Description
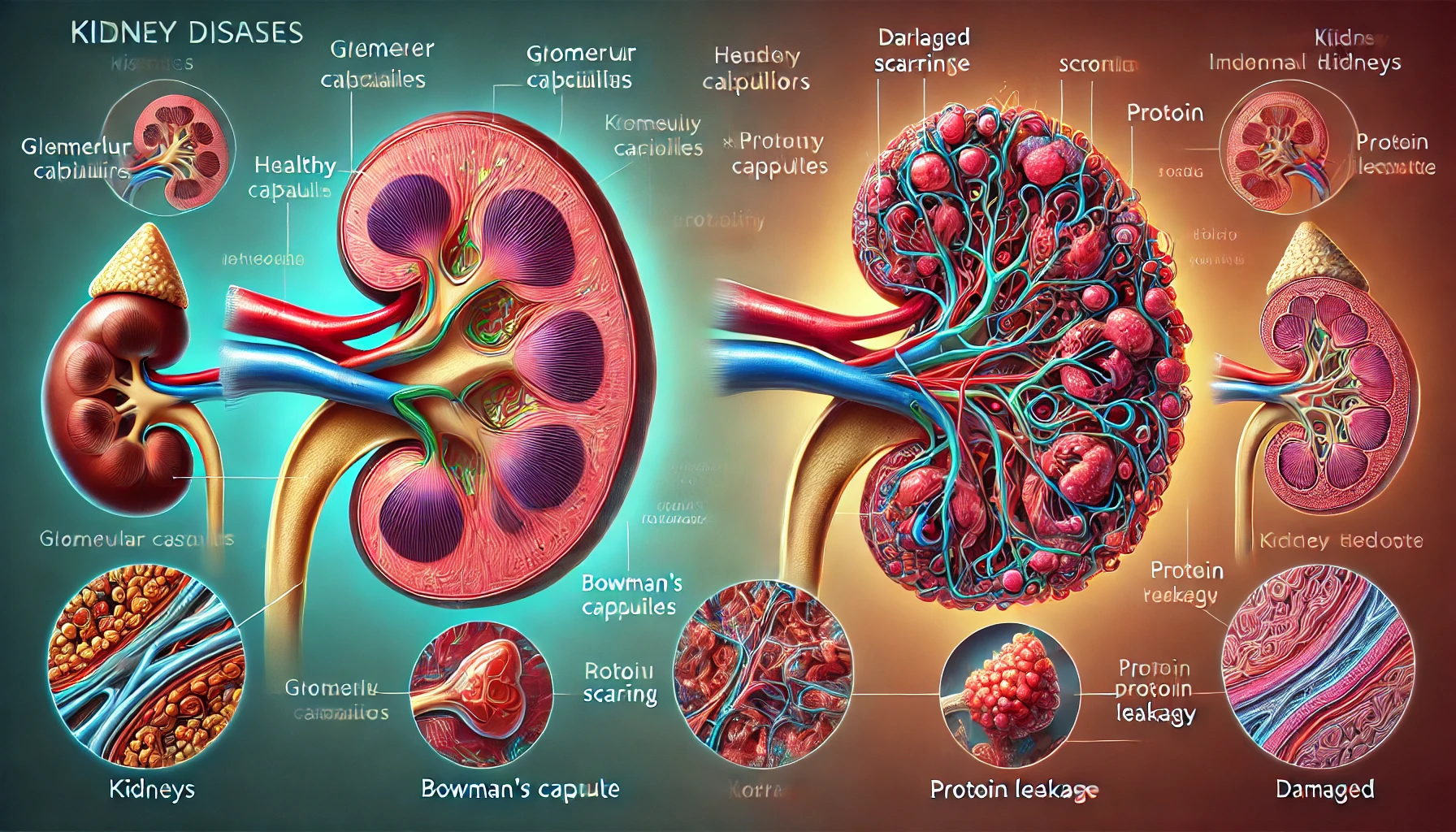
Glomerulonephritis, also called glomerular disease, represents a collection of kidney diseases characterized by swelling of the glomeruli (i.e., the filtering unit of the kidneys that filters blood). A cup-shaped formation called Bowman’s capsule is formed by finger-like extensions in podocytes, cells with specialized functions lining the capillaries, which allow selective transit of tiny molecules while blocking larger protein molecules and blood cell destruction.
Increased cellularity in the glomerulus or thickness of the basement membrane of the glomerular system includes two examples of structural damage frequently brought on by such inflammatory mechanisms in the glomeruli. Numerous things, such as infections, other systemic disorders, and malfunctions in the immune system, can cause this inflammation. Renal impairment and damage are possible outcomes of this acute or chronic condition.
You May Also Like:
Crohn’s disease (CD): Description, Causes, and Treatment Protocol
Glomerulonephritis: Description, Causes, and Treatment Protocol is an original (MedNewsPedia) article.
Possible Causes
Several reasons may lead to the onset of glomerulonephritis. Such causes include the following:
Infections: Post-infectious glomerulonephritis can be caused by infections, particularly those that come from viruses like HIV or bacteria like Streptococcus. The glomeruli are unintentionally damaged in these situations by the body’s immunological reaction to the infection. This type of glomerulonephritis must be managed promptly by treating the underlying infection.
Immunologic Mechanisms: A malfunctioning immune system that results in the production of immune complexes is one of the main causes of glomerulonephritis. When immune complexes—antibodies and antigens—deposit inside the glomeruli, an inflammatory reaction is set off. Many autoimmune illnesses, including IgA nephropathy and systemic lupus erythematosus (SLE), can cause this.
Medications and Toxins: Drug-induced glomerulonephritis can result from taking specific pharmaceuticals, including some antibiotics and nonsteroidal anti-inflammatory drugs (NSAIDs). Furthermore, exposure to pollutants like organic solvents and heavy metals might harm the glomeruli.
Systemic Diseases: Over time, systemic illnesses like diabetes and hypertension may aggravate glomerular damage. Elevated blood pressure levels can overstress the glomeruli, and unchecked diabetes can cause glucose byproducts to build up and damage the kidneys.

