Understanding how the body digests food and transforms it into glucose is fundamental not just to nutrition science but to our daily decisions about what we eat and how we live. While eating may seem like a simple act, digestion is an intricate biological process involving a highly coordinated effort between multiple organs, enzymes, and hormones. This process ensures that carbohydrates, fats, and proteins are broken down efficiently, with glucose serving as a primary fuel source for the body. Through a deeper look into the digestion of carbohydrates and the organs that rely on glucose, we uncover not only how this system functions, but also how nutrition supports overall wellness and disease prevention. For those seeking a medically accurate and SEO-optimized explanation, this article serves as a comprehensive and evidence-based exploration of the digestion process, complete with a detailed diagram of how food is digested with glucose.
You may also like: Macronutrients vs Micronutrients: What the Simple Definition of Macronutrients Reveals About Your Diet and Health
The Digestive Journey Begins: From the Mouth to the Stomach
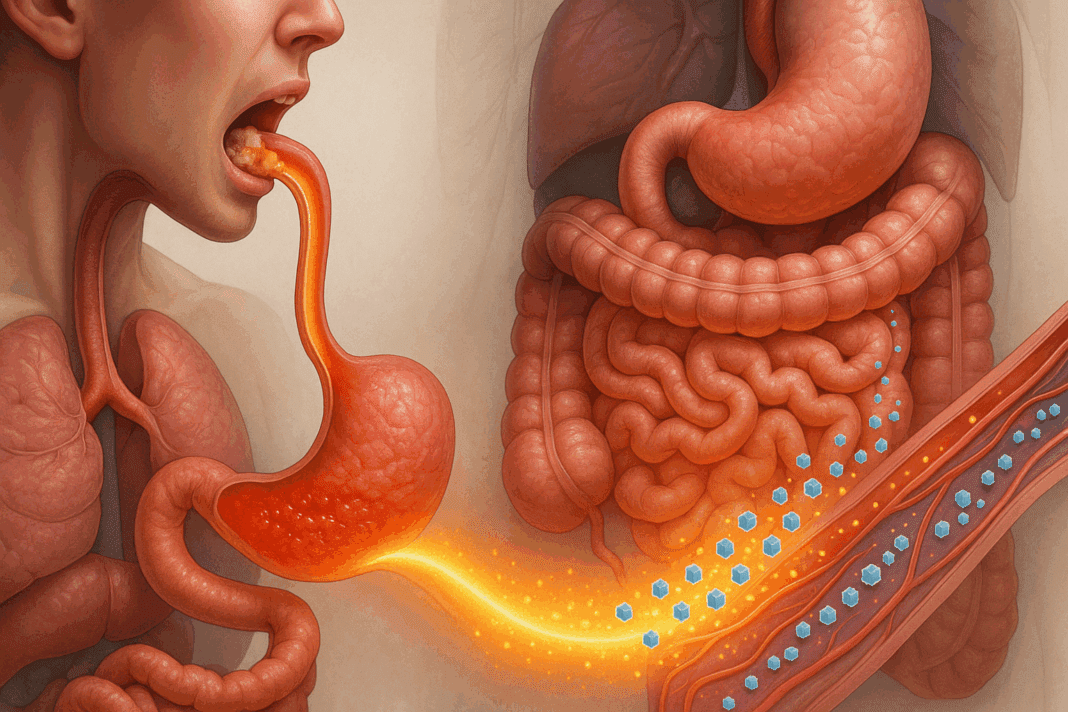
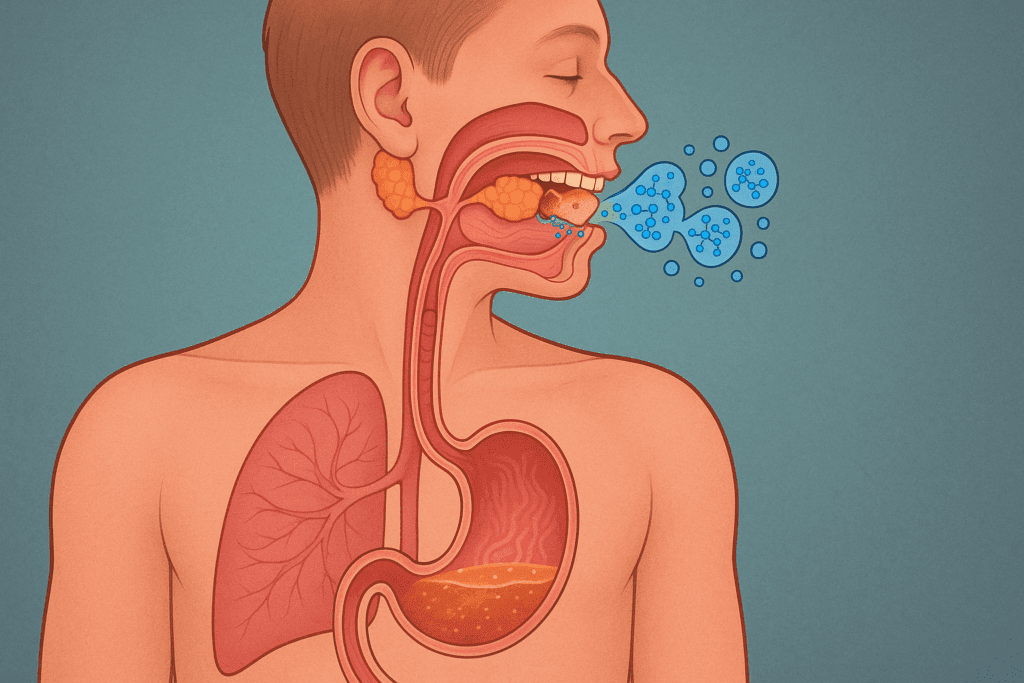
Digestion commences in the mouth, where mechanical breakdown by chewing combines with chemical digestion initiated by enzymes in saliva. Amylase, an enzyme secreted by the salivary glands, begins the process of breaking down complex carbohydrates into simpler sugars. This early stage is crucial, as it sets the tone for downstream enzymatic activity. Contrary to popular belief, digestion doesn’t begin in the stomach but rather in the oral cavity, where food is mechanically processed and mixed with enzymes. This first encounter between food and enzymes is especially relevant when discussing carbohydrates, as these macronutrients require specific conditions for optimal breakdown.
