Introduction: Rediscovering the Past to Understand the Present
The global rise in type 2 diabetes has triggered a renewed interest in understanding its origins, trajectory, and transformation through time. As both a metabolic and social condition, diabetes has existed in human records for thousands of years, yet it is only in recent decades that science has begun to unravel its intricate biological and environmental causes. By tracing the history of type 2 diabetes, we not only gain insight into the medical journey of this complex disease but also understand how modern tools, global collaboration, and public health awareness have shaped today’s landscape of treatment and prevention.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
This comprehensive exploration of the history of type 2 diabetes bridges ancient medical texts, Renaissance physiology, and twenty-first-century biotechnological innovations. In doing so, we discover how each diabetes discovery—from the first mention of “sweet urine” to genomic breakthroughs—has deepened our understanding and reshaped medical strategies. The journey is not just scientific; it is profoundly human, reflecting the evolving relationship between cultural beliefs, medical knowledge, and chronic illness.
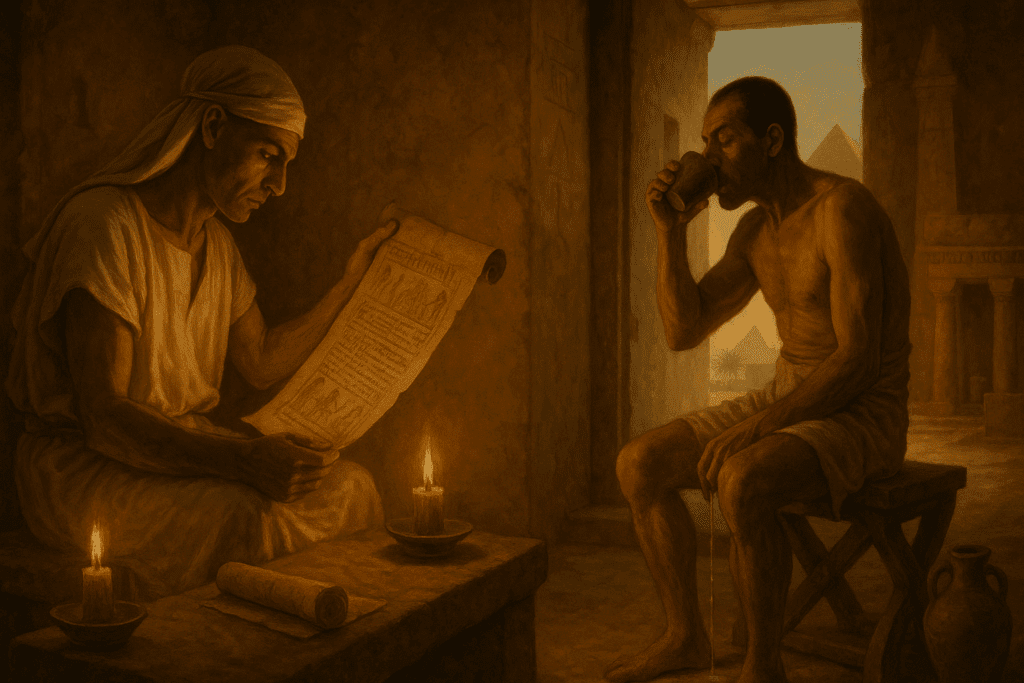
Ancient Descriptions and Observations of Diabetes-like Conditions
The earliest descriptions of diabetes-like conditions date back to ancient civilizations, particularly Egypt and India. Around 1550 BCE, the Ebers Papyrus—one of the oldest medical texts known—described a condition characterized by frequent urination. Similarly, ancient Hindu texts from around 1000 BCE described “Madhumeha,” meaning “honey urine,” a term used to describe what we now recognize as a symptom of diabetes. These early observations, while lacking modern scientific context, offered astute clinical recognition of what appeared to be a systemic disorder involving sugar metabolism.