Exacerbating and Mitigating Factors
The glomerulonephritis’s course and severity can be affected by several aggravating and moderating factors. Individuals as well as medical professionals must be aware of these elements to successfully manage the disorders. The following list covers aggravating and alleviating factors giving rise to glomerulonephritis:
The exacerbating factors involve:
Smoking: As kidney disease, particularly glomerulonephritis, develops and progresses, smoking is a known risk factor. Smoking can worsen inflammation and make it more difficult for the body to mend damaged kidney tissue.
Hypertension (or High Blood Pressure): An individual’s prognosis for glomerulonephritis might be considerably worsened by high blood pressure. Overstretching the already damaged glomeruli is one of the main effects of high blood pressure.
Proteinuria: A typical sign of glomerulonephritis is excessive protein leaking into the urine, or proteinuria. While the disease’s symptoms and eventual outcome are similar, proteinuria can make matters worse by adding to the general loss of vital proteins, such as albumin, which can result in edema and weakened immunological function.
Exposure to Toxins: Organic solvents and heavy metals are two examples of environmental pollutants that can cause glomerulonephritis. Renal injury may result from the accumulation of these poisons in the body.
Chronic Disease: Presumptive patients, such as those with diabetes and hypertension, are more likely to develop glomerulonephritis or exacerbate pre-existing diseases. Hypertension can put stress on the glomeruli, and uncontrolled diabetes can cause an accumulation of glucose byproducts that are harmful to the kidneys.
Infections: In post-infectious glomerulonephritis, the immune system’s reaction to an infection may unintentionally harm the glomeruli. This is particularly common with bacterial infections.

The mitigating factors involve:
Lifestyle Modifications: Glomerulonephritis can be slowed down in its progression by implementing heart-healthy lifestyle practices like stopping smoking, eating a balanced diet, and engaging in regular exercise.
Blood Pressure Control: To mitigate glomerulonephritis, controlling hypertension is essential. Reducing the burden on the glomeruli and delaying the progression of the condition can be achieved by appropriately managing blood pressure through lifestyle changes and antihypertensive medication.
Proteinuria Management: Proteinuria can be controlled using medications including angiotensin receptor blockers (ARBs) and angiotensin-converting enzyme (ACE) inhibitors, which decrease urine protein leakage while safeguarding the glomeruli.
Dietary Modifications: Less protein and sodium in a kidney-friendly diet can ease the burden on the glomeruli. For tailored dietary advice, speaking with a nutritionist is advantageous.
Consistent Observation and Follow-Up: To identify changes and modify treatment strategies as necessary, routine nephrologist check-ups and renal function monitoring are significant.
Immunomodulatory Therapies: When glomerulonephritis is caused by an autoimmune condition, immunosuppressive drugs may lessen the glomeruli’s invasion by the immune system.
Dialysis and Transplantation of Kidneys: If end-stage renal disease has been reached by glomerulonephritis, dialysis or a kidney transplant might be required in extreme cases to substitute for lost kidney functioning and effectively control symptoms.
Standard Treatment Protocol
The interdisciplinary approach is commonly employed in the care of glomerulonephritis, with treatment procedures tailored to the individual’s illness severity and underlying etiology. The usual treatment for glomerulonephritis does, however, include several common components:
Immunosuppressive Therapy: These mostly consist of prescription drugs, such as corticosteroids like prednisone, which are frequently used to lessen glomerular inflammation. In patients with autoimmune-driven glomerulonephritis, additional immunosuppressive medications such as mycophenolate mofetil and cyclophosphamide may be recommended.
Blood Pressure Management: This can be done by:
Lifestyle Modifications
A low-sodium diet, frequent exercise, and quitting smoking are all recommended for patients to lead heart-healthy lifestyles.
Antihypertensive Medications
Drugs that lower proteinuria and lower blood pressure include angiotensin receptor blockers (ARBs), such as losartan, and angiotensin-converting enzyme (ACE) inhibitors, such as enalapril. They are essential in safeguarding the glomeruli.
Diuretics: They include prescription diuretics such as furosemide and hydrochlorothiazide, which are given to treat edema, or fluid retention, a usual indication of glomerulonephritis.
Proteinuria Management: These include drugs such as ARBs and ACE Inhibitors. These medications are used to manage proteinuria in addition to blood pressure regulation. They help stop future damage by widening blood arteries, which lessens the strain on the glomeruli.
Dialysis and Kidney Transplantations: When glomerulonephritis is in its advanced stages and renal function has substantially declined, dialysis (peritoneal dialysis or hemodialysis) might be needed to filter the autoimmune factors that cause kidney disease. Kidney transplantation is thought to be the best course of treatment in these situations.