As food travels down the esophagus and enters the stomach, it encounters a highly acidic environment. While the stomach is primarily responsible for breaking down proteins with the help of hydrochloric acid and pepsin, carbohydrates continue to undergo enzymatic processing, albeit at a slower rate. The acidic nature of the stomach temporarily halts amylase activity, but this is a transitional phase before digestion resumes with full force in the small intestine. Despite its limited role in carbohydrate digestion, the stomach plays an indispensable part in mixing food into chyme, the semi-liquid form that will eventually pass into the intestines for further processing. This progression is an essential prelude to the intricate mechanisms that occur in the small intestine, where the majority of nutrient absorption takes place.

The Role of the Small Intestine: Digestion Meets Absorption
The small intestine is often described as the workhorse of the digestive system, and for good reason. Here, the pancreas secretes digestive enzymes like pancreatic amylase, which continues the breakdown of starches into maltose and eventually glucose. Meanwhile, the liver produces bile, which emulsifies fats but also supports the function of digestive enzymes by creating an optimal pH environment. Within the small intestine, particularly in the duodenum and jejunum, the breakdown of carbohydrates reaches completion. Enzymes such as maltase, sucrase, and lactase work at the brush border of the intestinal lining to convert disaccharides into monosaccharides, including glucose, fructose, and galactose.
At this point, the diagram of how food is digested with glucose becomes particularly relevant. Glucose molecules are absorbed through the lining of the small intestine and enter the bloodstream via the hepatic portal vein. This critical pathway allows nutrients to be filtered by the liver before reaching the rest of the body. The efficient absorption and transport of glucose ensure that the body receives a steady supply of energy, particularly for organs that are highly dependent on it. This stage of digestion marks the functional intersection of digestion and metabolism, highlighting the indispensable role of the small intestine in both nutrient acquisition and distribution.
