Sleep is foundational to human health, yet millions silently grapple with sleep challenges that erode their physical and mental well-being. Among the most insidious of these challenges is insomnia—a sleep disorder that quietly interferes with daily function and long-term health. If you’re wondering how to know if you have sleep insomnia, you’re not alone. The symptoms of insomnia are often misunderstood, misdiagnosed, or downplayed, especially when they arise sporadically or worsen over time. In this comprehensive guide, we will delve into the critical signs of insomnia, uncover its potential causes, explore medically approved and natural treatments, and provide practical advice for regaining control over your sleep.
You may also like: Best Evidence-Based Supplements to Lower Cholesterol Naturally
Understanding the Basics: What Is Insomnia?
Before diving into the more nuanced symptoms, it’s essential to define insomnia in clear, evidence-based terms. Insomnia is characterized by difficulty falling asleep, staying asleep, or achieving restorative sleep, despite having the opportunity to do so. This disorder may present acutely—lasting a few days or weeks due to stress or lifestyle changes—or become chronic, persisting for three months or longer. While it might be tempting to brush off a few sleepless nights, recognizing when insomnia becomes a recurring condition is vital for early intervention.
The question “what is insomnia?” is more layered than it seems. Clinically, it includes both nighttime and daytime symptoms. Beyond sleep troubles, individuals may experience fatigue, cognitive impairments, mood disturbances, and reduced performance in work or personal settings. It’s not simply about how long one sleeps, but about the quality and consistency of that sleep. Understanding insomnia meaning also involves knowing that the disorder can be primary or secondary—the latter being linked to other medical or psychiatric conditions.
How to Know If You Have Sleep Insomnia: Recognizing the Warning Signs
Identifying how to know if you have sleep insomnia requires attention to a variety of signs that go beyond occasional restlessness. One of the most telling signs is a persistent inability to fall asleep within 20 to 30 minutes of going to bed, despite feeling tired. This difficulty often extends to frequent nighttime awakenings without a clear cause, making it hard to return to sleep. Some individuals may wake up far earlier than intended and feel unrested.
Daytime symptoms are equally revealing. Chronic fatigue, irritability, impaired concentration, and a feeling of being “mentally foggy” are common complaints. Physical symptoms such as tension headaches or gastrointestinal distress may also manifest. Importantly, these effects occur even when you’ve had the chance to sleep, which differentiates insomnia from sleep deprivation due to external factors. These multifaceted indicators form the crux of how to find out if you have insomnia and whether it merits clinical attention.
Why Can’t I Sleep? Exploring Underlying Causes and Risk Factors
Asking “why can’t I sleep?” often uncovers a labyrinth of physiological, psychological, and environmental factors. Stress is one of the leading triggers of both acute and chronic insomnia. Anxiety, depression, and other mood disorders frequently disrupt sleep patterns by overactivating the nervous system, leading to hyperarousal and intrusive thoughts at night.
Medical conditions are another significant factor. Diseases causing insomnia include chronic pain syndromes like arthritis, gastrointestinal reflux disease (GERD), asthma, and neurodegenerative conditions such as Parkinson’s and Alzheimer’s. Hormonal imbalances, especially in women, contribute to sleep disturbances—highlighting the role of causes of insomnia in females such as menopause, PMS, and thyroid dysfunction.
In men, sleep issues often stem from insomnia causes in men like untreated sleep apnea, high stress, and substance use. Lifestyle habits—such as excessive screen time, caffeine consumption late in the day, or irregular sleep schedules—also exacerbate insomnia symptoms. Identifying root causes is essential for targeted treatment, which brings us to the next section.
The Frustrating Nature of Sudden and Intermittent Insomnia
Can insomnia come and go? The answer is a resounding yes, and this variability often confuses sufferers. Episodic insomnia might arise due to temporary stressors—a major life change, travel, or illness—and then seemingly resolve. However, even if it vanishes, it leaves behind the possibility of recurrence. This unpredictable nature underscores the question “can insomnia go away permanently,” which is best answered through personalized treatment plans and lifestyle adjustments.
For some, sudden insomnia becomes a regular occurrence, reemerging when the body and mind are under strain. The sporadic presentation can make individuals question the seriousness of their symptoms, leading them to delay seeking professional help. However, just because insomnia is intermittent doesn’t mean it should be ignored. Chronic patterns often start with occasional episodes that escalate in severity and frequency.

