In the evolving landscape of cancer care, innovation is not a luxury—it is a necessity. As the global burden of cancer continues to rise, clinicians, researchers, and patients alike are looking toward technologies that offer more than incremental change. Among the most promising developments in this quest are targeted radiation therapies and advanced beam treatment options powered by cutting-edge radiation machines for cancer. These technologies represent more than just an evolution in oncologic care; they signal a profound shift in how we understand, deliver, and measure effective cancer treatment.
You may also like: Cancer Research Breakthroughs: How Modern Advancements Are Transforming Treatment
Today’s breakthroughs in targeted radiation and beam therapy are grounded in decades of research but propelled by modern advancements in physics, computing, and molecular biology. This synergy has resulted in machines capable of delivering ultra-precise doses of radiation directly to tumors while sparing healthy tissues to an unprecedented degree. For patients, this means fewer side effects, shorter recovery times, and, most importantly, improved survival outcomes. For healthcare providers, it signifies a transition toward precision oncology—an approach that tailors treatment to the individual characteristics of each patient and their disease.
Understanding the Fundamentals of Radiation Therapy in Oncology
Radiation therapy has long been a cornerstone of cancer treatment, dating back to the discovery of X-rays in the late 19th century. By utilizing high-energy particles or waves, radiation therapy destroys or damages cancer cells, interfering with their ability to reproduce. Traditionally, this method involved exposing the tumor and surrounding areas to a broad field of radiation, a necessary but imprecise approach that often led to unintended harm to adjacent healthy tissues.
The fundamental principle behind all forms of radiation therapy is the induction of DNA damage within cancer cells. Since cancer cells typically divide more rapidly than normal cells and possess impaired mechanisms for repairing DNA, they are particularly vulnerable to this type of damage. However, normal tissues are not immune, and collateral damage has historically been a limiting factor in the effectiveness of radiation therapy. This is where the concept of targeting—both anatomically and biologically—has begun to revolutionize outcomes.
Emergence of Targeted Radiation: A Game-Changer in Oncology
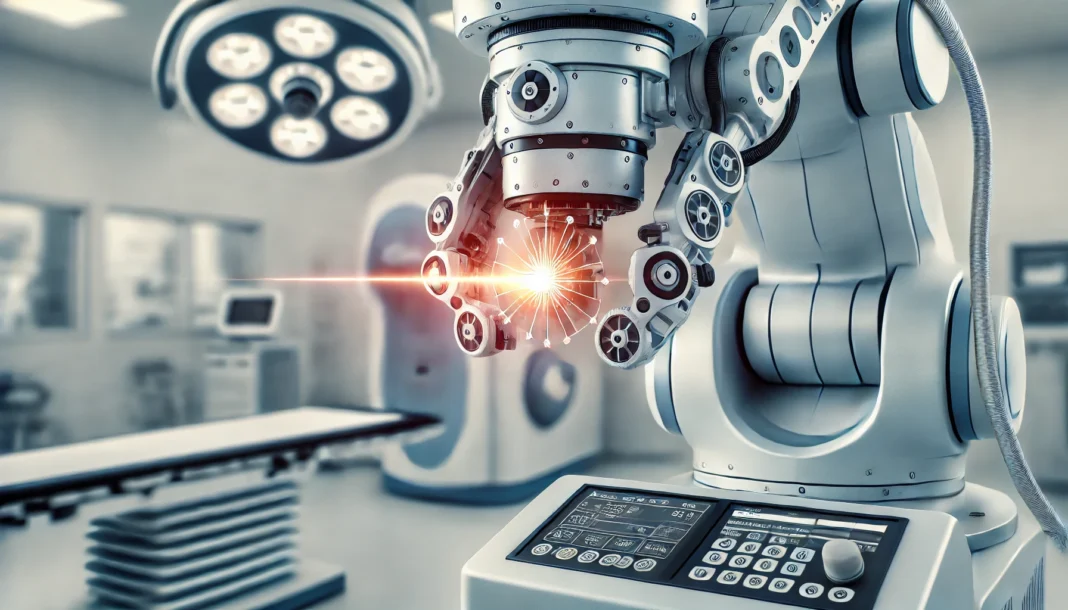
Targeted radiation is not a single technology but rather a suite of techniques that enables oncologists to direct radiation with extreme specificity. Techniques such as intensity-modulated radiation therapy (IMRT), stereotactic body radiation therapy (SBRT), and image-guided radiation therapy (IGRT) fall under this umbrella. These approaches leverage real-time imaging and computerized planning to adjust the shape, intensity, and direction of radiation beams as treatment progresses.