In ancient Greece, the term “diabetes” was coined by Aretaeus of Cappadocia in the second century CE. He used the word to describe a condition where fluids seemed to pass through the body without being absorbed, leading to excessive urination, thirst, and emaciation. Though this description likely referred to both type 1 and type 2 diabetes, it reflected a growing awareness of metabolic irregularities. What makes this phase of the history of type 2 diabetes compelling is the reliance on empirical observation. Without the benefit of biochemical tools or lab diagnostics, early physicians inferred disease from bodily fluids, patterns of behavior, and physical symptoms—laying the groundwork for future diabetes discovery.
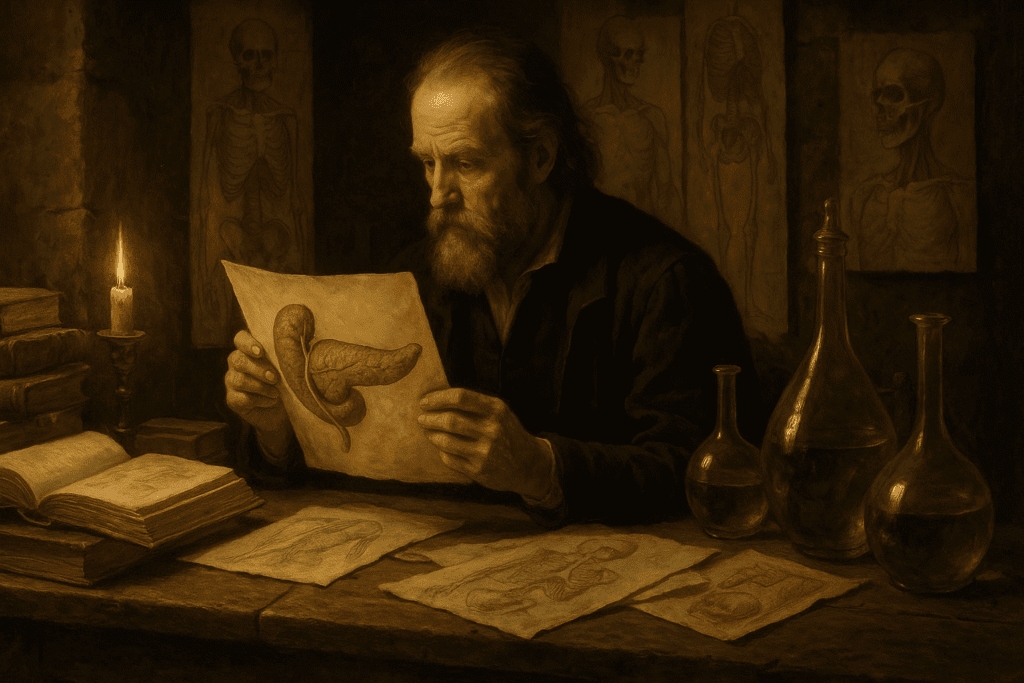
The Renaissance and Enlightenment Eras: First Steps Toward Scientific Understanding
The Renaissance ushered in a new era of anatomical and physiological inquiry, grounded in empirical investigation and human dissection. During this period, the pancreas was identified and anatomically described, although its function remained elusive for centuries. Thomas Willis, a 17th-century British physician, made one of the first distinctions between diabetes types by observing that some patients had sweet-tasting urine, while others did not. He postulated that “diabetes mellitus” (with sweet urine) was different from “diabetes insipidus,” a condition with similar symptoms but no sugar in the urine.
The Enlightenment further expanded the investigative lens. By the 18th and 19th centuries, physicians began using more sophisticated chemical analyses to detect sugar in urine. This era marked a significant turning point in the history of type 2 diabetes because it moved the condition out of the realm of mystery and superstition into that of quantifiable measurement. Despite lacking a cure or even a clear understanding of the disease’s etiology, this shift established diabetes as a discrete, identifiable pathology—setting the stage for later biochemical discoveries that would transform medicine.
