Introduction: Understanding Arterial Plaque and the Need for Safe Removal
Cardiovascular health is a fundamental aspect of overall well-being, with arterial blockages posing significant risks to individuals worldwide. Plaque accumulation within arteries, known as atherosclerosis, can lead to serious complications, including heart attacks and strokes. The safe and effective removal of plaque is critical for restoring proper blood flow and preventing life-threatening cardiovascular events. Among the various treatment options available, the atherectomy procedure has emerged as an advanced and minimally invasive technique for heart plaque removal. This article explores the role of the atherectomy procedure in facilitating the removal of plaque from the inner lining of an artery, emphasizing its safety, efficacy, and benefits over traditional interventions.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
The Mechanism of Arterial Plaque Formation and Its Health Implications
Arterial plaque develops due to the accumulation of fatty deposits, cholesterol, calcium, and other substances within the blood vessels. Over time, these deposits harden and narrow the arteries, restricting blood flow and increasing the risk of cardiovascular disease. This process, known as atherosclerosis, can result from various factors, including high cholesterol, hypertension, smoking, diabetes, and a sedentary lifestyle.
The implications of plaque buildup are severe, often leading to conditions such as coronary artery disease (CAD), peripheral artery disease (PAD), and cerebrovascular disease. As arteries become increasingly obstructed, oxygen-rich blood struggles to reach vital organs, leading to symptoms such as chest pain (angina), leg pain, fatigue, and, in severe cases, myocardial infarctions or strokes. Given these risks, effective vascular plaque removal methods are essential for preserving cardiovascular function and overall health.
The Role of Atherectomy in Cardiac Plaque Removal
The atherectomy procedure represents a highly specialized approach to treating arterial blockages. Unlike traditional methods such as angioplasty and stenting, which primarily focus on widening narrowed arteries, atherectomy directly targets and removes plaque, reducing the burden of arterial obstruction. This procedure is particularly beneficial for patients with calcified or fibrotic plaques that are resistant to conventional treatments.
Atherectomy is performed using a catheter-based device equipped with a rotating blade, laser, or orbital mechanism that shaves, vaporizes, or grinds away plaque deposits. This precise and controlled removal process enhances blood flow while minimizing damage to the arterial wall. The procedure is often used in conjunction with balloon angioplasty or stenting to optimize treatment outcomes, ensuring that arteries remain open and functional following plaque removal.
Types of Atherectomy Procedures and Their Applications
Several variations of the atherectomy procedure exist, each tailored to address specific types of arterial plaque and anatomical challenges. The four primary types include:
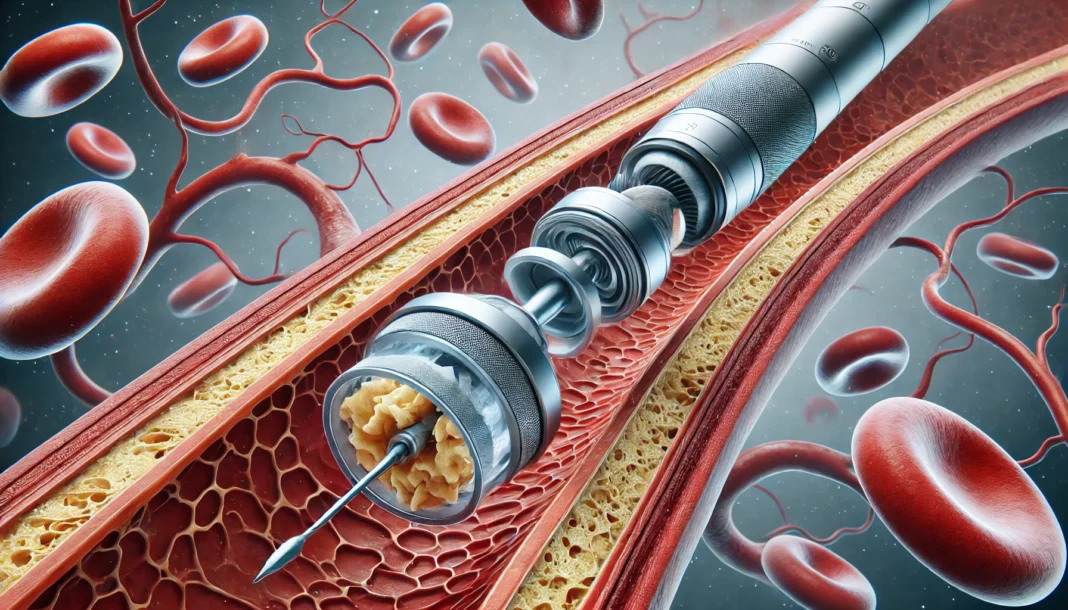
1. Directional Atherectomy
Directional atherectomy involves a catheter with a rotating blade that cuts away plaque and collects the debris for removal. This technique is particularly effective in treating non-calcified plaques in the coronary and peripheral arteries. By selectively excising plaque from targeted areas, directional atherectomy helps preserve arterial integrity while restoring optimal blood flow.
