Introduction
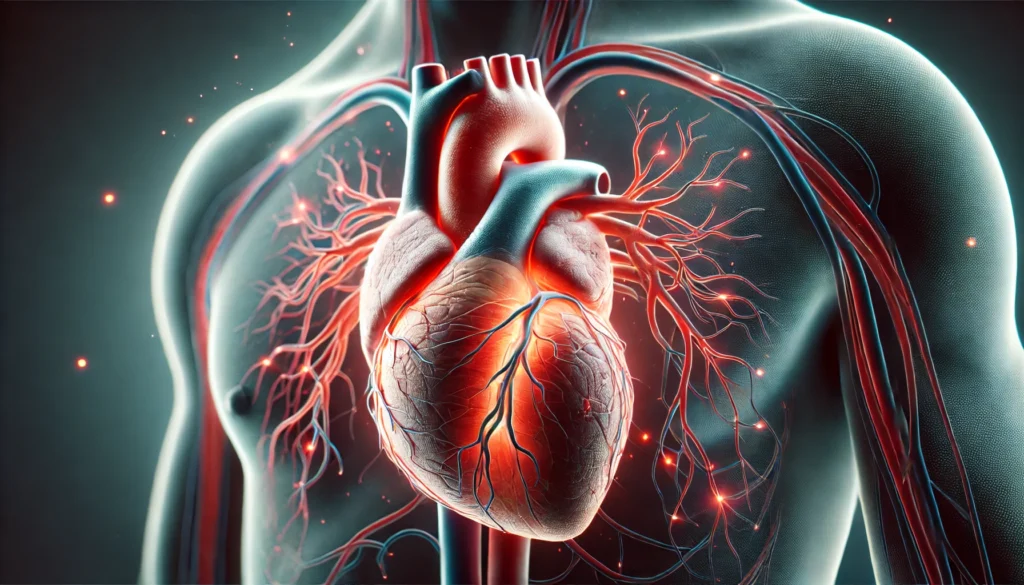
Heart disease remains one of the leading causes of mortality worldwide, affecting millions of people each year. The field of high-risk cardiology focuses on identifying and managing individuals who are at an increased likelihood of developing severe cardiovascular conditions. Understanding the five cardiac risk factors that contribute to heart disease is essential for both prevention and treatment. These risk factors include hypertension, high cholesterol, diabetes, smoking, and obesity. By exploring these key contributors in detail, we can gain insight into how lifestyle choices, medical interventions, and genetic predispositions interact to influence heart health. In this article, we will examine each of these risk factors comprehensively, highlighting their physiological effects, potential complications, and evidence-based strategies for mitigation.
You may also like: 5 Modern Treatments for Heart Disease: Advancements in Cardiac Care
The Impact of Hypertension on Cardiovascular Health
Hypertension, or high blood pressure, is one of the most significant risk factors for cardiovascular disease. It occurs when the force of blood against the artery walls remains consistently elevated, putting undue stress on the heart and blood vessels. Over time, this can lead to complications such as heart failure, stroke, and aneurysms. The insidious nature of hypertension is that it often presents with no noticeable symptoms until significant damage has occurred.
The relationship between hypertension and cardiovascular disease is well-documented in medical research. Elevated blood pressure levels can cause the heart to work harder than necessary, leading to left ventricular hypertrophy—a condition where the heart muscle thickens and loses its ability to pump efficiently. Additionally, hypertension accelerates the process of atherosclerosis, the buildup of fatty plaques within the arteries, which can lead to coronary artery disease and increased risk of heart attacks.
Managing hypertension involves a combination of lifestyle modifications and pharmacological interventions. Reducing sodium intake, maintaining a healthy weight, engaging in regular physical activity, and managing stress are essential lifestyle changes that can help lower blood pressure. Pharmacological treatments, such as ACE inhibitors, beta-blockers, and calcium channel blockers, are often prescribed to control hypertension effectively. Regular monitoring and early intervention are crucial to preventing the long-term consequences associated with high blood pressure.