How Glucose Fuels the Body: Circulation and Cellular Uptake
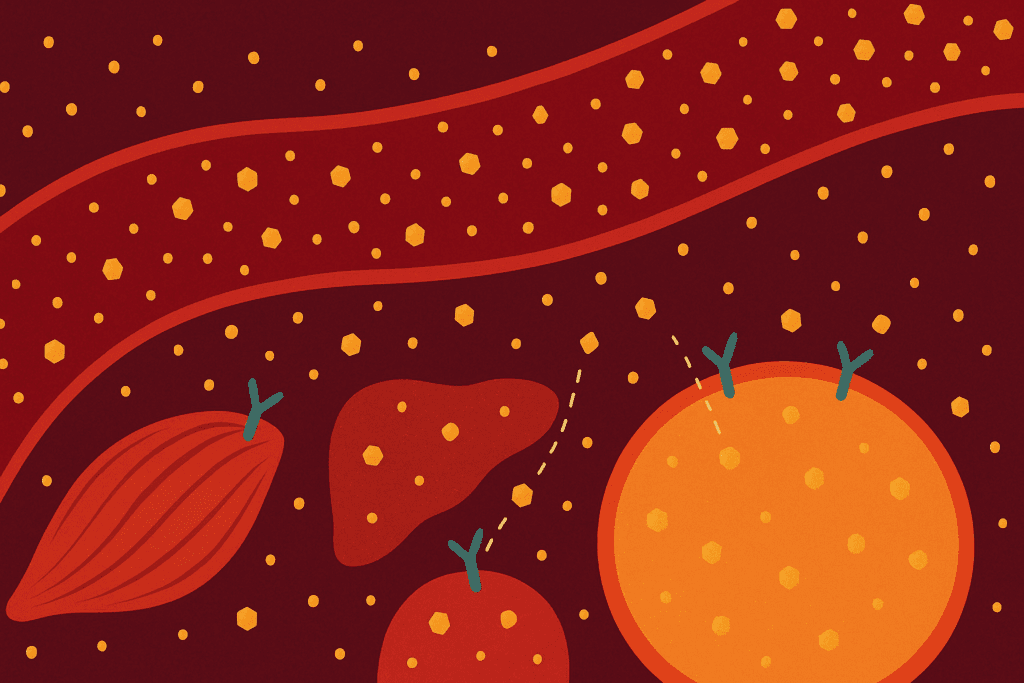
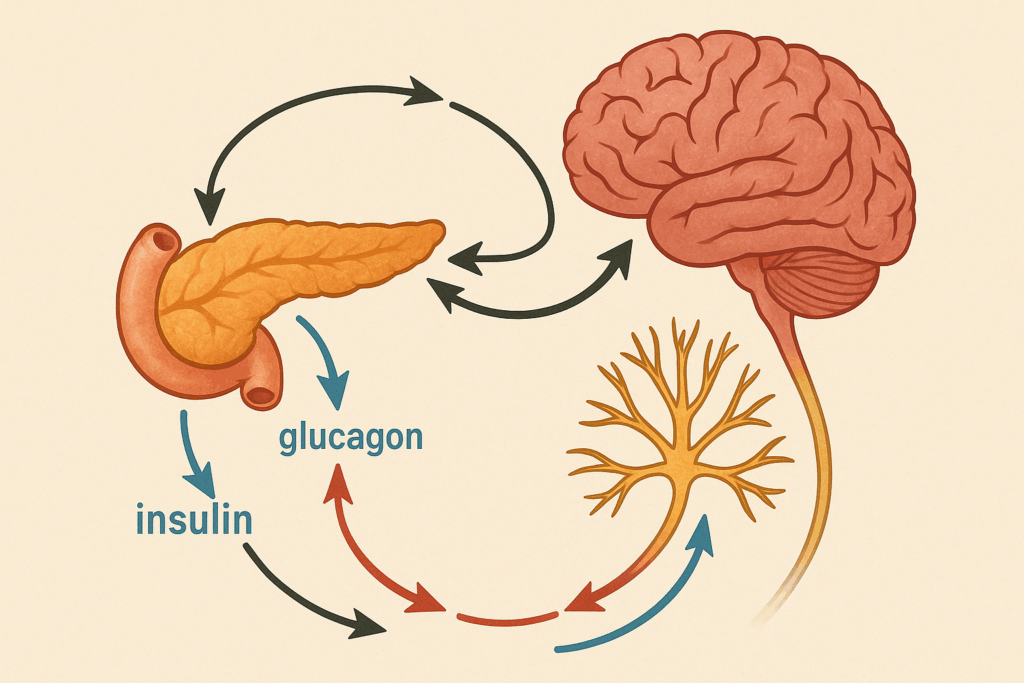
Once glucose enters the bloodstream, it becomes accessible to all cells of the body, but not all tissues utilize it equally. The hormone insulin, produced by the pancreas, plays a pivotal role in regulating glucose uptake. Insulin facilitates the entry of glucose into cells, especially in muscle, liver, and adipose tissue. Without adequate insulin signaling, as observed in diabetes mellitus, glucose remains in the bloodstream, leading to hyperglycemia and associated health risks. The presence of insulin not only lowers blood glucose levels but also ensures that cells have the energy required for metabolic activities.