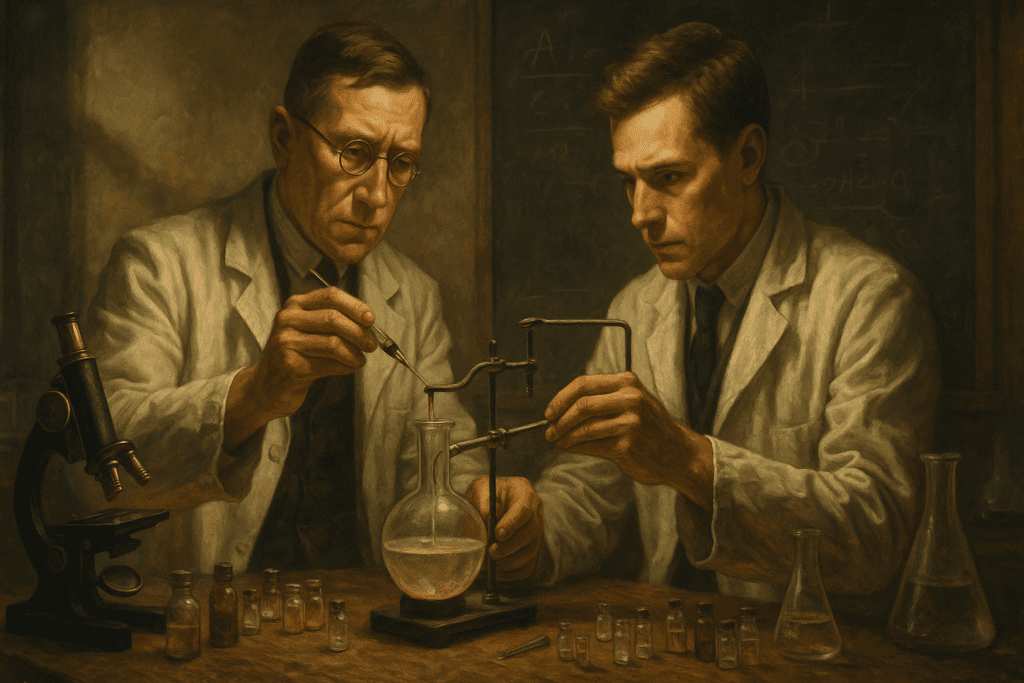
The Discovery of Insulin and Its Impact on Diabetes Classification
Perhaps no single diabetes discovery had a more profound impact on medicine than the isolation of insulin in 1921 by Frederick Banting and Charles Best, working under the guidance of John Macleod and assisted by James Collip. This groundbreaking achievement revolutionized the treatment of diabetes mellitus, particularly type 1, which until then had been a fatal diagnosis. However, insulin therapy also brought a clearer distinction between type 1 and type 2 diabetes.
Clinicians began to observe that not all patients required insulin to manage their symptoms. Many individuals, often older and overweight, could control their blood sugar through diet or oral medications, pointing toward a different pathophysiological mechanism. The discovery of insulin sharpened the diagnostic lens, allowing researchers to differentiate between insulin deficiency and insulin resistance. The history of type 2 diabetes shifted again, from one of symptom management to one involving underlying cellular mechanisms. As insulin became widely available, focus intensified on the varied presentations of diabetes, helping solidify our current understanding of type 2 as a disorder of impaired insulin sensitivity rather than absolute deficiency.
Epidemiological Insights and the Globalization of Type 2 Diabetes
By the mid-20th century, public health researchers began noticing rising rates of type 2 diabetes across multiple populations, particularly in urbanized and industrialized regions. In the 1960s and 1970s, epidemiological studies confirmed that lifestyle factors—especially diet, physical inactivity, and obesity—played major roles in type 2 diabetes onset. This global shift marked a key moment in the history of type 2 diabetes, as it expanded the disease from a niche medical concern to a full-fledged public health challenge.
Diabetes discovery during this era was no longer confined to laboratories. Population studies, like those conducted by the Framingham Heart Study and the World Health Organization, helped identify environmental and genetic risk factors. This broader lens allowed for a more comprehensive understanding of the disease’s determinants, from individual behaviors to social determinants of health. The rise of urban food deserts, processed foods, and sedentary lifestyles illuminated how modernization contributed to a growing diabetes epidemic. These insights laid the groundwork for modern public health interventions and prevention strategies, fundamentally altering the way healthcare systems addressed chronic diseases.
