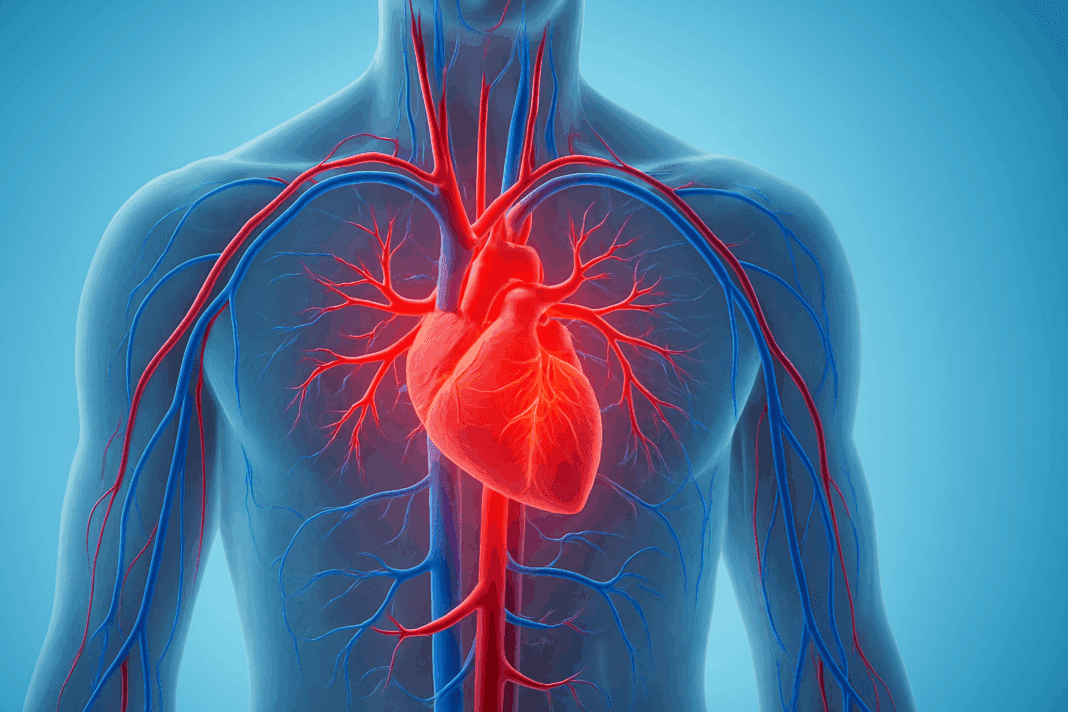
Blood pressure is a fundamental component of human physiology, playing a central role in the distribution of oxygen and nutrients throughout the body. The relationship between blood pressure and blood flow is essential to understanding not only how the cardiovascular system functions, but also how various conditions may disrupt this delicate balance. In this article, we will explore the intricate mechanisms that govern blood pressure and circulation, delve into the types of blood vessels involved in regulation, and examine the physical forces that drive the flow of blood through the human body. With a focus on scientific accuracy and reader accessibility, this discussion will also highlight the broader implications of blood pressure control for cardiovascular health.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Defining Blood Pressure and Its Function in the Cardiovascular System
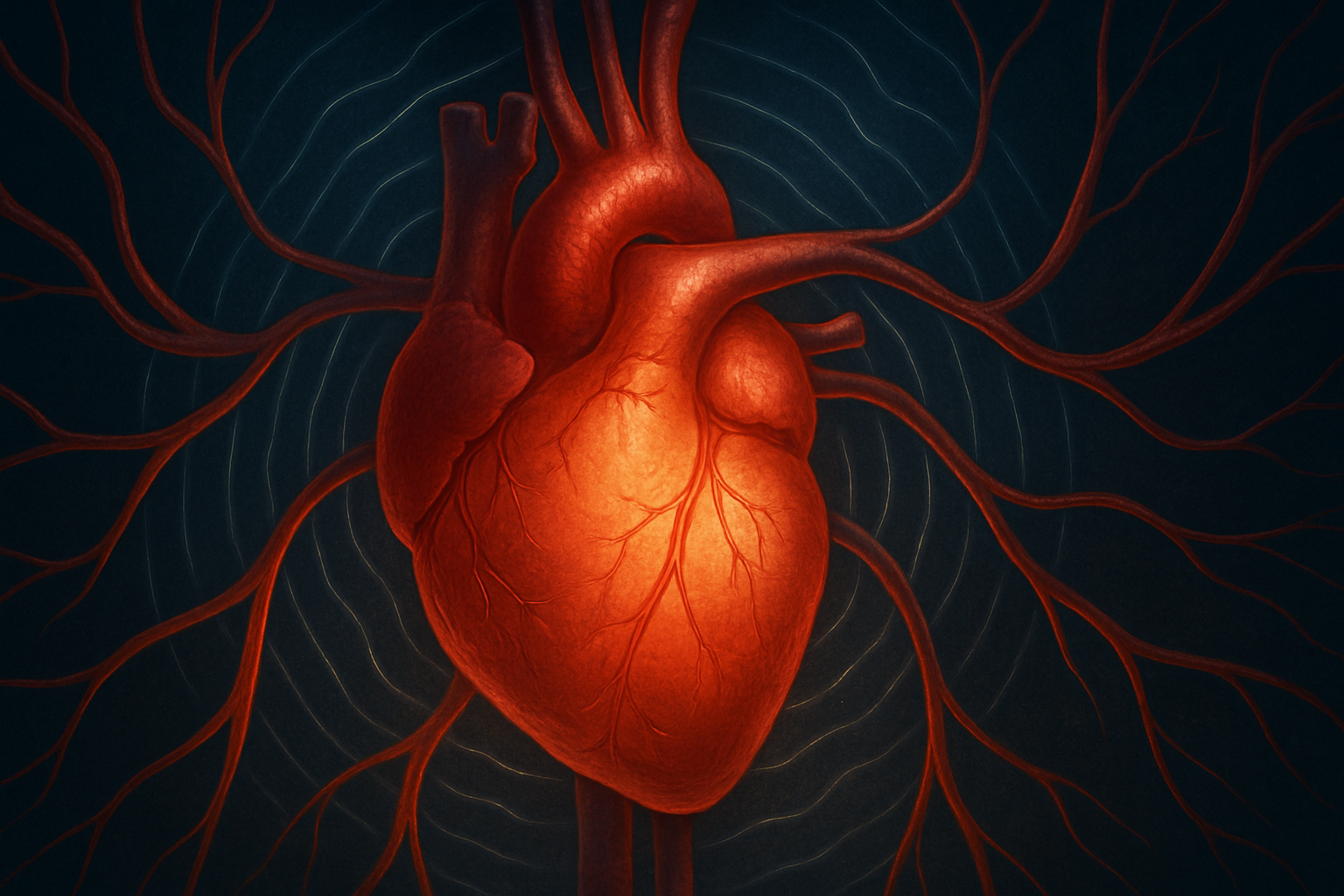
To appreciate how blood pressure affects blood flow, one must first understand what blood pressure is and the role it plays in the cardiovascular system. Blood pressure is defined as the force of blood against arterial walls as the heart pumps it through the body. This pressure is not constant; it fluctuates with each heartbeat, rising during systole (when the heart contracts) and falling during diastole (when the heart relaxes). In human anatomy, blood pressure serves as a key mechanism for pushing blood through the vast network of blood vessels that deliver oxygen and nutrients to tissues and organs.
In the context of cardiovascular system blood pressure, the function is multifaceted. It not only propels blood forward but also enables the exchange of gases, hormones, and waste products at the capillary level. Without adequate blood pressure, tissues may become ischemic, while excessive pressure can damage vessel walls and increase the risk of stroke or heart attack. The balance between pressure and flow is therefore a cornerstone of circulatory system health.
Blood Flow and the Principle of Pressure Gradients
One of the most basic yet critical principles in cardiovascular physiology is that blood flows from areas of higher pressure to areas of lower pressure. This concept answers the common query: does blood flow from high to low pressure heart? The answer is unequivocally yes. Blood ejected from the heart’s left ventricle enters the aorta, where pressure is highest, and then travels through arteries, arterioles, capillaries, venules, and finally veins, where pressure is lowest.
This pressure gradient is what drives blood through the entire circulatory system. In which vessel is blood pressure the highest? The answer is the aorta, immediately following left ventricular contraction. By the time blood reaches the capillaries and veins, the pressure has decreased significantly. This decrease is crucial for facilitating nutrient exchange and eventual return of deoxygenated blood to the heart. Blood pressure in the veins is relatively low, which is why additional mechanisms like muscle contraction and venous valves are needed to aid venous return.