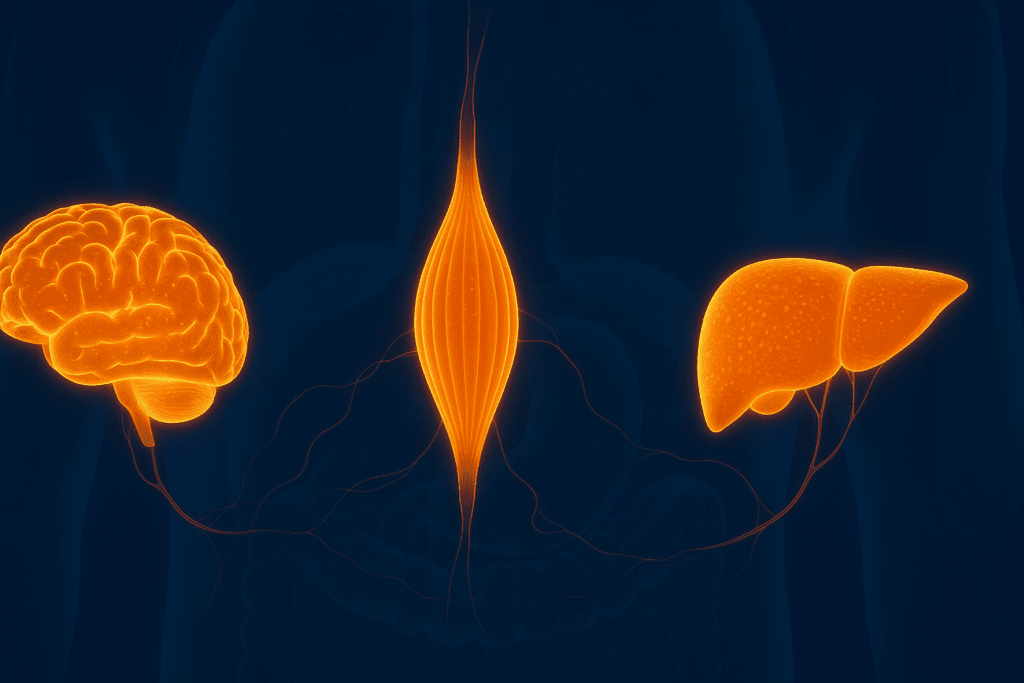
One of the most essential aspects of understanding which organs do carbohydrates help with lies in glucose’s targeted distribution. The brain, for instance, is one of the most glucose-dependent organs, consuming nearly 120 grams of glucose per day. Unlike other tissues, the brain cannot store glucose and relies on a constant supply from the bloodstream. Skeletal muscles, particularly during exercise, also require large amounts of glucose, although they can store it in the form of glycogen. The liver similarly stores glucose as glycogen and plays a critical role in maintaining blood glucose levels between meals through a process known as glycogenolysis. These examples underscore how glucose serves as a universal energy currency, with specific organs demonstrating heightened reliance.