The Role of High Cholesterol in Cardiovascular Disease
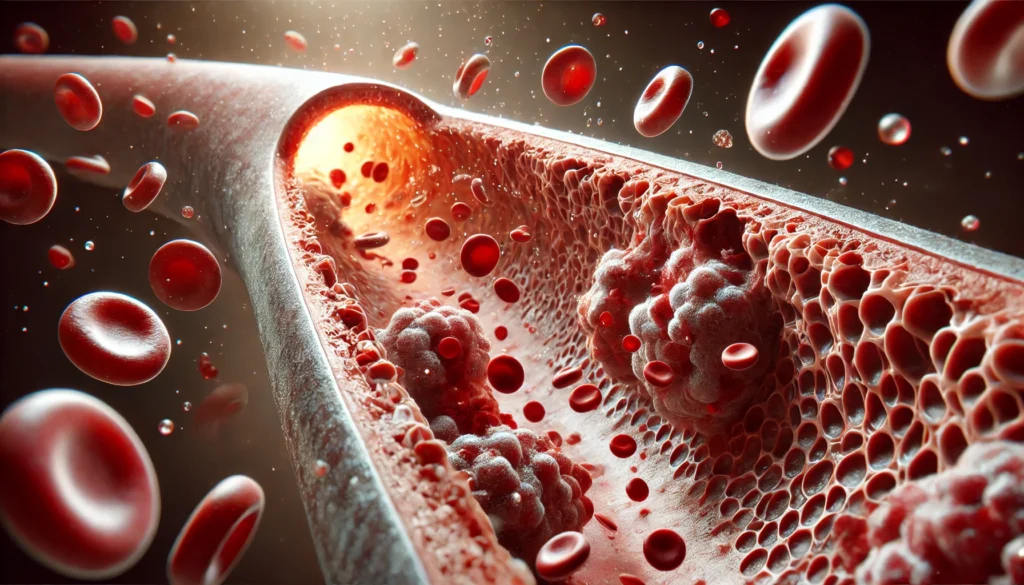
Cholesterol is a fatty substance found in the blood that plays a vital role in cell function and hormone production. However, when cholesterol levels become imbalanced—specifically when low-density lipoprotein (LDL) cholesterol is elevated—it can contribute to the development of atherosclerosis. This condition narrows the arteries, restricting blood flow and increasing the risk of heart attacks and strokes.
The interplay between cholesterol levels and cardiovascular risk is complex, as high-density lipoprotein (HDL) cholesterol is considered protective against heart disease. HDL cholesterol helps remove excess LDL cholesterol from the bloodstream, transporting it to the liver for excretion. When LDL levels remain persistently high, it promotes inflammation and oxidative stress within the arteries, further exacerbating cardiovascular risk.
Addressing high cholesterol requires a multifaceted approach, including dietary adjustments, exercise, and medication when necessary. Consuming a heart-healthy diet rich in unsaturated fats, fiber, and omega-3 fatty acids can help lower LDL cholesterol levels. Statins, a class of cholesterol-lowering medications, have been shown to significantly reduce cardiovascular events in high-risk individuals. Regular lipid panel screenings are crucial for monitoring cholesterol levels and making informed decisions about risk management.
The Link Between Diabetes and Cardiovascular Disease
Diabetes, particularly type 2 diabetes, is a well-established risk factor for cardiovascular disease. Chronically elevated blood sugar levels contribute to endothelial dysfunction, increased arterial stiffness, and systemic inflammation—all of which play a role in the progression of heart disease. Individuals with diabetes are two to four times more likely to develop cardiovascular complications compared to those without diabetes.
One of the primary mechanisms through which diabetes influences heart health is its impact on blood vessel integrity. Hyperglycemia, or high blood sugar, leads to glycation of proteins within the vascular system, reducing their functionality and increasing susceptibility to atherosclerosis. Additionally, diabetes is frequently associated with other cardiovascular risk factors, such as hypertension and dyslipidemia, compounding the overall risk.
Effective diabetes management is crucial for reducing cardiovascular complications. Maintaining tight glycemic control through dietary regulation, regular physical activity, and medication adherence can help mitigate the damage caused by high blood sugar levels. Emerging treatments, such as SGLT2 inhibitors and GLP-1 receptor agonists, have shown promise in reducing cardiovascular events in diabetic patients. A multidisciplinary approach involving endocrinologists, cardiologists, and primary care physicians is essential for optimizing heart health in individuals with diabetes.
The Dangers of Smoking on Heart Health
Smoking is one of the most preventable causes of cardiovascular disease, yet it remains a significant public health concern. The harmful chemicals in tobacco smoke contribute to oxidative stress, inflammation, and endothelial dysfunction, all of which accelerate the development of atherosclerosis. Smoking also promotes platelet aggregation, increasing the risk of blood clots that can lead to heart attacks and strokes.
The cardiovascular consequences of smoking extend beyond direct damage to blood vessels. Nicotine, the addictive component of tobacco, stimulates the sympathetic nervous system, leading to increased heart rate and blood pressure. Over time, this places additional strain on the cardiovascular system, heightening the likelihood of heart failure and arrhythmias.
Quitting smoking is one of the most effective ways to reduce cardiovascular risk. Within weeks of smoking cessation, blood pressure and circulation begin to improve, and within a year, the risk of coronary heart disease drops significantly. Various smoking cessation strategies, including nicotine replacement therapy, prescription medications like varenicline, and behavioral counseling, can aid individuals in overcoming nicotine dependence. Public health initiatives aimed at reducing smoking prevalence have demonstrated substantial benefits in lowering heart disease rates.