Types of Blood Vessels and Their Roles in Regulating Pressure
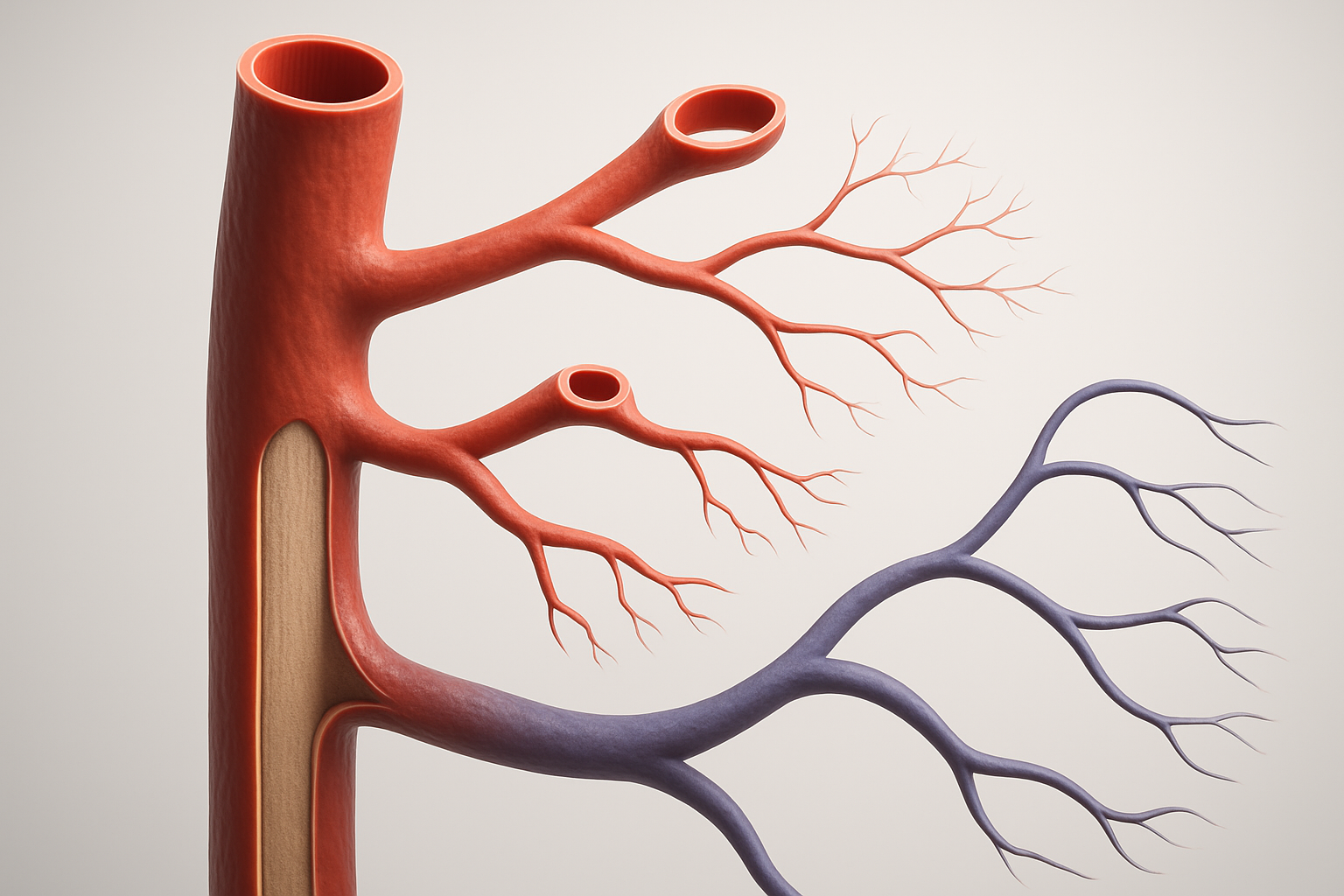
The vascular system is composed of various types of blood vessels, each with a distinct role in maintaining blood pressure and ensuring efficient circulation. Arteries, arterioles, capillaries, venules, and veins each contribute uniquely to the regulation of pressure and flow. When asking what type of blood vessel regulates blood pressure, the arterioles emerge as the primary regulators. These small-diameter vessels possess muscular walls that can constrict or dilate in response to neural and chemical signals.