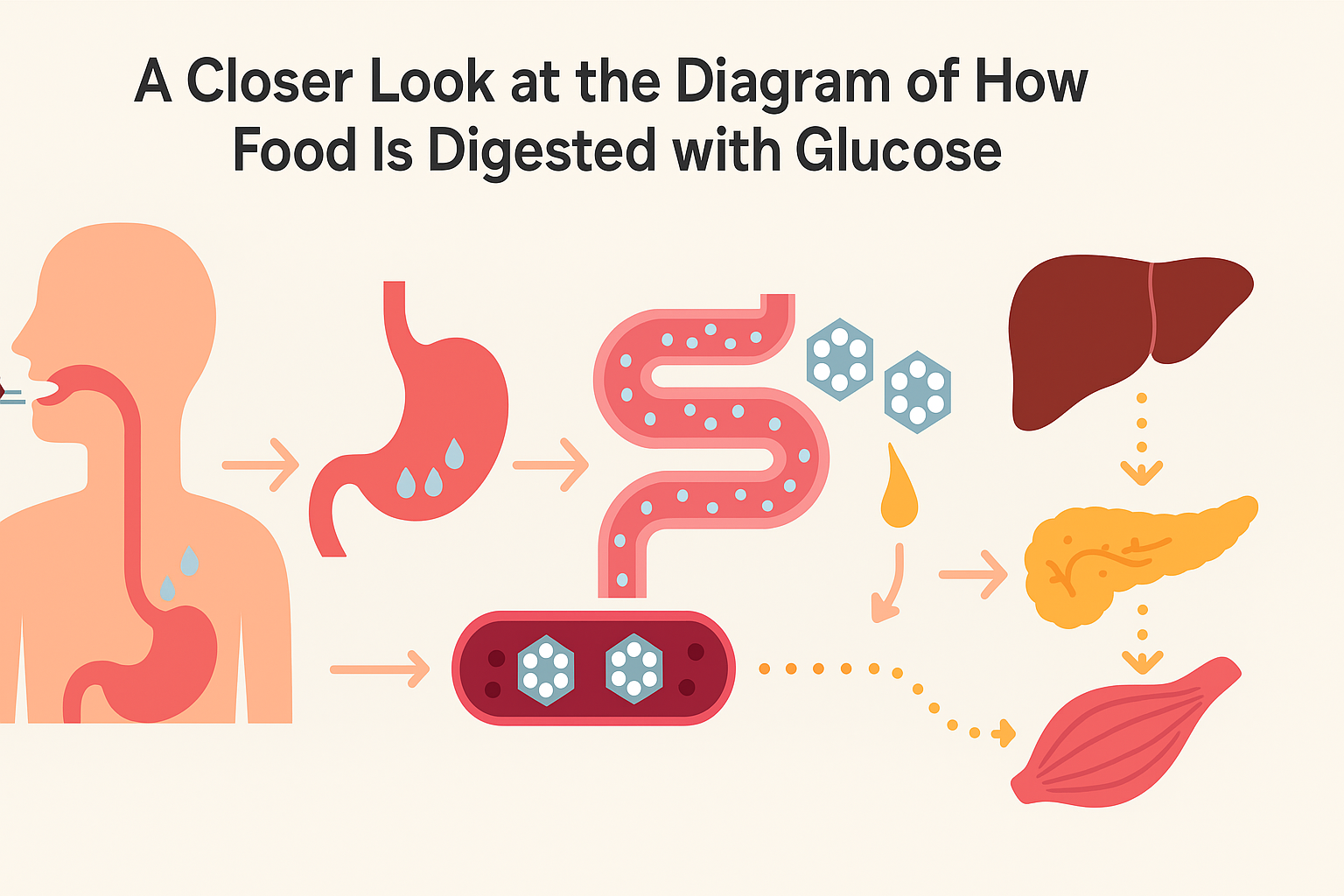
A Closer Look at the Diagram of How Food Is Digested with Glucose
For a visual representation, the diagram of how food is digested with glucose typically illustrates the sequential flow of food through the digestive tract, beginning with the mouth and ending with nutrient absorption in the intestines. Such diagrams highlight the enzymatic interactions at each stage, showing how polysaccharides are progressively reduced to glucose. This visual context not only aids in conceptual understanding but also reinforces the integrated nature of digestion and glucose metabolism. A properly labeled diagram shows how the oral cavity initiates starch digestion, how the stomach contributes to mechanical mixing, and how the small intestine finalizes carbohydrate digestion and facilitates glucose absorption.
In medical and nutritional education, such diagrams are critical tools. They visually communicate the complexity of digestion while grounding abstract biochemical concepts in anatomical reality. For those seeking clarity on metabolic pathways, a well-constructed diagram provides a roadmap for understanding how glucose becomes bioavailable and how its journey from ingestion to cellular energy production unfolds. The diagram also plays an important role in patient education, especially for individuals managing blood sugar levels due to diabetes or metabolic syndrome.
Which Organs Do Carbohydrates Help With?
To fully grasp which organs do carbohydrates help with, one must consider both short-term and long-term metabolic needs. As mentioned, the brain is heavily reliant on a continuous supply of glucose due to its high metabolic rate and inability to utilize fat directly for energy. Neurons require glucose for synaptic transmission, cognitive function, and maintaining electrical gradients across membranes. Even brief episodes of hypoglycemia can impair brain function, manifesting as confusion, fatigue, or even loss of consciousness in severe cases. Thus, carbohydrate intake is not just about energy—it is about neurological stability and mental clarity.