How to Know If You Have Sleep Insomnia: Behavioral and Cognitive Clues
When examining how to know if you have sleep insomnia, behavioral and cognitive changes offer vital clues. Many people begin developing anxiety around bedtime itself, fearing the inevitable tossing and turning. This phenomenon, known as conditioned arousal, reinforces sleeplessness, making it harder to fall asleep each night.
Negative sleep thoughts also perpetuate the cycle. You might find yourself catastrophizing about the impact of poor sleep on your work performance or health, which paradoxically heightens stress and delays sleep onset. Some individuals even begin to adopt maladaptive coping behaviors—such as increasing caffeine or alcohol intake—that further disrupt circadian rhythms.
Cognitive impairments, such as memory lapses, slowed reaction times, and decision-making difficulties, compound the issue. If you’re routinely making errors, forgetting conversations, or struggling to focus, insomnia could be the hidden culprit. These signs go beyond nighttime symptoms, helping to address the question “how do you tell if you have insomnia” through a more comprehensive lens.
Do I Have Insomnia or Just a Few Bad Nights?
It can be challenging to differentiate between transient sleep disturbances and clinical insomnia. Asking yourself, “do I have insomnia?” means evaluating the frequency, duration, and impact of your symptoms. Clinical insomnia is diagnosed when sleep difficulties occur at least three nights per week and persist for at least three months, coupled with functional impairment during the day.
If your symptoms fluctuate but consistently interfere with daily life, you may fall under the spectrum of chronic insomnia. Insomnia diagnosis usually involves sleep questionnaires, sleep diaries, and sometimes a polysomnography or actigraphy test. These tools allow healthcare providers to distinguish between insomnia and other sleep disorders such as sleep apnea, restless leg syndrome, or circadian rhythm disruptions.
Understanding where you stand is the first step toward targeted treatment. Whether you’re dealing with acute episodes or enduring long-term patterns, validating your experience is essential. Early recognition not only improves treatment outcomes but also helps prevent comorbid conditions like depression and cardiovascular disease.
The Ripple Effects of Severe Insomnia Over the Years
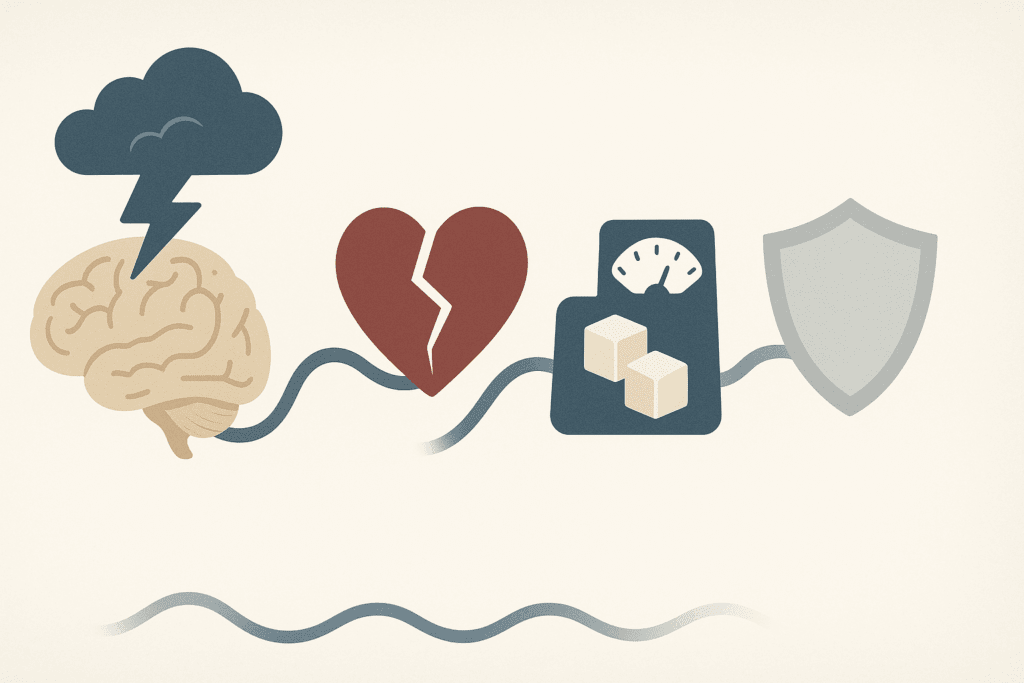
The long-term effects of severe insomnia for years are not merely frustrating—they are clinically significant. Chronic insomnia is associated with an increased risk of mood disorders, particularly major depression and generalized anxiety. Cardiovascular problems, such as hypertension and heart disease, are also more common in individuals who experience persistent sleep deprivation.