Genetic and Molecular Breakthroughs in the Late 20th Century
The last few decades of the 20th century saw a dramatic acceleration in diabetes discovery, largely driven by advances in molecular biology and genomics. Researchers identified numerous genes associated with insulin resistance, beta-cell dysfunction, and lipid metabolism, clarifying the multifactorial nature of type 2 diabetes. One of the most significant milestones was the discovery of the TCF7L2 gene, which plays a critical role in glucose regulation and has been consistently linked to increased type 2 diabetes risk across various populations.
This molecular turn in the history of type 2 diabetes revealed the complexity underlying its pathophysiology. Rather than a single-cause disorder, type 2 diabetes emerged as a multifactorial condition influenced by genetic predisposition, epigenetic changes, and environmental exposures. Studies in epigenetics began to show how prenatal conditions, such as maternal obesity or undernutrition, could influence gene expression in offspring, increasing lifetime diabetes risk. The scientific narrative expanded from glucose and insulin to include pathways involving inflammation, mitochondrial function, and gut microbiota—a transformation that continues to inform clinical and therapeutic developments today.
Technological Innovations in Monitoring and Managing Type 2 Diabetes
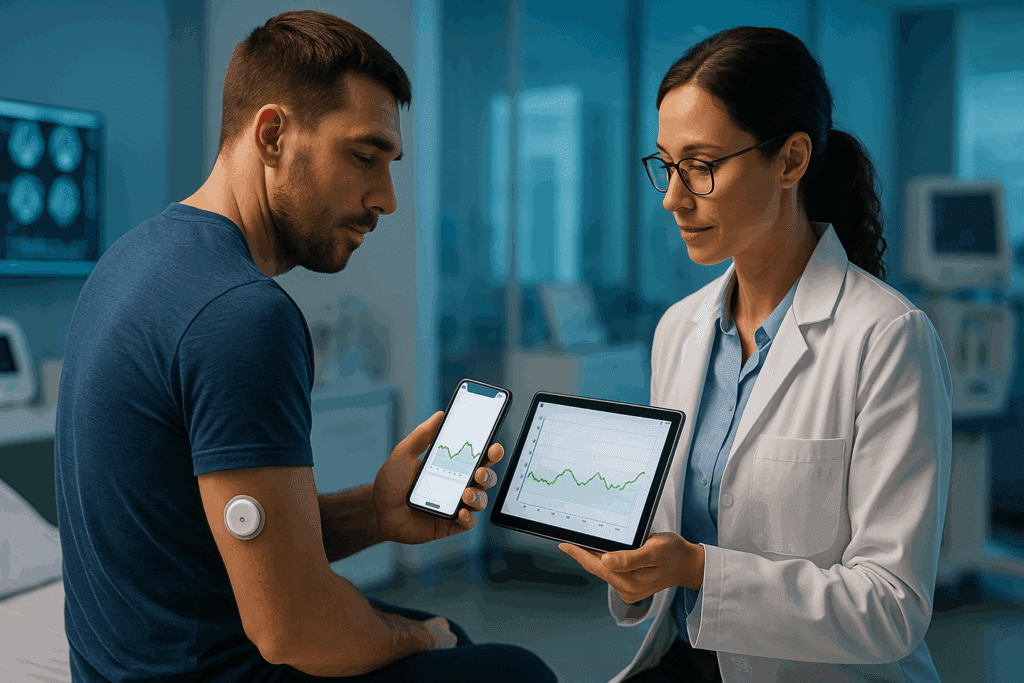
As scientific knowledge deepened, technological advancements transformed how type 2 diabetes was managed on a daily basis. The development of home blood glucose monitors in the 1980s gave patients unprecedented control over their health. Continuous glucose monitors (CGMs) and mobile health applications have since enabled real-time feedback, helping individuals and healthcare providers make more informed decisions.
Artificial intelligence and machine learning now assist in predicting blood glucose trends, optimizing treatment regimens, and identifying early signs of complications. Furthermore, closed-loop systems—also known as “artificial pancreas” technologies—are being tested in type 2 diabetes populations with insulin dependence. These breakthroughs represent more than just technological progress; they mark a profound change in how chronic disease is lived and managed. The history of type 2 diabetes is now intertwined with digital health, precision medicine, and personalized care, reflecting the intersection of biology, engineering, and patient-centered innovation.