In the muscular system, carbohydrates are indispensable during physical activity. Muscle contractions require adenosine triphosphate (ATP), and glucose oxidation is one of the fastest ways to generate ATP. During high-intensity exercise, the body favors carbohydrate metabolism over fat due to its rapid energy yield. Moreover, glycogen stored in muscle serves as a readily available energy reservoir, and its depletion is closely associated with fatigue. This is why athletes often engage in carbohydrate loading before competitions. Clearly, carbohydrates play a significant role in muscular endurance, recovery, and overall performance.
The liver’s relationship with carbohydrates is multifaceted. It not only stores glucose but also synthesizes it from non-carbohydrate sources during fasting or low-carbohydrate intake, a process known as gluconeogenesis. This regulatory function ensures homeostasis of blood glucose levels. The liver also acts as a metabolic filter, processing nutrients absorbed from the gastrointestinal tract and determining whether to store, utilize, or redistribute glucose. This dynamic regulatory capability is crucial for balancing energy needs across the body and maintaining metabolic stability. Hence, when considering which organs do carbohydrates help with, the liver stands out as both a consumer and regulator of glucose.
How Carbohydrates Interact with the Endocrine and Nervous Systems
Beyond the primary organs involved in glucose metabolism, carbohydrates also exert significant influence over the endocrine and nervous systems. Insulin and glucagon, two key hormones secreted by the pancreas, form a feedback loop that maintains glucose balance. Carbohydrate intake triggers insulin release, promoting cellular glucose uptake and storage. In contrast, low glucose levels prompt glucagon secretion, stimulating glycogen breakdown and gluconeogenesis. This hormonal interplay exemplifies how carbohydrates are not just nutrients but also modulators of physiological balance.
In the autonomic nervous system, carbohydrate availability can affect sympathetic and parasympathetic activity. During fasting or hypoglycemia, the sympathetic nervous system is activated to promote alertness and mobilize energy reserves. Conversely, after a carbohydrate-rich meal, the parasympathetic system becomes more dominant, encouraging rest, digestion, and nutrient absorption. These shifts highlight how carbohydrate metabolism is deeply intertwined with the body’s regulatory systems, influencing not only metabolic processes but also mood, energy levels, and even circadian rhythms.
Carbohydrates also influence hormonal health in more subtle ways. Leptin and ghrelin, hormones that regulate hunger and satiety, respond to carbohydrate intake. While these hormones are influenced by total caloric intake, carbohydrates in particular have been shown to promote a quicker rise in leptin, which signals fullness. Ghrelin, the hunger hormone, decreases more rapidly after carbohydrate-rich meals compared to fat or protein-heavy ones. This interaction may explain why balanced carbohydrate consumption helps in appetite regulation and weight management.
Practical Applications: Dietary Choices That Support Glucose Balance
Translating this understanding into daily practice involves making informed choices about carbohydrate quality and quantity. Whole grains, legumes, fruits, and vegetables offer complex carbohydrates that digest more slowly and provide a steady release of glucose. These foods also contain dietary fiber, which slows gastric emptying and enhances satiety. In contrast, refined carbohydrates such as white bread and sugary snacks cause rapid glucose spikes followed by crashes, contributing to insulin resistance over time. The glycemic index and glycemic load of foods are helpful tools in selecting carbohydrate sources that align with stable blood sugar management.
Personalizing carbohydrate intake is equally important. Athletes, for example, may require higher carbohydrate consumption to match their energy expenditure, whereas individuals with insulin resistance or type 2 diabetes benefit from lower-glycemic options. Additionally, timing carbohydrate intake around physical activity can improve performance and recovery. For the general population, evenly distributing carbohydrates throughout the day helps maintain consistent energy levels and avoids large postprandial glucose swings.
Meal composition also plays a role in digestion and glucose response. Combining carbohydrates with protein, fat, and fiber helps moderate glucose absorption. For instance, pairing quinoa with grilled chicken and vegetables creates a meal that is balanced in macronutrients and supportive of metabolic health. These dietary strategies, rooted in a scientific understanding of digestion and glucose metabolism, empower individuals to make choices that nourish their bodies and sustain energy levels.