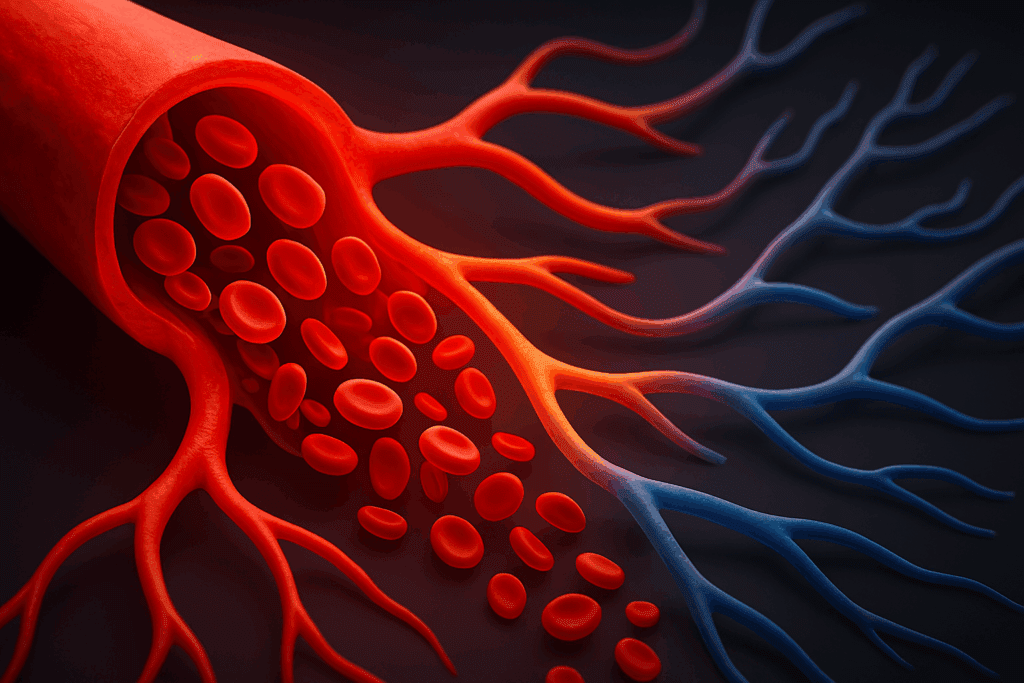
This ability to change diameter—known as vasoconstriction or vasodilation—directly influences resistance and, consequently, blood pressure. Arterioles serve as the main control points for adjusting flow to specific tissues based on metabolic demand. Capillaries, in contrast, are where the actual exchange of gases and nutrients occurs, and blood pressure in the capillaries must be sufficiently low to allow for efficient exchange without damaging delicate endothelial cells.
Meanwhile, veins are more compliant and serve as blood reservoirs. Although blood pressure in the veins is low, their large volume capacity plays a significant role in overall circulatory stability. Blood pressure is usually measured in what blood vessel? The standard measurement is taken from a brachial artery, typically located in the upper arm, because it provides a reliable representation of systemic arterial pressure.
The Physical Forces Behind Blood Pressure
Blood pressure is the result of two primary physical forces: cardiac output and peripheral resistance. These two components answer the common question: what are the two physical forces that cause blood pressure? Cardiac output refers to the volume of blood the heart pumps per minute, while peripheral resistance is the opposition to blood flow offered by the blood vessels, particularly the arterioles.
An increase in either cardiac output or peripheral resistance will elevate blood pressure. Conversely, reductions in these forces will cause blood pressure to fall. The force of blood against arterial walls is not simply a passive occurrence; it is a dynamic interplay of heart function and vessel tone. This understanding is essential in managing conditions such as hypertension, where one or both of these forces may be abnormally elevated.
Understanding how is blood pressure produced requires an integrated view of cardiovascular function. It begins with ventricular contraction, which propels blood into the arteries, creating a surge of pressure. This is followed by a relaxation phase, during which arterial elasticity helps maintain continuous blood flow. The net result is a pulsatile but steady movement of blood throughout the body.
Blood Pressure in Different Regions of the Circulatory System
Blood pressure is not uniform throughout the circulatory system. The highest pressures are found in the large arteries closest to the heart, such as the aorta. The pressure gradually declines as blood moves through the arterial tree and into the microcirculation. Blood pressure in the capillaries is significantly lower than in arteries, which is beneficial because it protects fragile capillary walls and facilitates nutrient exchange.
The gradual decline continues into the venous system. Blood pressure in the veins is typically very low, often close to zero near the right atrium of the heart. This low pressure presents a physiological challenge, necessitating mechanisms such as skeletal muscle contractions and thoracic pressure changes during respiration to aid venous return. When discussing pressure in the arteries when the heart is at rest, this is referred to as diastolic pressure, which provides a baseline pressure between heartbeats.
This spatial distribution of pressure is critical for efficient circulation. Blood pressure flow depends on these gradients, and any disruption—such as arterial stiffness, blockages, or venous insufficiency—can compromise tissue perfusion. Monitoring blood pressure in circulatory system health assessments thus provides insights into potential dysfunctions across the vascular continuum.