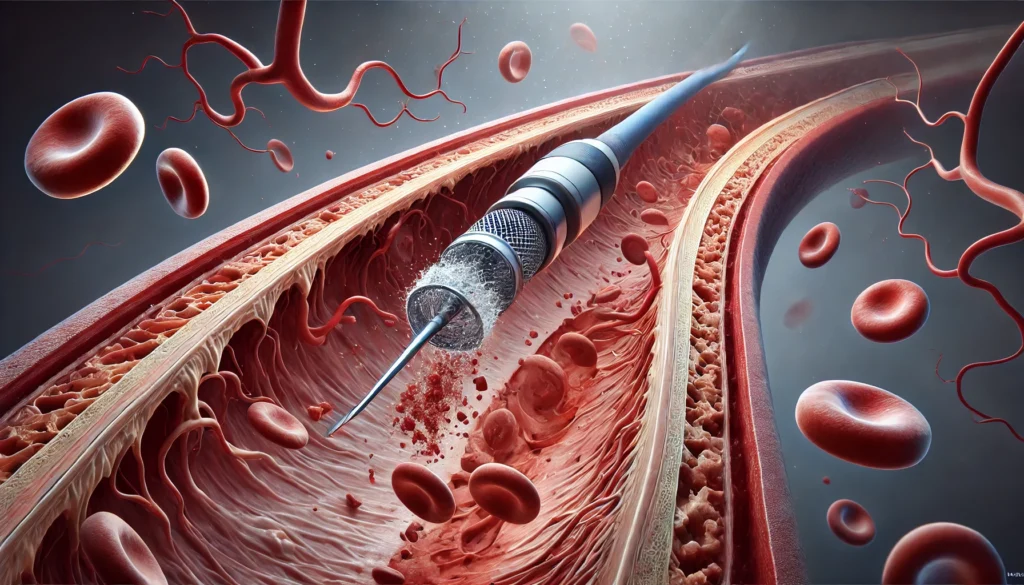
2. Rotational Atherectomy
Rotational atherectomy utilizes a high-speed, diamond-tipped burr to pulverize hardened, calcified plaque into microscopic particles that are naturally excreted by the body. This approach is especially useful in cases where standard angioplasty balloons are unable to adequately dilate rigid blockages. Rotational atherectomy is commonly employed in coronary interventions to facilitate successful stent placement.
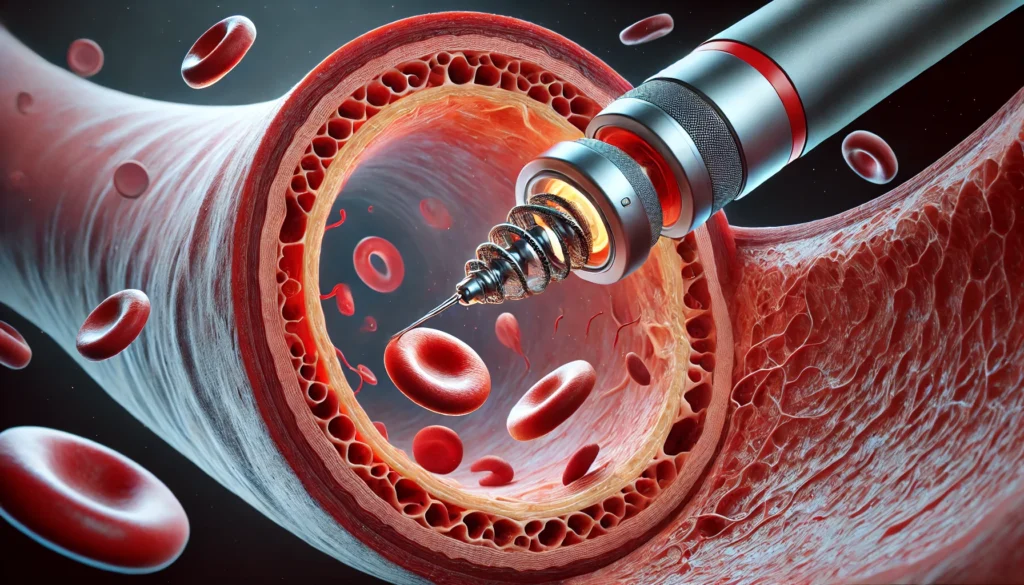
3. Orbital Atherectomy
Orbital atherectomy employs an eccentrically rotating crown that sands down plaque while preserving the arterial wall. The device’s oscillatory motion ensures uniform plaque modification, making it a preferred choice for complex, heavily calcified lesions. This technique is particularly beneficial for patients with advanced peripheral artery disease who require extensive vascular plaque removal.