Why Understanding the Digestive Process Matters for Prevention and Wellness
Appreciating the intricacies of how the body digests food and glucose extends beyond academic interest; it is a foundational element of preventive health. Conditions like obesity, type 2 diabetes, and cardiovascular disease often stem from chronic imbalances in glucose regulation. By understanding the diagram of how food is digested with glucose and recognizing which organs do carbohydrates help with, individuals can make targeted dietary and lifestyle adjustments that reduce disease risk. This knowledge equips patients, healthcare providers, and policymakers to prioritize nutritional interventions that are both effective and sustainable.
Educational initiatives that emphasize digestive health can have widespread public health benefits. Teaching children and adolescents about how food turns into energy encourages lifelong habits of balanced eating. For adults, especially those managing chronic conditions, revisiting these fundamental concepts can illuminate new paths to wellness. When individuals comprehend how carbohydrates are processed, stored, and utilized, they are better prepared to interpret nutrition labels, regulate meal timing, and assess dietary needs during illness or stress.
In clinical practice, integrating education about glucose metabolism into consultations can improve treatment adherence and outcomes. Patients managing diabetes, for example, often benefit from visual aids and diagrams that clarify how food choices translate to blood sugar fluctuations. This promotes not only understanding but also empowerment, reinforcing the idea that nutrition is a form of medicine when applied with precision and awareness.
Frequently Asked Questions: Digestion, Glucose, and the Role of Carbohydrates
1. Can the brain function properly without a constant supply of glucose? While the brain can utilize alternative energy sources like ketone bodies during prolonged fasting or ketogenic diets, glucose remains its preferred and most efficient fuel source. This is especially true for tasks requiring immediate cognitive responses, such as decision-making, memory recall, and motor coordination. The brain’s lack of glycogen storage makes it entirely dependent on the bloodstream for glucose delivery. This reliance is often illustrated in the diagram of how food is digested with glucose, where nutrient absorption in the small intestine directly links to cerebral energy availability. Consequently, even mild dips in blood glucose can result in brain fog, reduced concentration, and mood instability.
2. How does stress affect the digestion of carbohydrates and glucose availability? Stress activates the hypothalamic-pituitary-adrenal (HPA) axis, which elevates cortisol levels and shifts energy metabolism. This physiological response often slows down digestion and can alter how efficiently carbohydrates are processed and absorbed. Elevated cortisol can cause insulin resistance over time, reducing the body’s ability to use glucose effectively. A detailed diagram of how food is digested with glucose can help visualize how digestive slowdown under stress affects nutrient flow. Moreover, stress-related hormonal shifts can interfere with which organs do carbohydrates help with most effectively, often diverting glucose to muscles in preparation for a fight-or-flight response.
3. Are certain carbohydrates better for organ health than others? Yes, the quality and complexity of carbohydrates significantly affect organ function. Whole grains, legumes, and fibrous vegetables support sustained glucose release, reducing the metabolic burden on insulin-sensitive tissues like the liver and pancreas. These foods better support the organs that carbohydrates help with, particularly by minimizing glucose spikes that can strain vascular and neurological systems. Visualizing this through a diagram of how food is digested with glucose highlights how slow-digesting carbs improve glucose distribution across organs. Additionally, complex carbs often carry micronutrients that nourish the nervous system and aid in red blood cell formation.
4. Can visual learning tools improve public understanding of glucose metabolism? Absolutely. Many individuals find it easier to understand physiological processes when presented with visual aids. A well-designed diagram of how food is digested with glucose simplifies complex mechanisms, such as enzymatic breakdown and insulin-regulated uptake, in ways that text alone cannot. Educational initiatives in clinical and community health settings increasingly use such visuals to teach patients about metabolic health. These tools can also clarify which organs do carbohydrates help with, particularly for those managing conditions like diabetes, where meal planning must be strategic and personalized. When paired with narrative explanations, diagrams enhance retention and application of health knowledge.
5. Do high-performance athletes digest and use carbohydrates differently? Elite athletes experience significant adaptations in carbohydrate metabolism due to their high energy demands and repetitive training. Their digestive efficiency often improves, allowing for quicker glucose availability from meals and supplements. Muscles in trained individuals store more glycogen and use it more efficiently during exercise, making them highly responsive to carbohydrate intake. A diagram of how food is digested with glucose in athletes would emphasize faster transitions from ingestion to muscle glycogen storage. These adaptations also highlight which organs do carbohydrates help with during performance, primarily skeletal muscles and the heart, both of which require rapid ATP replenishment.