Cultural, Socioeconomic, and Racial Disparities in Type 2 Diabetes Outcomes
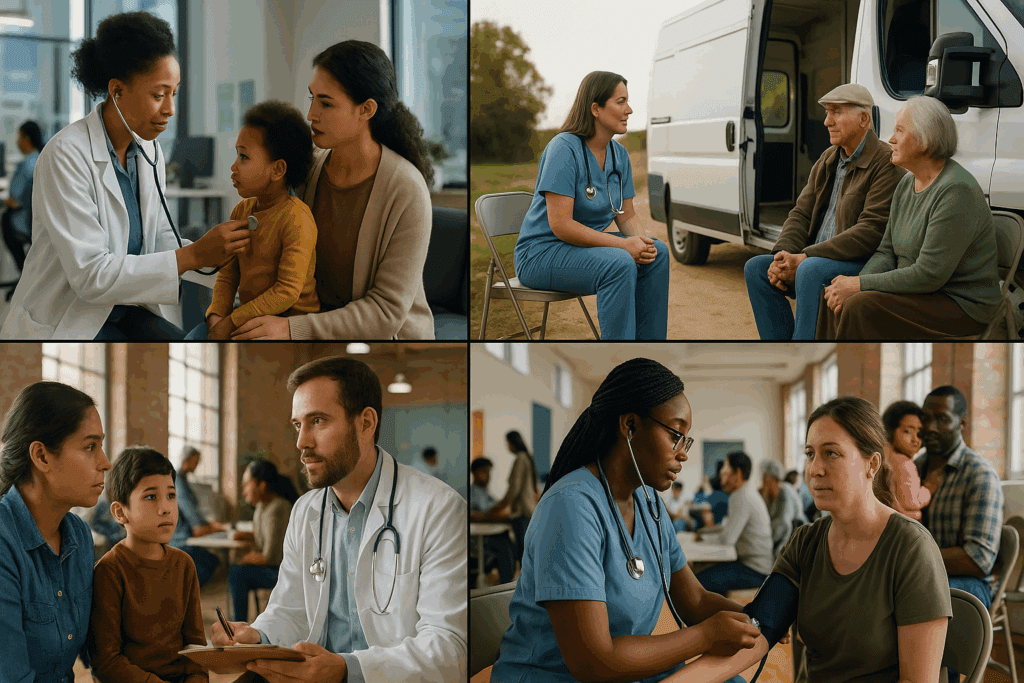
While biological research has advanced rapidly, disparities in type 2 diabetes outcomes remain deeply entrenched. Communities of color, indigenous populations, and those in lower socioeconomic strata often bear the brunt of the diabetes burden. Social determinants of health—including access to care, food insecurity, education, and neighborhood environments—exacerbate these inequities.
A crucial diabetes discovery in recent years has been the recognition that clinical care alone cannot address these disparities. Multidisciplinary approaches that integrate social work, community health, and culturally tailored education have shown promise in narrowing these gaps. Understanding the history of type 2 diabetes requires acknowledging how systemic inequities intersect with medical care. Historical marginalization, economic exclusion, and biased research practices have all contributed to unequal health outcomes, underscoring the need for equity-focused solutions in both research and policy.
The Emerging Role of Personalized Medicine and Future Research Frontiers
Looking forward, personalized medicine represents a new chapter in the history of type 2 diabetes. By integrating genetic profiles, metabolic biomarkers, and lifestyle data, researchers and clinicians aim to tailor interventions that are both more effective and more sustainable. No longer is treatment a one-size-fits-all approach. Instead, individualized care plans are being designed to reflect a patient’s unique biological and environmental context.
Pharmacogenomics is also reshaping diabetes care. Certain medications, such as GLP-1 receptor agonists and SGLT2 inhibitors, show variable responses based on genetic background. As precision medicine advances, these therapies may be fine-tuned to achieve optimal outcomes for diverse patient populations. Meanwhile, research continues into beta-cell regeneration, gut microbiome modulation, and even vaccine-based approaches for metabolic regulation. Each new diabetes discovery brings us closer to the goal of not just managing, but potentially reversing or preventing the disease altogether.
