapt to an individual’s unique biomechanics and progress, providing personalized support and feedback.
As AI continues to evolve, surgical robots may become even more autonomous, capable of performing certain procedures under human supervision. However, maintaining rigorous safety standards, regulatory oversight, and ethical guidelines will be critical to ensuring patient trust and well-being.
Telemedicine and Virtual Care: Expanding Access with AI
The COVID-19 pandemic catalyzed a rapid expansion of telemedicine and virtual care, trends that are poised to continue growing with the support of AI. Virtual care platforms augmented with AI can triage patients, recommend self-care measures, and escalate cases requiring in-person evaluation.
AI algorithms analyze patient-reported symptoms, medical histories, and even facial expressions during video consultations to assist clinicians in making accurate assessments. Moreover, remote patient monitoring devices equipped with AI can detect early signs of deterioration and prompt timely interventions.
The future of artificial intelligence in healthcare envisions a hybrid model where virtual and in-person care are seamlessly integrated, improving convenience, continuity, and outcomes for patients across diverse geographic and socioeconomic backgrounds.
Frequently Asked Questions: Breakthrough Insights into the Future of Artificial Intelligence in Healthcare
1. How is the future of artificial intelligence in healthcare expected to impact global health equity?
The future of artificial intelligence in healthcare is poised to significantly address global health disparities by providing advanced diagnostic and treatment tools in under-resourced areas. AI-powered mobile applications and telemedicine platforms can offer high-quality consultations to remote and underserved populations without requiring a physical healthcare infrastructure. Predictive analytics could help identify disease outbreaks early, allowing public health officials to respond more rapidly and allocate resources more effectively. Furthermore, AI translation tools can bridge language barriers between patients and healthcare providers, promoting inclusivity and reducing miscommunication. However, achieving true global equity will require concerted efforts to ensure that AI solutions are affordable, culturally appropriate, and ethically deployed.
2. What are some emerging fields where the future of AI in medicine is showing unexpected potential?
Beyond traditional healthcare domains, the future of AI in medicine is revealing surprising applications in areas like mental health support, palliative care, and geriatric management. AI chatbots are being refined to detect early signs of depression or anxiety based on language patterns and sentiment analysis, offering a supplementary layer of mental health care. In palliative settings, AI can help personalize comfort care plans based on patient data and predicted disease trajectories. For the elderly, AI-driven monitoring systems can detect subtle changes in movement or cognition, helping caregivers intervene before crises occur. These innovations illustrate that AI’s utility in medicine is expanding beyond clinical diagnosis to enhance holistic, patient-centered care.
3. What are “explainable AI” models, and why are they crucial for the future of artificial intelligence in healthcare?
Explainable AI (XAI) models are designed to provide transparent, understandable rationales for their decisions, making their outputs more interpretable to healthcare providers. In the context of the future of artificial intelligence in healthcare, XAI is critical because clinicians must trust and comprehend AI recommendations before integrating them into patient care. Traditional “black box” AI models often yield highly accurate results but lack transparency, posing risks when clinical stakes are high. By prioritizing explainability, healthcare systems can foster stronger human-machine collaboration, leading to more ethical and patient-safe deployments. Additionally, XAI facilitates better regulatory compliance, an essential factor as governments and organizations tighten oversight on medical AI technologies.
4. How will AI reshape patient autonomy and shared decision-making in the future of AI in medicine?
The future of AI in medicine is likely to empower patients by giving them greater access to personalized information and treatment options. AI-driven decision-support tools can present patients with tailored analyses of potential outcomes based on their specific profiles, fostering more informed discussions with healthcare providers. This democratization of knowledge encourages shared decision-making, where patients actively participate in selecting treatments aligned with their values and preferences. However, to fully realize this potential, efforts must be made to ensure AI tools present information in ways that are accessible and understandable to diverse patient populations. Training healthcare providers to navigate these conversations will also be pivotal for maintaining trust and clarity.
5. In what ways could AI change the structure of healthcare teams?
As the future of artificial intelligence in healthcare unfolds, healthcare teams are expected to become increasingly interdisciplinary, incorporating data scientists, AI specialists, ethicists, and human factors experts alongside traditional medical professionals. AI will automate certain routine clinical tasks, allowing physicians and nurses to focus more on complex patient interactions, holistic care, and critical decision-making. Additionally, new roles such as AI model validators, data stewards, and AI ethicists will emerge, ensuring that AI tools are effectively integrated and ethically managed. Training programs that foster cross-disciplinary collaboration will be essential for healthcare institutions seeking to thrive in an AI-augmented environment. These shifts will likely redefine professional boundaries and foster more dynamic, adaptable care teams.