The Role of Obesity in Cardiovascular Disease
Obesity is a growing global epidemic that has profound implications for heart health. Excess body weight is associated with numerous metabolic disturbances, including insulin resistance, hypertension, and dyslipidemia—all of which contribute to an increased risk of cardiovascular disease. Additionally, obesity is linked to systemic inflammation and endothelial dysfunction, further exacerbating vascular damage.
One of the primary concerns associated with obesity is its impact on cardiac workload. The heart must work harder to supply oxygen-rich blood to an increased body mass, leading to structural changes such as left ventricular hypertrophy. Furthermore, obesity promotes the accumulation of visceral fat, which releases pro-inflammatory cytokines that contribute to atherogenesis and cardiovascular complications.
Addressing obesity requires a comprehensive lifestyle approach that includes dietary modifications, increased physical activity, and behavioral interventions. Reducing caloric intake, engaging in regular exercise, and adopting sustainable dietary patterns, such as the Mediterranean or DASH diet, have been shown to improve cardiovascular outcomes. In cases of severe obesity, medical interventions, including pharmacotherapy and bariatric surgery, may be necessary to achieve meaningful weight loss and risk reduction.

Frequently Asked Questions (FAQ) on High-Risk Cardiology and Cardiac Risk Factors
1. What is high-risk cardiology, and who should be concerned about it?
High-risk cardiology is a specialized branch of cardiovascular medicine that focuses on individuals with a significantly elevated likelihood of developing heart disease or experiencing severe cardiovascular events. Those who fall into this category often have multiple overlapping risk factors, such as hypertension, diabetes, and obesity. Individuals with a family history of early-onset cardiovascular disease or a history of previous heart-related complications should also be particularly vigilant. Preventative strategies in high-risk cardiology often involve aggressive lifestyle modifications, medical interventions, and regular monitoring. Early detection and proactive management can significantly reduce the likelihood of major cardiac events, even in those with a strong genetic predisposition.
2. How do the 5 cardiac risk factors interact to increase heart disease risk?
The 5 cardiac risk factors—hypertension, high cholesterol, diabetes, smoking, and obesity—often do not operate in isolation but rather exacerbate one another. For example, obesity can contribute to insulin resistance, increasing the risk of diabetes, which in turn accelerates the progression of atherosclerosis. Hypertension places additional strain on the cardiovascular system, making it more vulnerable to the harmful effects of high cholesterol and smoking. The cumulative impact of these risk factors amplifies the overall cardiovascular burden, leading to earlier onset and more severe disease. Addressing multiple risk factors simultaneously is crucial in high-risk cardiology to break the cycle of worsening heart health.
3. Why is hypertension considered one of the most dangerous cardiac risk factors?
Hypertension is often referred to as the “silent killer” because it typically presents no symptoms until significant cardiovascular damage has already occurred. Uncontrolled high blood pressure places immense stress on the arteries, increasing the risk of stroke, heart attack, and heart failure. Additionally, hypertension accelerates arterial stiffening, which further compromises circulation and raises the risk of ischemic events. High-risk cardiology emphasizes routine blood pressure monitoring and management strategies, including lifestyle modifications and medication when necessary. Without intervention, prolonged hypertension can lead to irreversible cardiac and renal complications.
4. Can someone have normal cholesterol levels but still be at high risk for heart disease?
Yes, cholesterol levels alone do not provide a complete picture of cardiovascular risk. Some individuals with normal LDL and total cholesterol levels may still be classified under high-risk cardiology due to factors such as chronic inflammation, poor arterial function, or metabolic disorders. The ratio of LDL to HDL cholesterol, the presence of small, dense LDL particles, and markers such as C-reactive protein (CRP) can offer deeper insight into an individual’s true cardiovascular risk. Additionally, genetic predispositions and lifestyle factors, such as poor diet and inactivity, can elevate heart disease risk even in those with seemingly normal cholesterol profiles. This highlights the importance of a comprehensive cardiovascular assessment beyond standard lipid panels.
5. How does diabetes specifically damage the cardiovascular system?
Diabetes increases cardiovascular risk through multiple mechanisms, including chronic inflammation, endothelial dysfunction, and abnormal lipid metabolism. Elevated blood sugar levels damage the inner lining of blood vessels, leading to reduced elasticity and increased susceptibility to plaque buildup. Diabetes also promotes an atherogenic lipid profile, characterized by high triglycerides and low HDL cholesterol, further accelerating heart disease progression. Individuals with diabetes are at an elevated risk of silent heart attacks, where symptoms may be absent or mild, delaying diagnosis and treatment. High-risk cardiology approaches often include aggressive blood sugar control, lifestyle modifications, and medications designed to reduce cardiovascular complications.