Mechanisms of Blood Pressure Regulation in the Human Body
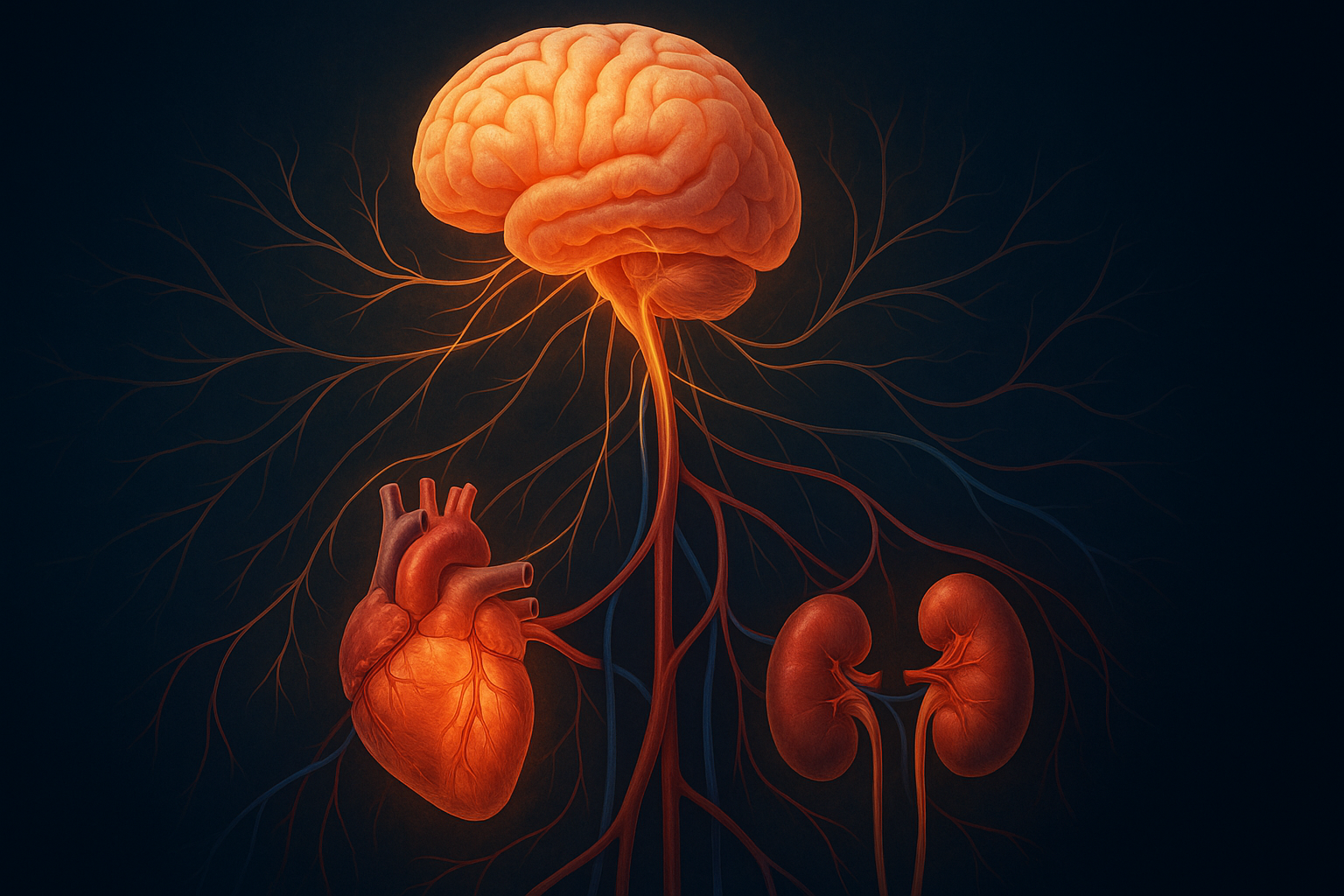
The body has evolved sophisticated mechanisms to regulate blood pressure and maintain homeostasis. Central to these mechanisms are neural, hormonal, and renal controls. When discussing how does the body control blood pressure, it is important to recognize the role of baroreceptors—specialized pressure sensors located in the carotid sinuses and aortic arch. These receptors send signals to the brainstem, which adjusts heart rate and vascular tone in response to changes in pressure.
Hormonal regulation is equally vital. The renin-angiotensin-aldosterone system (RAAS) is a key player in long-term blood pressure control. When blood volume or sodium levels drop, the kidneys release renin, which initiates a cascade resulting in vasoconstriction and sodium retention. These responses help restore blood pressure to normal levels. The sympathetic nervous system can also rapidly increase blood pressure by constricting blood vessels and increasing heart rate during stress or physical exertion.
Renal function cannot be overlooked in the discussion of how blood pressure is created and sustained. The kidneys regulate blood volume by adjusting urine output, thereby influencing blood pressure indirectly. Dysfunction in any of these regulatory systems can lead to chronic hypertension or hypotension, both of which carry significant health risks.