6. How will the future of artificial intelligence in healthcare influence public health initiatives?
Public health initiatives will increasingly leverage the future of artificial intelligence in healthcare to anticipate and address population-wide health trends. Predictive modeling can identify communities at risk for emerging infectious diseases, chronic illnesses, or environmental health hazards, enabling targeted interventions before problems escalate. AI-driven simulations can help policymakers test the potential impacts of various public health strategies in a virtual environment, improving decision-making and resource allocation. Furthermore, natural language processing can analyze social media and online forums to detect public sentiment and misinformation, helping public health campaigns tailor their messaging more effectively. These applications promise to make public health efforts more proactive, data-driven, and responsive to real-time needs.
7. What are the potential psychological effects of AI integration on healthcare providers?
The future of AI in medicine will inevitably reshape the psychological landscape for healthcare providers, introducing both opportunities and challenges. On one hand, AI can alleviate cognitive burdens by managing repetitive tasks, reducing burnout, and freeing up time for more meaningful patient interactions. On the other hand, providers may experience “automation anxiety,” fearing loss of professional identity, deskilling, or diminished autonomy. Transparent communication about AI’s role, robust training programs, and active provider involvement in AI system design can help mitigate these concerns. Additionally, fostering a culture that values human intuition and empathy alongside technological prowess will be essential for maintaining provider well-being in an AI-enhanced healthcare environment.
8. How can AI address social determinants of health in future healthcare models?
AI has the potential to revolutionize how healthcare systems address social determinants of health (SDOH), which are often critical yet underappreciated drivers of patient outcomes. By analyzing non-medical data—such as housing stability, education level, and access to nutritious food—the future of artificial intelligence in healthcare can identify at-risk individuals and communities. AI models can then inform targeted interventions, such as connecting patients with social services, adjusting treatment plans to account for resource limitations, or advocating for policy changes. Moreover, integrating SDOH into clinical decision support systems ensures that care recommendations are truly holistic. To succeed, however, it is crucial that data collection respects patient privacy and that interventions are designed collaboratively with community stakeholders.
9. How might AI-driven healthcare innovations differ between urban and rural settings?
The future of AI in medicine will likely play out differently in urban versus rural environments due to disparities in infrastructure, resources, and patient demographics. In urban settings, AI might focus on optimizing complex hospital operations, managing high patient volumes, and enhancing specialty care through precision diagnostics. Conversely, in rural areas, AI applications are more likely to emphasize telehealth expansion, mobile diagnostic units, and decision-support tools that empower general practitioners to deliver specialized care remotely. Furthermore, rural deployments will need to address unique challenges such as limited broadband access and workforce shortages. Successful rural AI strategies will require customized solutions, sustainable investment, and strong community partnerships to bridge the healthcare gap.
10. What future innovations could further enhance the role of AI in personalized medicine?
The future of artificial intelligence in healthcare is on the cusp of ushering in even more sophisticated personalized medicine breakthroughs. Innovations like “digital twins”—virtual models of individual patients built using their genomic, proteomic, and clinical data—could allow doctors to simulate treatment outcomes before applying them in real life. Advanced wearable technologies, powered by AI, will continuously collect multidimensional health data, enabling hyper-personalized interventions that adapt in real-time. Additionally, integrating AI with CRISPR gene-editing techniques could open new avenues for highly targeted therapeutic strategies. As these innovations mature, they will push personalized medicine beyond reactive treatments toward truly predictive, preventive, and participatory care models, fundamentally transforming patient experiences and health outcomes.
Conclusion: Embracing the Future of Artificial Intelligence in Healthcare with Purpose and Prudence
The journey into the future of artificial intelligence in healthcare is one of immense promise, profound transformation, and thoughtful stewardship. As AI reshapes every facet of medicine—from diagnosis to treatment, from operations to patient engagement—it is imperative to harness its power responsibly and ethically. The integration of AI into healthcare systems must prioritize patient-centered care, equity, transparency, and continuous evaluation.
The future of AI in medicine will be defined not only by technological breakthroughs but also by the wisdom, compassion, and foresight with which we deploy these innovations. By embracing a collaborative, interdisciplinary approach and fostering a culture of ethical vigilance, we can ensure that AI fulfills its potential to enhance human health and dignity.
In this unfolding era, healthcare professionals, policymakers, technologists, and patients alike have a role to play in shaping a future where artificial intelligence serves as a force for good—a future where tomorrow’s medicine is not only smarter but also more humane, inclusive, and resilient.
Further Reading
What’s the Future of AI in Health Tech? Challenges, Opportunities, and What Comes Next
The future of AI in medicine and what it means for physicians and practices with Tom Lawry