6. Why is smoking so harmful to heart health beyond its effects on the lungs?
While smoking is widely known for its detrimental impact on lung health, its effects on the cardiovascular system are equally severe. The chemicals in cigarette smoke damage arterial walls, increasing inflammation and promoting the buildup of fatty deposits. Smoking also enhances platelet aggregation, making blood more prone to clotting, which raises the risk of heart attacks and strokes. Additionally, nicotine exposure leads to increased heart rate and blood pressure, placing chronic stress on the heart. High-risk cardiology prioritizes smoking cessation as a critical intervention, as quitting smoking yields immediate and long-term cardiovascular benefits.
7. How does obesity contribute to heart disease beyond increasing blood pressure?
Obesity is a multifaceted risk factor that affects cardiovascular health in numerous ways. Excess adipose tissue, particularly visceral fat, releases inflammatory cytokines that contribute to endothelial dysfunction and arterial plaque formation. Obesity also increases the body’s demand for oxygenated blood, forcing the heart to work harder, which can lead to left ventricular hypertrophy and heart failure over time. Furthermore, obesity often coexists with metabolic syndrome, a cluster of conditions including insulin resistance and dyslipidemia, which further compound heart disease risk. High-risk cardiology interventions for obesity emphasize sustainable weight loss through dietary changes, physical activity, and, in some cases, medical or surgical interventions.
8. What are the most effective lifestyle changes for reducing high-risk cardiology concerns?
For individuals categorized under high-risk cardiology, lifestyle modifications are often the first line of defense against heart disease. The most impactful changes include adopting a heart-healthy diet, such as the Mediterranean or DASH diet, which emphasizes whole foods, lean proteins, and healthy fats. Regular physical activity, including both aerobic and resistance training, improves cardiovascular endurance and metabolic function. Stress management techniques, such as mindfulness and meditation, have been shown to reduce blood pressure and lower heart disease risk. High-risk individuals should also prioritize sleep quality, as poor sleep is linked to increased blood pressure and metabolic dysregulation. Consistency in these areas can yield significant improvements in cardiovascular outcomes.
9. How does high-risk cardiology incorporate new medical advancements?
High-risk cardiology is a rapidly evolving field that continuously integrates cutting-edge research and medical advancements to improve patient outcomes. Newer cholesterol-lowering drugs, such as PCSK9 inhibitors, provide additional options for individuals who do not respond well to statins. Advances in continuous glucose monitoring and personalized diabetes management have enhanced cardiovascular risk reduction for diabetic patients. Additionally, imaging technologies like coronary artery calcium scoring allow for earlier detection of atherosclerosis, enabling preemptive interventions. Researchers are also exploring the role of genetic testing in identifying individuals at heightened risk for cardiovascular disease, potentially paving the way for more tailored prevention strategies.
10. What is the future outlook for preventing heart disease in high-risk populations?
The future of high-risk cardiology is promising, with a growing emphasis on precision medicine and individualized treatment approaches. Advances in artificial intelligence and big data analytics are helping to refine risk prediction models, allowing for earlier and more targeted interventions. Gene therapy and regenerative medicine are also emerging as potential tools for repairing damaged heart tissue and reversing some aspects of cardiovascular disease. Public health initiatives aimed at reducing smoking rates, improving access to heart-healthy foods, and promoting physical activity are expected to play a crucial role in population-wide cardiovascular risk reduction. As research continues to uncover new therapeutic avenues, the ability to prevent and manage heart disease in high-risk individuals will only continue to improve.
Conclusion: Prioritizing Heart Health Through Risk Factor Management
Understanding and addressing the five cardiac risk factors—hypertension, high cholesterol, diabetes, smoking, and obesity—is crucial for preventing cardiovascular disease. Each of these factors contributes uniquely to heart disease progression, underscoring the importance of early intervention and comprehensive risk management strategies. By adopting a proactive approach that includes lifestyle modifications, medical treatments, and regular health screenings, individuals can significantly reduce their risk of heart disease. The field of high-risk cardiology continues to evolve, offering new insights and treatment options to improve cardiovascular outcomes. By prioritizing heart health, individuals can enhance their quality of life and reduce the burden of cardiovascular disease on a global scale.
cardiovascular health strategies, preventing heart disease, heart attack prevention tips, managing high blood pressure, cholesterol and heart health, diabetes and heart disease connection, smoking cessation benefits, obesity and cardiovascular risk, lifestyle changes for heart health, heart-healthy diet plan, exercise for heart disease prevention, stress management for heart patients, hypertension treatment options, cholesterol-lowering foods, diabetes management techniques, early signs of heart disease, cardiac risk assessment, metabolic syndrome and heart disease, inflammation and heart health, latest cardiology research
Further Reading:
Understand Your Risks to Prevent a Heart Attack
A Systematic Review of Major Cardiovascular Risk Factors: A Growing Global Health Concern
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