The Relationship Between Blood Pressure and Blood Flow
The relationship between blood pressure and blood flow is central to cardiovascular health. Many people ask: how are blood pressure and blood flow related? The answer lies in the principles of hemodynamics. Blood flow is directly proportional to the pressure gradient between two points and inversely proportional to vascular resistance. This means that even small changes in pressure or resistance can dramatically affect flow.
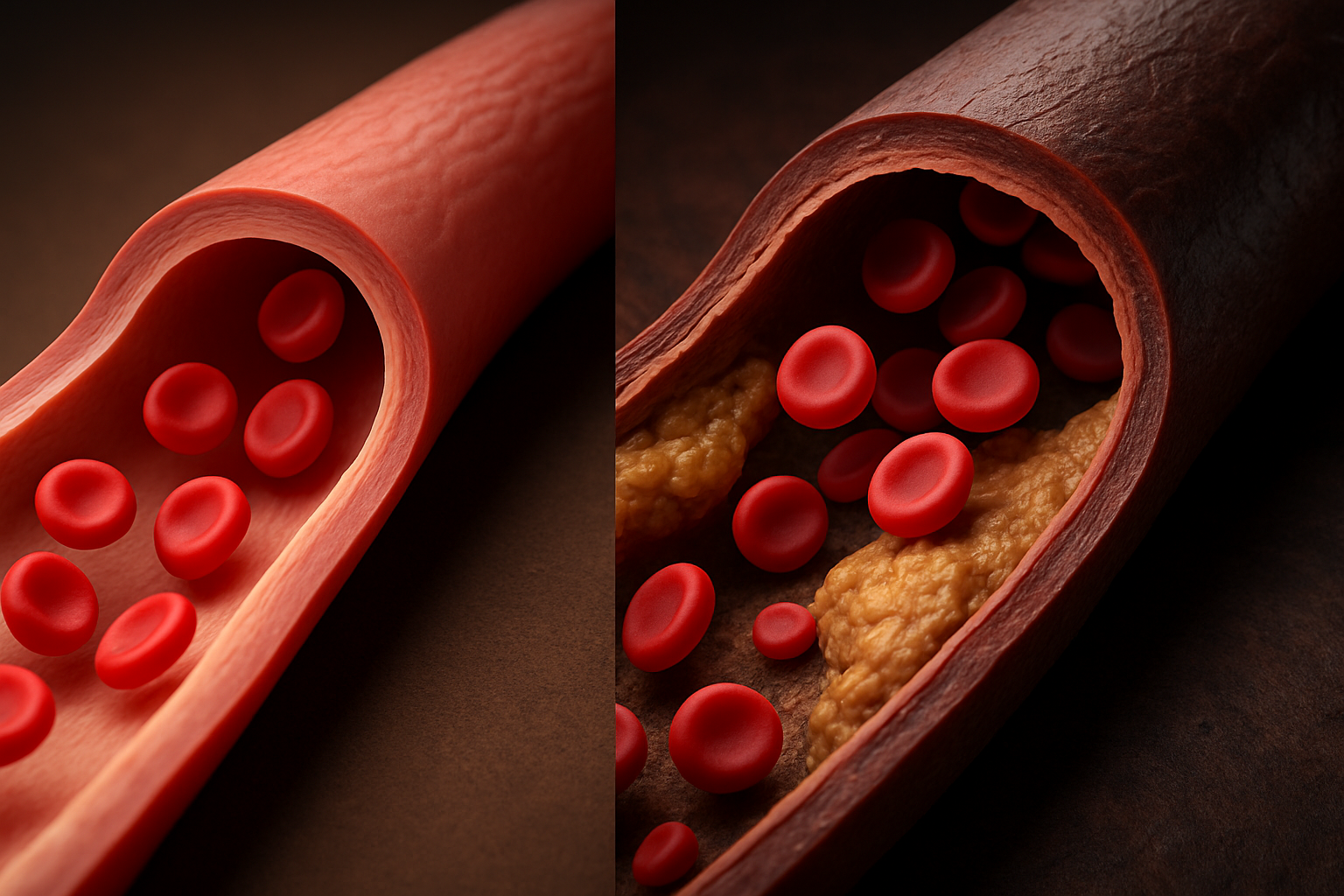
For instance, during physical activity, arterioles dilate in active muscles, reducing resistance and allowing greater blood flow even if systemic blood pressure does not increase significantly. On the other hand, in pathological conditions such as atherosclerosis, narrowed arteries increase resistance, requiring higher blood pressure to maintain adequate flow. Understanding blood flow and blood pressure dynamics helps explain why managing vascular resistance is a cornerstone of hypertension therapy.