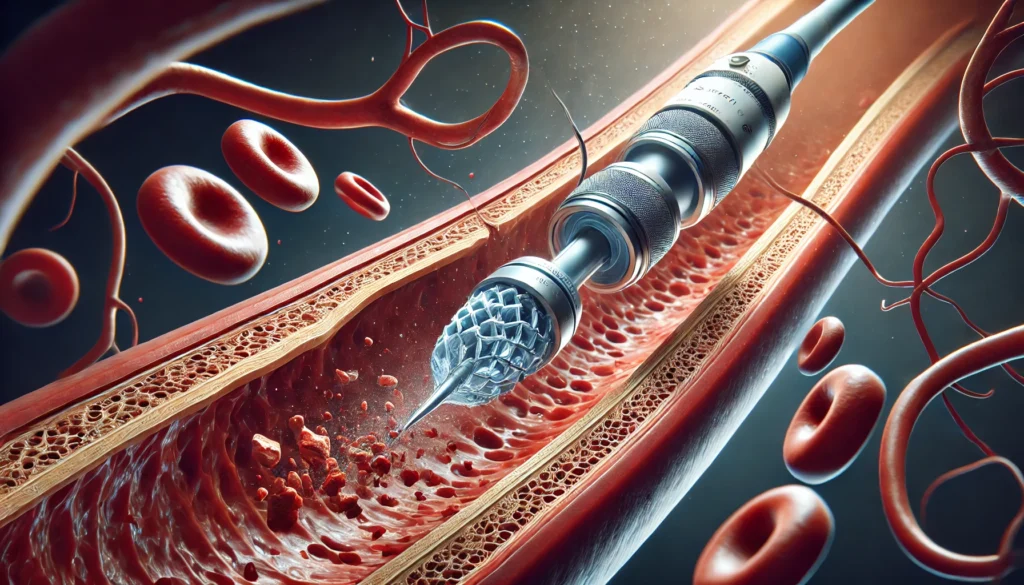
4. Laser Atherectomy
Laser atherectomy uses high-energy laser beams to vaporize plaque deposits, reducing their volume and restoring arterial patency. This method is often employed in cases involving soft, fibrotic, or thrombotic plaques that respond well to thermal energy. Laser atherectomy is a versatile option for both coronary and peripheral applications, offering a minimally invasive alternative to surgical interventions.
Benefits of Atherectomy Over Traditional Plaque Removal Methods
The atherectomy procedure offers several advantages over conventional treatments, making it a preferred choice for many patients with arterial disease. These benefits include:
- Minimally Invasive Nature: Atherectomy is performed via a catheter inserted through a small incision, reducing the need for open surgery and minimizing recovery time.
- Targeted Plaque Removal: Unlike angioplasty, which compresses plaque against the artery walls, atherectomy physically removes the obstruction, decreasing the likelihood of restenosis (re-narrowing of the artery).
- Enhanced Efficacy for Calcified Lesions: Many traditional interventions struggle to effectively treat heavily calcified plaques. Atherectomy excels in modifying and eliminating rigid blockages, improving procedural success rates.
- Improved Long-Term Outcomes: By directly addressing the root cause of arterial obstruction, atherectomy contributes to sustained improvements in blood flow and cardiovascular health.
Potential Risks and Considerations in Atherectomy Procedures
While atherectomy is a highly effective intervention, it is not without risks. Potential complications include arterial perforation, embolization (plaque debris breaking off and traveling to other areas), and vessel dissection. To mitigate these risks, physicians carefully evaluate patient eligibility, selecting candidates based on factors such as plaque composition, vessel anatomy, and overall cardiovascular health.