6. How does aging affect the way carbohydrates are digested and used? As we age, the efficiency of digestion and glucose metabolism tends to decline. Enzyme production may decrease, and insulin sensitivity often diminishes, particularly in sedentary individuals. This shift can alter how carbohydrates are absorbed and which organs do carbohydrates help with most effectively, as metabolic regulation becomes less responsive. A modern diagram of how food is digested with glucose in older adults would likely show a slower digestive transit time and more variable glucose uptake. Tailoring carbohydrate choices to include more fiber, lower glycemic options, and consistent meal timing can help offset age-related changes in glucose dynamics.
7. What role do gut microbes play in carbohydrate digestion? The gut microbiome plays a crucial and underappreciated role in the breakdown of complex carbohydrates. Bacteria in the colon ferment fiber and resistant starches, producing short-chain fatty acids (SCFAs) that support colonocyte health and modulate glucose metabolism. These SCFAs can influence which organs do carbohydrates help with indirectly, by improving insulin sensitivity and reducing inflammation in peripheral tissues. A comprehensive diagram of how food is digested with glucose that includes the microbiome would illustrate how undigested carbs are processed post-absorption. Emerging research suggests that microbiome diversity can even predict how well an individual handles carbohydrate-rich meals.
8. Can poor carbohydrate digestion signal underlying health issues? Yes, difficulties digesting carbohydrates may indicate conditions like small intestinal bacterial overgrowth (SIBO), enzyme deficiencies, or even early signs of diabetes. Symptoms such as bloating, fatigue, and erratic blood sugar levels can point to problems in how glucose is metabolized or absorbed. A diagnostic tool or diagram of how food is digested with glucose can be instrumental in identifying where breakdowns in the process occur. Understanding which organs do carbohydrates help with allows clinicians to narrow down dysfunctions, such as impaired insulin signaling in the liver or reduced glucose uptake in muscles. Timely intervention can help restore balance and prevent progression to chronic conditions.
9. How can intermittent fasting affect glucose metabolism and organ function? Intermittent fasting alters the temporal dynamics of digestion and glucose utilization. During fasting periods, the body shifts from using glucose to relying more on fatty acids and ketones, especially in the brain and liver. However, refeeding periods demand precise carbohydrate management to avoid overwhelming insulin response. A dynamic diagram of how food is digested with glucose post-fasting would show accelerated absorption and insulin sensitivity reactivation. This metabolic shift also reshapes which organs do carbohydrates help with most directly, often favoring muscle replenishment and liver glycogen storage immediately following a fasted state.
10. What innovations are emerging to monitor carbohydrate digestion and glucose use in real time? Technological advancements like continuous glucose monitors (CGMs) and smart insulin pens offer real-time feedback on how the body processes carbohydrates. These tools allow individuals to visualize personal glucose curves, which can be cross-referenced with a conceptual diagram of how food is digested with glucose for better understanding. Machine learning algorithms are now being used to predict post-meal glucose responses, factoring in microbiome data, sleep, and activity levels. These innovations help identify which organs do carbohydrates help with most actively under specific conditions, such as during exercise, stress, or illness. Such personalized data-driven approaches are revolutionizing preventive nutrition and chronic disease management alike.
Conclusion: Supporting the Body with Smarter Carbohydrate Choices and Digestive Awareness
The human digestive system is a marvel of biology, converting the foods we eat into usable energy with astonishing precision and coordination. By examining the full journey of carbohydrates from ingestion to glucose absorption, and identifying which organs do carbohydrates help with, we unveil a deeper understanding of how nutrition fuels our health. The diagram of how food is digested with glucose serves not only as an educational tool but as a reminder of the elegant complexity behind every bite we take.
Glucose is not just a molecule; it is the lifeblood of brain function, muscular performance, and metabolic equilibrium. Each organ that depends on carbohydrates does so in its own way, reflecting the diverse yet interconnected nature of human physiology. By choosing nutrient-dense carbohydrates and supporting efficient digestion, individuals can enhance cognitive clarity, physical endurance, and metabolic resilience.
Further Reading:
Carbohydrate Digestion and Absorption
How Are Carbohydrates Digested?
What Are the Key Functions of Carbohydrates?