What truly distinguishes targeted radiation is its ability to adapt treatment in real time. Through technologies such as adaptive radiation therapy (ART), clinicians can account for changes in tumor size, shape, or position over the course of treatment. This dynamic adaptation ensures that each session is optimized based on the most current anatomical information. Such precision is particularly vital for tumors located near critical structures, where millimeters can make the difference between curative treatment and unacceptable toxicity.
Beam Therapy and the Rise of Particle-Based Treatments
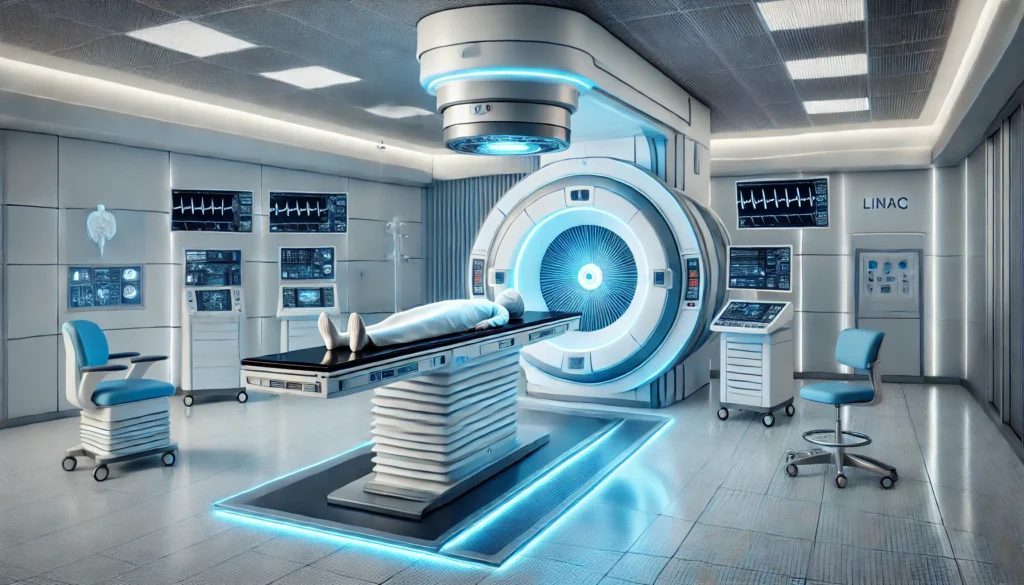
Among the most significant advancements in radiation oncology is the development of beam therapy that employs particles—rather than photons—as the medium of energy transfer. Proton therapy and carbon ion therapy are the most well-known forms of particle beam therapy. Unlike conventional X-rays, which deposit energy along their entire path through the body, proton beams release the majority of their energy at a specific point known as the Bragg peak. This unique property allows for maximum tumor destruction with minimal exposure to surrounding healthy tissues.
Proton beam therapy has gained traction for pediatric cancers, brain tumors, and other malignancies where long-term side effects from radiation are a major concern. For example, in treating medulloblastoma, a common pediatric brain cancer, proton therapy reduces radiation exposure to the developing brain and spinal cord, potentially preserving cognitive function. Carbon ion therapy, although less widely available, offers even greater biological effectiveness and may be useful for radioresistant tumors that do not respond well to conventional radiation.
Clinical Evidence and Patient Outcomes: What the Data Shows
As with any medical innovation, the promise of targeted radiation and beam therapy must be substantiated by clinical evidence. Fortunately, a growing body of research supports the efficacy and safety of these technologies. Numerous randomized controlled trials and observational studies have shown improved local control rates and reduced toxicity for a variety of cancers, including prostate, lung, breast, and head and neck malignancies.
Importantly, these improved outcomes are not confined to survival metrics alone. Quality-of-life assessments have revealed that patients undergoing targeted radiation or beam treatment report less fatigue, fewer gastrointestinal disturbances, and quicker return to daily activities. This holistic benefit is especially relevant in the context of survivorship, where long-term function and well-being are just as critical as disease eradication.
Expanding Access and Overcoming Barriers to Adoption
Despite the promise of targeted radiation and beam therapy, access remains uneven. High costs associated with installing and maintaining advanced radiation machines for cancer, including particle therapy systems, can limit availability to only well-funded institutions. Insurance reimbursement policies also vary widely, which can create disparities in who receives these treatments.