Post-Procedure Care and Long-Term Cardiovascular Management
Following an atherectomy procedure, patients must adhere to a comprehensive cardiovascular care plan to prevent future plaque accumulation. Lifestyle modifications, including a heart-healthy diet, regular exercise, smoking cessation, and cholesterol management, play a crucial role in maintaining arterial health. Additionally, medications such as antiplatelet agents, statins, and blood pressure regulators may be prescribed to reduce the risk of recurrent blockages.
Frequently Asked Questions (FAQ) on the Atherectomy Procedure and Plaque Removal
1. What makes the atherectomy procedure different from other methods of heart plaque removal?
The atherectomy procedure distinguishes itself from traditional interventions by directly excising and eliminating plaque rather than simply compressing it against arterial walls. Unlike angioplasty, which uses a balloon to push plaque aside, atherectomy physically removes obstructions, reducing the risk of re-narrowing. Additionally, this procedure is particularly beneficial for patients with heavily calcified plaques that do not respond well to standard balloon angioplasty. The various atherectomy techniques, such as rotational, orbital, and laser atherectomy, offer customized approaches to different types of arterial blockages, ensuring optimal results. By integrating advanced plaque removal strategies, the atherectomy procedure enhances long-term vascular health outcomes while minimizing complications associated with plaque fragmentation.
2. How does the removal of plaque from the inner lining of an artery impact long-term cardiovascular health?
The removal of plaque from the inner lining of an artery significantly improves long-term cardiovascular health by restoring proper blood flow and reducing the likelihood of major cardiovascular events such as heart attacks and strokes. When plaque obstructs arteries, oxygen and nutrient delivery to vital organs is compromised, leading to tissue damage over time. By using an atherectomy procedure to remove these obstructions, patients experience improved circulation, reduced symptoms such as chest pain or leg cramps, and enhanced overall quality of life. Furthermore, effective plaque removal lowers systemic inflammation, which plays a crucial role in the progression of cardiovascular disease. This targeted intervention helps break the cycle of plaque buildup, especially when paired with lifestyle modifications and medication management.
3. Who is an ideal candidate for vascular plaque removal through atherectomy?
An ideal candidate for vascular plaque removal via atherectomy is someone who has developed significant arterial blockages that do not respond well to conventional treatments. Patients with calcified or fibrotic plaque formations, which are difficult to manage with angioplasty alone, often benefit most from this procedure. Additionally, individuals who have undergone previous stent placements but continue to experience arterial narrowing may be good candidates for atherectomy. Those with peripheral artery disease (PAD) or coronary artery disease (CAD) who exhibit symptoms like leg pain, difficulty walking, or persistent angina are also considered for this intervention. A comprehensive cardiovascular evaluation, including imaging studies and risk assessments, helps determine the suitability of an atherectomy procedure for a given patient.
4. How does cardiac plaque removal through atherectomy improve blood flow efficiency?
Cardiac plaque removal via atherectomy enhances blood flow efficiency by directly eliminating the physical barriers that restrict circulation. Unlike other treatments that may leave residual plaque in place, atherectomy physically extracts or modifies the plaque, allowing for smoother and more consistent blood movement through the arteries. This increased efficiency helps reduce strain on the heart, lowering blood pressure and improving oxygen delivery to tissues. Over time, the reduction of arterial blockages decreases the risk of clot formation, which can lead to heart attacks or strokes. As a result, patients often experience increased energy levels, improved exercise tolerance, and reduced symptoms of cardiovascular distress following an atherectomy procedure.
5. What risks are associated with an atherectomy procedure for heart plaque removal?
Like any medical intervention, the atherectomy procedure carries some risks, though they are generally low when performed by experienced specialists. Potential complications include arterial perforation, where the catheter may unintentionally damage the artery wall, leading to bleeding or vessel rupture. Another concern is embolization, where dislodged plaque fragments travel to smaller blood vessels, potentially causing blockages elsewhere. There is also a minor risk of restenosis, where the artery narrows again after the procedure, though this risk is mitigated when atherectomy is combined with stent placement or medication therapy. Patients should discuss these risks with their healthcare provider to determine the best approach for their specific condition.
6. What role does lifestyle modification play in maintaining results after vascular plaque removal?
Lifestyle modifications play a critical role in sustaining the benefits of vascular plaque removal after an atherectomy procedure. While the intervention effectively eliminates existing blockages, it does not prevent new plaque formation. Therefore, adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins is essential in reducing cholesterol buildup. Regular physical activity improves circulation and strengthens the cardiovascular system, further preventing arterial disease progression. Smoking cessation is another crucial factor, as tobacco use accelerates plaque accumulation and damages blood vessels. Long-term success also depends on medication adherence, particularly for those prescribed cholesterol-lowering statins or blood pressure medications to keep arteries open and functional.