The broader concept of blood pressure and circulation reflects this balance. It is not just about the pressure itself, but how that pressure facilitates or hinders effective blood distribution. This is why clinicians monitor both parameters closely when assessing cardiovascular function.
Clinical Implications and Why High Blood Pressure Matters
High blood pressure, or hypertension, is a major risk factor for cardiovascular disease, stroke, and renal failure. Understanding why high blood pressure matters to your health begins with recognizing its impact on vascular integrity. Chronically elevated blood pressure can damage the endothelium, the delicate lining of blood vessels, initiating a cascade of inflammatory responses and plaque formation.
Over time, this can lead to narrowed or hardened arteries, reducing blood flow to critical organs. This underscores the question: how does blood pressure affect blood flow? The answer is that excessive pressure can paradoxically reduce flow by damaging the very vessels through which blood travels. It also increases the workload on the heart, leading to left ventricular hypertrophy and eventual heart failure.
Preventive strategies often focus on identifying which of the following changes would increase blood pressure—factors like high sodium intake, obesity, stress, and sedentary lifestyle—and mitigating them through lifestyle interventions and medication. Educating patients on the force of blood against arterial walls helps them appreciate the tangible consequences of poor blood pressure control.
Monitoring and Maintaining Healthy Blood Pressure
Regular monitoring is essential for early detection and management of blood pressure abnormalities. As mentioned earlier, blood pressure is usually measured in what blood vessel? The brachial artery is the standard site for clinical measurements, offering a convenient and accurate reflection of systemic pressure.
Lifestyle choices play a substantial role in maintaining optimal blood pressure. Diets low in sodium and rich in potassium, regular aerobic exercise, and weight management all contribute to vascular health. Pharmacological interventions may also be necessary in cases where lifestyle changes are insufficient. These interventions aim to address the underlying contributors to elevated blood pressure, whether that be excessive fluid retention, overactive sympathetic tone, or arterial stiffness.
Education about blood pressure definition anatomy and function should be part of routine healthcare, empowering individuals to take an active role in managing their cardiovascular risk. Recognizing the signs of abnormal blood pressure early can prevent long-term complications and improve quality of life.
Frequently Asked Questions: Blood Pressure and Circulatory Health
What role does altitude play in blood pressure and circulation?
Living at higher altitudes can significantly impact blood pressure and circulation due to lower oxygen levels in the environment. In response to reduced oxygen availability, the body increases red blood cell production and may elevate blood pressure to improve oxygen delivery to tissues. These changes alter the pressure in blood vessels over time, especially in individuals unaccustomed to such conditions. While initially adaptive, prolonged exposure can place additional stress on the cardiovascular system, particularly in those with pre-existing conditions. This example underscores how dynamic blood pressure and blood circulation can be in response to environmental factors.
Can stress alter how blood flows through the vascular system?
Yes, chronic psychological stress can substantially influence blood flow and blood pressure. Stress triggers the sympathetic nervous system, leading to vasoconstriction and elevated cardiac output—both of which increase the force of blood against arterial walls. Over time, this stress-induced rise in cardiovascular system blood pressure can contribute to hypertension and vascular damage. Stress also affects the balance of hormones like cortisol, which can further disrupt normal blood pressure function. Understanding how stress shapes blood flow and pressure helps contextualize its long-term impact on human anatomy blood pressure regulation.
How does pregnancy affect blood pressure in the circulatory system?
During pregnancy, a woman’s circulatory system undergoes profound changes to support fetal development. Blood volume increases significantly, placing extra demand on the heart and altering pressure in the arteries when the heart is at rest. As the body adjusts, blood vessels dilate to accommodate increased volume, which can cause transient dips or spikes in blood pressure. The body carefully controls this transition, but complications like preeclampsia can arise when blood pressure becomes dysregulated. Monitoring blood pressure in circulatory system changes during pregnancy is essential for maternal and fetal health.
Why is nighttime blood pressure monitoring gaining attention?
Recent research shows that blood pressure flow patterns vary throughout the day and night, with healthy individuals typically experiencing a nocturnal dip. When this dip does not occur—known as “non-dipping”—it may signal heightened cardiovascular risk. Monitoring blood pressure in the veins and arteries during sleep offers insights into conditions that daytime readings might miss. Since blood vessels’ blood pressure response can differ under resting conditions, 24-hour monitoring is increasingly seen as vital for detecting early vascular issues. Understanding blood pressure and circulation over a full day reveals hidden patterns linked to stroke or heart attack risk.