Efforts are underway to make these therapies more accessible. Some countries have launched public-private partnerships to fund the development of proton centers, while others are encouraging regional collaboration to share resources across institutions. Furthermore, cost-effectiveness analyses are increasingly showing that although initial expenditures are high, the reduction in long-term side effects, hospitalizations, and lost productivity makes beam treatment a worthwhile investment for many health systems.

Looking Ahead: The Next Frontier in Radiation Oncology
The future of radiation oncology lies at the intersection of technology, biology, and patient-centered care. Researchers are exploring the integration of immunotherapy with beam therapy, leveraging radiation’s ability to release tumor antigens and enhance immune responses. Clinical trials are testing combinations of proton therapy with immune checkpoint inhibitors, aiming to improve outcomes in cancers like melanoma and non-small cell lung cancer.
Newer modalities, such as FLASH radiation therapy—which delivers ultra-high doses in a fraction of a second—are under active investigation. Early studies suggest that FLASH may spare normal tissues even more effectively than conventional techniques, potentially revolutionizing how beam treatment is delivered. Similarly, portable radiation devices may expand access to care in underserved areas and during emergencies.
Frequently Asked Questions (FAQ): Targeted Radiation, Beam Therapy, and the Latest Cancer Treatment Technologies
1. How is patient mental health affected during and after beam therapy treatments?
While much attention is given to the physical side effects of cancer therapy, the emotional and psychological dimensions of beam therapy also warrant deep consideration. Many patients undergoing beam treatment experience a mixture of hope and anxiety—hope from using cutting-edge therapies, but anxiety due to the unfamiliar nature of a proton or carbon ion radiation machine for cancer. In some cases, the intense focus on precision and machinery can make the treatment feel impersonal, which underscores the importance of psychosocial support throughout the process. Clinical settings that integrate psychological counseling alongside targeted radiation care tend to see better long-term mental health outcomes. For patients, being informed about the beam therapy process in detail and having open channels of communication with their care team can help alleviate fear and improve emotional resilience.
2. Are there emerging applications of beam therapy beyond traditional cancer types?
Yes, beam therapy is increasingly being studied for rare and difficult-to-treat tumors, such as chordomas at the skull base or certain sarcomas that resist conventional treatment. Researchers are now exploring its potential in cases where conventional therapy has failed, including recurrent cancers and previously irradiated areas. These efforts are made possible by the high conformality and sparing nature of targeted radiation, which allows for precise retreatment. Additionally, some clinical trials are investigating how beam treatment could benefit benign but problematic tumors like acoustic neuromas or arteriovenous malformations. As technology evolves, the capabilities of every advanced radiation machine for cancer treatment are expected to expand, broadening the scope of beam therapy’s clinical utility.
3. Can patients continue working or performing normal activities during beam treatment?
In many cases, yes. One of the key advantages of modern beam treatment methods—especially targeted radiation—is the reduced side effect profile compared to older approaches. Because beam therapy can spare healthy tissue more effectively, patients often report fewer instances of fatigue, nausea, or skin irritation. This allows many to maintain a regular work schedule or daily routines, although temporary adjustments may be necessary based on tumor location and individual tolerance. It’s important for patients to coordinate with their oncologists to develop a supportive plan, especially if the treatment site affects mobility or energy levels.
4. What are the logistical challenges of accessing a radiation machine for cancer treatment using beam therapy?
Accessibility remains a significant challenge, particularly in rural or underserved areas. Facilities housing a beam therapy-capable radiation machine for cancer treatment are highly specialized and require substantial investment in both infrastructure and trained personnel. As a result, patients may need to travel long distances or even relocate temporarily to access beam treatment. The time commitment can include daily visits over several weeks, depending on the treatment plan. Fortunately, some health systems are implementing remote housing programs and partnerships with regional hospitals to ease this burden. As demand increases, it’s likely that more compact and cost-effective proton and carbon ion systems will emerge, making targeted radiation more widely accessible.
5. How do patients’ individual biology and tumor genetics influence beam therapy planning?
One of the most promising frontiers in beam therapy is the integration of molecular diagnostics into treatment planning. The growing use of genomics allows oncologists to predict how a tumor might respond to targeted radiation based on its biological profile. Certain genetic mutations, for example, may confer resistance to conventional radiation but still be susceptible to high-LET (Linear Energy Transfer) particles like carbon ions. Advanced imaging and radiomics further enhance this precision, allowing treatment with a radiation machine for cancer to be shaped not just around anatomical structures, but around biologically active regions. Personalized beam treatment protocols rooted in genomic data are being actively studied and could redefine individualized cancer care.