7. How does atherectomy compare to bypass surgery for cardiac plaque removal?
Atherectomy and bypass surgery are both effective methods for cardiac plaque removal, but they differ significantly in their approach, recovery time, and risk profile. Atherectomy is a minimally invasive catheter-based procedure that removes plaque through a small incision, making it a less traumatic option compared to open-heart bypass surgery. Bypass surgery, on the other hand, requires the creation of new pathways for blood flow by grafting healthy blood vessels around blocked arteries. While bypass surgery is often recommended for patients with severe, multi-vessel disease, atherectomy is preferable for those with localized or heavily calcified plaques that require precise removal. Recovery from atherectomy is much quicker, allowing patients to return to normal activities sooner, whereas bypass surgery involves a more extended healing process.
8. Can an atherectomy procedure be repeated if plaque builds up again?
Yes, an atherectomy procedure can be repeated if plaque builds up again, though the goal is to minimize the need for recurrent interventions through effective long-term cardiovascular management. Some patients may experience restenosis, particularly if they have aggressive atherosclerosis or underlying risk factors such as diabetes or high cholesterol. In such cases, follow-up imaging and cardiovascular evaluations help determine whether another atherectomy is necessary. Additionally, advances in atherectomy technology, including drug-coated devices and improved catheter designs, continue to enhance long-term outcomes and reduce the likelihood of repeat procedures. For most patients, combining atherectomy with lifestyle modifications and medical therapies significantly lowers the need for future interventions.
9. How does the atherectomy procedure benefit patients with peripheral artery disease (PAD)?
Patients with peripheral artery disease (PAD) benefit immensely from the atherectomy procedure because it effectively restores blood flow to the lower extremities, reducing symptoms such as pain, numbness, and difficulty walking. PAD occurs when plaque accumulates in the leg arteries, leading to restricted circulation and, in severe cases, non-healing ulcers or gangrene. Atherectomy is particularly useful for removing hard, calcified plaques in leg arteries, where traditional balloon angioplasty may be less effective. By eliminating these blockages, atherectomy reduces the risk of amputation and significantly improves patients’ mobility and quality of life. This procedure is often combined with angioplasty and stent placement to ensure optimal blood flow and long-term vascular health.
10. What future advancements are expected in the field of vascular plaque removal?
The field of vascular plaque removal continues to evolve, with ongoing research and technological innovations aimed at improving the effectiveness and safety of the atherectomy procedure. One promising advancement is the development of bioresorbable scaffolds, which provide temporary structural support to arteries before dissolving naturally, reducing long-term complications. Additionally, drug-coated atherectomy devices are being explored to prevent plaque regrowth by delivering localized anti-inflammatory or cholesterol-lowering medication directly to treated arteries. Artificial intelligence and robotics are also playing a growing role in refining procedural accuracy, reducing the risk of complications, and enhancing real-time decision-making for interventional cardiologists. As these innovations progress, patients can expect even safer and more effective options for managing arterial disease in the coming years.
Conclusion: The Future of Atherectomy in Cardiovascular Medicine
Atherectomy represents a significant advancement in the treatment of arterial plaque buildup, offering a safe and effective method for heart plaque removal. As technology continues to evolve, ongoing innovations in atherectomy devices and techniques will further enhance the precision and success of these procedures. By combining atherectomy with comprehensive cardiovascular management strategies, patients can achieve long-term improvements in vascular health, reducing their risk of severe cardiovascular events. As research and clinical experience expand, the role of atherectomy in cardiac and vascular care will continue to grow, solidifying its place as a cornerstone of modern interventional cardiology.
arterial disease treatment, endovascular procedures, blood flow restoration, cardiovascular intervention, peripheral artery treatment, coronary artery health, minimally invasive cardiology, artery blockage solutions, advanced catheter techniques, interventional cardiology advancements, vascular health improvement, cholesterol plaque removal, circulation enhancement, heart disease prevention, arterial blockage removal, plaque buildup reduction, atherosclerosis management, calcified plaque treatment, medical device innovations, cardiovascular surgery alternatives
Further Reading:
Atherectomy: Types, procedure, and effectiveness
Current Status of Rotational Atherectomy
Statement on the Importance of Atherectomy as a Safe and Effective Treatment Option for Patients
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.