Metabolic issues like weight gain, insulin resistance, and even type 2 diabetes have been linked to chronic poor sleep. The immune system, too, takes a hit, leaving individuals more vulnerable to infections. Cognitively, prolonged insomnia may accelerate age-related decline, reducing memory function and executive skills.
These ripple effects affirm why early intervention matters. Persistent insomnia reshapes how the brain and body function, creating a cycle of deterioration that becomes harder to reverse over time. Knowing the true cost of inaction can motivate individuals to seek help and pursue meaningful change.
How to Know If You Have Sleep Insomnia: The Role of Emotional Regulation
Among the subtler signs of insomnia is its impact on emotional regulation. Individuals often report feeling unusually irritable, impatient, or overwhelmed by minor stressors. These emotional shifts are not just side effects; they are evidence of neurological changes associated with poor sleep. Insufficient rest reduces the brain’s ability to process emotional information, particularly in areas like the amygdala and prefrontal cortex.
Mood swings, increased sensitivity to criticism, and social withdrawal are all potential red flags. If you notice these patterns alongside sleep disturbances, they may help confirm whether you’re dealing with insomnia or another underlying issue. Understanding these emotional symptoms provides a fuller picture of how to know if u have insomnia and how deeply it affects both interpersonal and intrapersonal dynamics.
Exploring the Landscape of Insomnia Treatments and Therapies
When it comes to managing insomnia, a one-size-fits-all approach simply doesn’t work. Insomnia treatments range from cognitive-behavioral therapy for insomnia (CBT-I) to pharmacological options like benzodiazepines, non-benzodiazepine sedatives, and melatonin receptor agonists. CBT-I, in particular, has emerged as the gold standard for chronic insomnia treatment, helping patients reframe sleep-related thoughts and improve sleep hygiene behaviors.
However, pharmacotherapy may be necessary for those experiencing acute or severe insomnia. This should always be done under medical supervision due to the risk of dependency and side effects. Newer insomnia therapies focus on targeting the biological mechanisms of wakefulness, offering a more nuanced approach than older sedatives.
For those wary of medication, natural remedies for insomnia include valerian root, chamomile tea, magnesium supplements, and lifestyle changes like consistent sleep schedules and screen-free wind-down routines. While not as potent as prescription drugs, these options can support mild to moderate insomnia and serve as adjuncts to behavioral therapy.
The Persistent Question: Does Insomnia Go Away?
Does insomnia go away completely? In many cases, yes—but not without effort. Addressing insomnia requires consistent application of treatment strategies, as well as an understanding that sleep patterns may take weeks or months to stabilize. The notion of “the cure for insomnia” is somewhat misleading, as most treatments aim for management rather than eradication.
However, many people do experience full remission, particularly when the underlying causes—such as stress, hormonal imbalance, or poor sleep habits—are identified and corrected. The idea that insomnia is a life sentence is inaccurate. With the right tools, mindset, and medical support, it is entirely possible to re-establish healthy sleep patterns.
How to Cure Insomnia in 12 Minutes: Debunking Myths and Finding Real Solutions
One of the most searched queries online is how to cure insomnia in 12 minutes. While catchy, this phrase often leads to disappointment, as chronic insomnia cannot be solved with a single breathing technique or sleep hack. That said, short-term relaxation methods—such as the military sleep method, progressive muscle relaxation, and guided imagery—can indeed initiate the sleep process quickly for some individuals.
These techniques may work especially well for those whose insomnia is driven by anxiety or racing thoughts. However, they are not standalone cures. Sustainable improvement involves layered approaches that combine behavioral change, medical evaluation, and sometimes pharmacological intervention. Real healing lies not in quick fixes but in consistent practice and personalized strategies.
Were You Able to Sleep? The Power of Self-Reflection and Sleep Journaling
Tracking your sleep can offer invaluable insight into your insomnia patterns. Simple questions like “were you able to sleep last night?” can evolve into detailed journaling that captures bedtime, wake times, number of awakenings, mood upon waking, and factors like caffeine or alcohol use. Over time, patterns emerge that help identify triggers and effective interventions.