Treatment Options
Certain lifestyle changes and adjunct therapies may enhance traditional treatments and enhance overall results in addition to the prescribed course of care. These supplemental treatments seek to control symptoms, enhance renal function, and minimize inflammation. The following are some of the additional therapy options for glomerulonephritis:
Nutritional Supplements: These are as follows:
Vitamin D
Supplemental vitamin D may be required if renal impairment impairs the body’s ability to convert vitamin D into its most active form. The balance of calcium and phosphate, as well as the general health of the bones, depend on this. However, a healthcare provider should be consulted on dosage and safety.
Omega-3 Fatty Acids
Fish oil supplements, which often contain omega-3 fatty acids, may have anti-inflammatory effects. They may lessen glomerular inflammation and shield the glomerulus from more harm. Nevertheless, before using supplements, patients should speak with a doctor because large amounts of supplements can interfere with other prescriptions or medical issues.
Coenzyme Q10 (CoQ10)
An antioxidant called CoQ10 may be able to safeguard renal function. Certain studies have indicated that it may have a positive impact on glomerulonephritis outcomes.
Dietary Modifications: These entail eating a kidney-friendly diet that is low in protein and sodium. Consuming food in this way can lessen the pressure on the glomeruli.
Natural and Herbal Remedies: These include the following:
Turmeric (Curcumin)
Curcumin, a powerful anti-inflammatory molecule, is the active ingredient in turmeric. Curcumin can reduce renal inflammation and shield the kidneys from additional harm, according to certain research. It is possible to take it as a supplement or include it in your diet.

Astragalus
A plant with potential immunomodulatory effects, astragalus is utilized in traditional Chinese medicine. To assist in controlling their immunological reaction, some glomerulonephritis patients take astragalus pills.
Nettle Leaf
The anti-inflammatory and diuretic effects of nettle leaf are well known. It can be purchased as tea or supplements. It is used by some people to relieve glomerulonephritis symptoms.
Dandelion Root
Being a diuretic, dandelion root may help lessen edema, or the retention of fluid. Tea, tinctures, and pills are just a few of the forms it comes in.
Stress Management: Prolonged stress might intensify inflammation and perhaps make glomerulonephritis worse. Relaxation exercises, mindfulness training, and meditation are examples of stress-reduction strategies that can enhance general well-being and facilitate medical care.
However, it is important to stress that even if these adjunct therapies could be beneficial, a healthcare physician should always be consulted and given the go-ahead before using them. The selection of supplemental therapies ought to be tailored to the individual requirements and state of health of the patient. Monitoring the course of glomerulonephritis and making any necessary modifications to treatment regimens require routine follow-up visits with a nephrologist or other member of the healthcare team.
Conclusion
Glomerulonephritis is a complex kidney condition marked by inflammation of the glomeruli, which impairs the kidney’s ability to filter blood effectively. The disease can arise from various causes, including infections, immune system dysfunction, systemic conditions, and environmental factors, and it can progress to chronic kidney disease or end-stage renal failure if left untreated. Early diagnosis and timely intervention are crucial for managing symptoms, slowing progression, and preserving kidney function.
Standard treatment protocols include immunosuppressive therapies, blood pressure control, diuretics, and in severe cases, dialysis or kidney transplantation. Complementary approaches, such as lifestyle modifications, stress management, dietary changes, and targeted nutritional supplements, can further support kidney health and enhance overall outcomes. Supplements like omega-3 fatty acids, vitamin D, and antioxidants, alongside natural remedies like turmeric and astragalus, may help reduce inflammation when used under medical supervision.

Additional resources for further reference
https://www.ncbi.nlm.nih.gov/books/NBK560644
https://www.nature.com/articles/s41577-022-00816-y
https://www.thelancet.com/article/S0140-6736(22)00461-5/fulltext
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.