6. What are the environmental and operational considerations of installing beam therapy systems?
Beyond clinical factors, installing a radiation machine for cancer that supports beam therapy involves unique environmental and operational planning. Proton and carbon ion accelerators require substantial space, often needing purpose-built facilities with advanced shielding and cooling systems. These units also demand a highly trained support team, including physicists, engineers, and radiation safety officers. Energy consumption is another consideration, although newer models are being designed with sustainability in mind. Forward-thinking cancer centers are now factoring environmental impact into their purchasing decisions, seeking systems that deliver effective beam treatment while reducing their carbon footprint.
7. What role does artificial intelligence play in modern targeted radiation treatments?
Artificial intelligence (AI) is increasingly central to optimizing targeted radiation plans. AI algorithms analyze thousands of data points from imaging scans, previous outcomes, and tumor characteristics to suggest ideal beam configurations. This enhances the safety and speed of treatment planning, allowing beam therapy to be deployed more rapidly without compromising quality. AI also supports adaptive therapy by learning from how a patient’s tumor responds during the course of treatment, enabling real-time modifications. While AI cannot replace human clinical judgment, it acts as a powerful partner in ensuring that each session with a radiation machine for cancer delivers the most effective dose to the intended target.
8. How do socioeconomic disparities impact access to targeted radiation and beam treatment?
Socioeconomic status can significantly influence access to advanced cancer therapies. Patients from lower-income backgrounds may face greater difficulty accessing beam therapy due to travel costs, time off work, and gaps in insurance coverage. While some public systems and philanthropic programs are working to bridge this divide, disparities remain. Radiation machines for cancer treatment that incorporate beam therapy are often located in major metropolitan centers, making geographic location a factor as well. Policymakers and healthcare advocates are calling for reimbursement reforms and expanded investment in regional cancer hubs to make targeted radiation more equitable.
9. Are there any long-term monitoring needs after undergoing beam therapy?
Yes, patients who complete beam treatment often require lifelong follow-up tailored to the type and location of the cancer treated. While targeted radiation typically results in fewer acute side effects, there may be delayed complications such as fibrosis, hormonal changes, or secondary cancers—particularly in pediatric patients. Regular imaging and lab tests help monitor for recurrence or late-emerging issues. Newer data-driven monitoring tools are being developed to assess risk based on real-time patient feedback and long-term biomarker analysis. These advances ensure that the benefits of using a precision radiation machine for cancer don’t end when treatment does—they extend into vigilant survivorship care.
10. What future innovations could enhance beam therapy in the next decade?
The future of beam therapy is likely to be shaped by miniaturization, speed, and integration. Researchers are developing compact radiation machines for cancer care that can deliver beam treatment without the need for massive infrastructure. FLASH therapy, a new technique that delivers ultra-high dose rates in milliseconds, is being explored for its potential to spare healthy tissue even more effectively than current methods. Integrating immunotherapy with targeted radiation is another exciting frontier, potentially turning local treatment into a systemic anti-cancer response. Finally, virtual reality and patient-centered software are being introduced to improve the treatment experience, making beam therapy not only more effective, but also more humane and patient-friendly.

Conclusion: Shaping the Future of Oncology with Targeted Radiation and Beam Therapy
As we stand on the precipice of a new era in cancer care, the transformative power of targeted radiation and advanced beam therapy is impossible to ignore. These modalities, backed by cutting-edge radiation machines for cancer, have fundamentally redefined how clinicians approach the delicate balance between eradicating malignancies and preserving healthy function. Through improved targeting, real-time imaging, and the biological precision of beam treatment technologies like proton and carbon ion therapy, we are now able to offer patients more effective care with fewer adverse effects.
Ultimately, the integration of targeted radiation and beam therapy into modern oncology is not merely about advancing technology—it is about transforming lives. These innovations speak to the core mission of medicine: to heal with precision, compassion, and vision. As research, engineering, and clinical expertise continue to converge, we are not only improving cancer treatment—we are redefining what is possible in the fight against cancer.
precision cancer treatment, radiotherapy innovations, next-generation oncology, cancer imaging technology, advanced radiology systems, high-precision tumor targeting, stereotactic radiotherapy advances, proton radiation therapy benefits, cancer care technology trends, adaptive radiotherapy planning, personalized oncology solutions, cutting-edge oncology devices, radiation oncology breakthroughs, modern cancer treatment techniques, image-guided therapy systems, non-invasive cancer therapy, oncology treatment optimization, survivorship in radiation oncology, future of cancer therapy, radiation treatment planning tools
Further Reading:
How Radiation Therapy Is Used to Treat Cancer
External Beam Radiation Therapy for Cancer
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.