Frequently Asked Questions (FAQ): Exploring the History of Type 2 Diabetes and Breakthroughs in Diabetes Discovery
1. How did social attitudes toward type 2 diabetes evolve alongside scientific understanding?
Throughout the history of type 2 diabetes, public perception of the condition has undergone dramatic transformation. In earlier centuries, metabolic disorders were often misunderstood, shrouded in stigma, or incorrectly attributed to moral weakness or overindulgence. As diabetes discovery progressed—especially with advancements in diagnostics, endocrinology, and nutritional science—so did public awareness and empathy toward those managing the condition. Today, while stigma persists in some communities, public health campaigns and advocacy efforts have helped reframe type 2 diabetes as a complex interplay of genetic, lifestyle, and social determinants rather than a reflection of personal failure. Understanding this shift is crucial for fostering patient empowerment and reducing the psychological burden of living with a chronic illness.
2. What roles did traditional healing systems play in managing early diabetes-like symptoms?
Long before modern medical classifications, traditional systems like Ayurveda, Traditional Chinese Medicine (TCM), and Unani addressed symptoms we now associate with type 2 diabetes. These ancient frameworks often interpreted excessive thirst, frequent urination, and fatigue through holistic paradigms that involved imbalances in bodily humors or elemental forces. While these models lack the biochemical specificity achieved through modern diabetes discovery, they contributed to the broader history of type 2 diabetes by offering early recognition and lifestyle-based interventions. Herbal remedies, dietary restrictions, and mind-body practices formed the basis for managing symptoms. Contemporary researchers are increasingly studying these ancient remedies for potential bioactive compounds that may complement current therapies.
3. How has the history of type 2 diabetes influenced our current dietary guidelines?
The development of dietary recommendations has been profoundly shaped by evolving knowledge from every stage of the history of type 2 diabetes. Initial advice focused on sugar restriction alone, but scientific breakthroughs in metabolism, glycemic index, and macronutrient interaction have expanded this view. Modern guidelines now emphasize whole grains, fiber-rich foods, unsaturated fats, and controlled carbohydrate intake, rooted in decades of diabetes discovery. Moreover, longitudinal dietary studies have helped clarify that one-size-fits-all approaches are ineffective, leading to culturally sensitive and personalized nutrition plans. This progression underscores how historical context and scientific advancement have converged to inform today’s evidence-based dietary strategies.
4. What new frontiers in diabetes discovery could reshape type 2 diabetes treatment in the next decade?
Future breakthroughs may emerge from several promising research areas, including beta-cell regeneration, immunomodulation, and gut microbiome engineering. As the history of type 2 diabetes continues to unfold, precision medicine is taking center stage, supported by advances in metabolomics, AI-driven diagnostics, and wearable health technologies. Novel therapeutic targets are also being explored through systems biology, where cellular signaling pathways are mapped to reveal new intervention points. Epigenetic therapies, still in early development, could provide treatments that adjust gene expression related to insulin sensitivity without altering the genetic code itself. These innovative directions not only expand the scope of diabetes discovery but also redefine what it means to manage, prevent, or even reverse type 2 diabetes.
5. How have environmental exposures factored into the historical development of type 2 diabetes?
Environmental contributors to type 2 diabetes extend beyond diet and physical activity. Exposure to endocrine-disrupting chemicals such as bisphenol A (BPA) and phthalates has been linked to insulin resistance and metabolic dysfunction. This dimension of the history of type 2 diabetes reveals how industrialization, urbanization, and changes in agricultural practices have subtly but significantly influenced disease prevalence. Air pollution, for instance, has been associated with increased inflammation and diabetes risk. These findings add nuance to our understanding of diabetes discovery, underscoring the importance of public policy, urban planning, and ecological health in comprehensive diabetes prevention strategies.
6. In what ways has the history of type 2 diabetes intersected with women’s health and gender-specific research?
Although type 2 diabetes affects all genders, its expression, risk factors, and complications can differ significantly between men and women. Historical clinical trials often underrepresented women, limiting early insights into gender-specific outcomes. Recent diabetes discovery has corrected this gap by highlighting how hormonal fluctuations, pregnancy-related insulin resistance, and conditions like polycystic ovary syndrome (PCOS) contribute to unique diabetes risks in women. Furthermore, psychosocial factors, including caregiving burdens and healthcare access disparities, have historically affected how women manage the disease. Ongoing research is now exploring how estrogen and other sex hormones influence insulin sensitivity and cardiovascular outcomes in diabetic women, offering gender-informed paths to prevention and care.