Are there gender-based differences in how blood pressure is produced and regulated?
Yes, hormonal differences between men and women lead to variations in how blood pressure is created and managed. Estrogen tends to promote vasodilation and lower blood pressure, while testosterone may contribute to higher vascular resistance. These hormonal effects influence the pressure in blood vessels differently throughout the lifespan, especially during puberty, pregnancy, and menopause. The ways in which blood pressure is usually measured in what blood vessel (typically the brachial artery) are the same for both genders, but interpreting the data may require gender-specific baselines. Understanding these distinctions helps refine treatment strategies for high or low blood pressure in different populations.
What role does posture play in blood pressure regulation?
Postural changes can significantly affect blood pressure and blood flow, especially in older adults or those with autonomic dysfunction. Standing up suddenly can cause a temporary drop in blood pressure, a condition called orthostatic hypotension. This occurs because gravity shifts blood to the lower extremities, reducing the pressure in the capillaries and upper body until compensatory mechanisms engage. These rapid shifts highlight how sensitive the cardiovascular system is to positional changes and how the body controls blood pressure in real time. Postural responses reflect the intricate balance between blood pressure and blood circulation that sustains vital organ function.
How do blood pressure medications target specific vessels in the vascular system?
Modern antihypertensive drugs are designed with precision to influence different segments of the vascular system. For instance, calcium channel blockers relax the smooth muscles in arterial walls, thereby reducing the pressure in blood vessels and improving flow. Diuretics reduce blood volume, lowering both cardiac output and the pressure in the arteries when the heart is at rest. These treatments are tailored based on understanding which type of blood vessel regulates blood pressure most effectively—typically the arterioles. Targeting vessel-specific responses allows for more personalized management of blood pressure in circulatory system disorders.
How are new technologies changing blood pressure monitoring?
Emerging technologies are redefining how we monitor and interpret blood pressure data. Wearable devices now allow for continuous, non-invasive readings, offering deeper insights into blood pressure function across various activities and environments. Some devices even assess the blood pressure in the capillaries through photoplethysmography, enhancing understanding of microcirculatory health. These advancements help identify trends in blood pressure and blood circulation that static office measurements might miss. As these tools evolve, they promise to revolutionize how we define, measure, and manage cardiovascular system blood pressure in real-time settings.
Why do some people develop high blood pressure without symptoms?
Hypertension is often dubbed the “silent killer” because it can persist without noticeable symptoms, yet still exert damaging force on blood vessels. The absence of symptoms does not equate to the absence of risk; chronic high blood pressure affects blood flow and blood pressure dynamics long before organ damage becomes apparent. Subclinical changes such as increased pressure in blood vessels or microvascular inflammation may quietly progress. This is why understanding which of the following changes would increase blood pressure—like excess salt intake or sedentary behavior—is crucial for early prevention. Routine screening helps detect asymptomatic hypertension before it leads to irreversible complications.
What future breakthroughs may change how we treat blood pressure disorders?
The future of blood pressure treatment lies in precision medicine and gene-based therapies. Researchers are investigating genetic markers that influence how blood pressure is produced and maintained, which could lead to targeted interventions based on a person’s unique physiology. Advances in bioengineered tissues may eventually allow us to repair or replace damaged blood vessels whose blood pressure regulation has failed. These innovations aim to enhance how are blood pressure and blood flow related in real-time, offering dynamic, adaptive treatments. As our understanding of blood pressure definition anatomy deepens, treatment approaches will become increasingly customized, effective, and preventive.
Conclusion: The Vital Interplay Between Blood Pressure and Circulatory Health
In summary, the relationship between blood pressure and blood flow is a dynamic and vital aspect of human physiology. From the pressure in blood vessels to the force of blood against arterial walls, every component of the cardiovascular system is involved in regulating circulation. Understanding how blood pressure is created, regulated, and maintained provides critical insights into broader cardiovascular health.
Whether considering the highest pressures found in the aorta or the reduced levels in the veins and capillaries, each region of the vascular system contributes to efficient and balanced blood pressure flow. The fact that blood flows from high to low pressure heart regions is not just a principle—it is a physiological necessity that sustains life. Recognizing how the body controls blood pressure through neural, hormonal, and renal mechanisms adds depth to our understanding of health and disease.
Ultimately, blood pressure and blood circulation are inseparable partners in sustaining life. By integrating an understanding of blood vessels, blood pressure, and hemodynamics into everyday health practices, we empower ourselves to better manage risk factors, improve cardiovascular outcomes, and support long-term well-being. The ongoing study of blood pressure in the circulatory system continues to unlock new insights into both preventive care and clinical interventions for cardiovascular disorders.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.