7. How have Indigenous communities contributed to the broader understanding of diabetes management?
Indigenous knowledge systems have long emphasized the interdependence of community, environment, and health—a perspective now gaining renewed attention in diabetes research. While type 2 diabetes has disproportionately impacted many Indigenous populations due to colonial disruption and socio-economic inequality, these communities also offer culturally grounded practices that can inform holistic care. From plant-based medicine to land-based physical activity and communal eating practices, Indigenous frameworks highlight sustainability and prevention over reactive treatment. Their lived experiences add a critical layer to the history of type 2 diabetes, reminding us that effective solutions must integrate cultural wisdom with biomedical innovation. Efforts to co-create research agendas with Indigenous scholars represent a significant step forward in inclusive diabetes discovery.
8. What is the psychological toll of type 2 diabetes, and how is it being addressed in modern care models?
The psychological impact of type 2 diabetes is profound, encompassing stress, anxiety, depression, and diabetes-related distress. Historically, the biomedical model treated diabetes as a purely physiological condition, often neglecting emotional well-being. However, a growing body of evidence has shifted diabetes discovery toward integrated care models that include mental health support as a core component. Today, diabetes self-management education often includes behavioral therapy, peer support, and cognitive reframing techniques. Recognizing mental health as part of the history of type 2 diabetes not only improves outcomes but also reduces burnout for patients navigating a lifelong condition.
9. How are wearable technologies changing the patient experience and scientific understanding of type 2 diabetes?
The rise of wearable health devices has transformed both personal and clinical engagement with diabetes management. Continuous glucose monitors (CGMs), smartwatches, and mobile applications provide real-time data, empowering users to identify trends, triggers, and progress in their glycemic control. These tools also enrich diabetes discovery by generating vast datasets that researchers use to refine algorithms and treatment protocols. Beyond convenience, wearables reduce the emotional burden of uncertainty and improve medication adherence through timely alerts and personalized feedback. The integration of this technology into the history of type 2 diabetes reflects a shift toward patient-centered care grounded in actionable insights.
10. Why is it important to examine the history of type 2 diabetes through multiple disciplinary lenses?
Understanding the history of type 2 diabetes requires more than just medical expertise; it demands input from sociology, anthropology, public health, economics, and ethics. This multidisciplinary perspective uncovers the societal structures and cultural beliefs that have shaped diabetes care and disparities over time. Each new diabetes discovery is situated within a broader context that includes historical power dynamics, health policy evolution, and shifts in societal values. For example, the commercialization of food, racialized healthcare access, and global trade policies have all influenced how the disease manifests and is treated across populations. Looking through multiple lenses not only enriches our comprehension but ensures that future solutions are inclusive, equitable, and culturally resonant.
Conclusion: Reflecting on the Evolution and Future of Diabetes Discovery
The journey through the history of type 2 diabetes reveals far more than the evolution of a single disease. It reflects the cumulative progress of medicine, public health, technology, and human understanding. From ancient descriptions of sweet-tasting urine to the genomic mapping of disease risk, each phase of diabetes discovery has expanded our capabilities and redefined our challenges. Today, we stand at a critical juncture, where the promise of personalized medicine and digital health could reshape outcomes for millions worldwide.
Yet, the story is far from over. As the burden of type 2 diabetes continues to grow, particularly in vulnerable and underserved populations, the need for inclusive, multidisciplinary solutions becomes ever more urgent. By grounding future innovations in the lessons of the past, we can move toward a future where diabetes care is not only more effective but also more equitable. The history of type 2 diabetes is not merely a chronicle of scientific progress—it is a call to action, a testament to resilience, and a blueprint for discovery still to come.
Further Reading:
Diabetes: Past treatments, new discoveries
The Fascinating History of Diabetes
History of Diabetes: From Ancient Egypt to Modern Medicine
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.