Sleep diaries are also useful during clinical evaluations, providing objective data for insomnia diagnosis and helping therapists tailor cognitive-behavioral strategies. The act of self-monitoring not only empowers individuals but also fosters accountability and mindfulness. By cultivating awareness, sufferers can begin to reclaim control over their sleep narrative.
Frequently Asked Questions: Advanced Insights on Insomnia
How to Know If You Have Sleep Insomnia When Symptoms Aren’t Obvious
Sleep insomnia doesn’t always manifest in overt ways like hours of tossing and turning. In fact, some individuals fall asleep relatively quickly but still wake up exhausted, experiencing fragmented or non-restorative sleep. This condition, often mistaken for general fatigue or overwork, can be a subtle sign of insomnia. Monitoring cognitive performance, mood fluctuations, and energy levels throughout the day can provide clues. If you’re frequently asking yourself, “Why can’t I focus even after eight hours in bed?” it may be time to consider how to know if you have sleep insomnia even when the signs are understated.
Is There a Way to Find Out How to Know If You Have Sleep Insomnia Without Going to a Sleep Clinic?
While clinical evaluations like polysomnography offer the most comprehensive data, many people can begin the process of understanding their sleep patterns at home. Wearable sleep trackers with validated algorithms now provide rich insight into sleep stages and interruptions. Apps that combine sleep logging with mood, diet, and physical activity can offer a multi-dimensional look into one’s nighttime habits. These tools help reveal whether recurring issues like sudden insomnia or fragmented sleep may be escalating into a chronic issue. For many, these self-assessments are the first step toward realizing how to know if you have sleep insomnia and when to seek professional intervention.
What Are the Most Overlooked Causes of Insomnia in Females?
Beyond the commonly cited reasons like hormonal fluctuations from menopause or PMS, there are nuanced causes of insomnia in females that are frequently overlooked. Conditions like endometriosis and polycystic ovarian syndrome (PCOS) can disrupt sleep due to chronic pain, anxiety, and hormonal imbalances. Caregiving responsibilities—whether for children, aging parents, or both—also uniquely impact women’s stress and sleep cycles. Additionally, female patients are more likely to internalize stress and anxiety, leading to a higher incidence of psychophysiological insomnia. These layered factors underscore the importance of personalized evaluation for women facing recurring sleep challenges.
Can Insomnia Come and Go Even If I’m Not Stressed?
Yes, insomnia can come and go due to a variety of subtle or cyclical triggers unrelated to stress. Seasonal changes in daylight exposure, travel, shifts in diet, and even phases of the moon can contribute to changes in sleep patterns. In some cases, individuals may unknowingly adjust behaviors—like increasing caffeine intake or altering exercise habits—that disrupt their circadian rhythms. For those with high sleep reactivity, even slight lifestyle changes can trigger temporary insomnia. Recognizing that intermittent symptoms may precede chronic problems can motivate proactive steps before insomnia becomes ingrained.
What’s the Relationship Between Severe Insomnia for Years and Long-Term Brain Function?
When severe insomnia persists for years, the implications on brain function are both profound and measurable. Studies have shown that chronic sleep deprivation affects the hippocampus, a region critical for memory consolidation. Neuroimaging reveals reductions in gray matter volume among long-term insomniacs, correlating with reduced cognitive flexibility and slower processing speeds. Emotional regulation also deteriorates, increasing the risk of mood disorders and even suicidal ideation. While some damage may be reversible with consistent sleep recovery, persistent insomnia accelerates neurodegenerative risks. Thus, managing long-standing insomnia isn’t just about sleep—it’s about preserving long-term brain health.
How Do You Tell If You Have Insomnia When You’re Already Dealing With Another Health Condition?
When managing chronic illnesses like diabetes, arthritis, or asthma, it can be difficult to separate symptoms of the condition from insomnia. Diseases causing insomnia often have overlapping features—like pain, breathing issues, or medication side effects—that confuse diagnosis. In these cases, the best way to distinguish insomnia symptoms is to track patterns unrelated to disease flare-ups. For example, if sleep disruptions persist during periods of remission or stable health, it may point more specifically to insomnia. Discussing these trends with a provider can ensure that your insomnia diagnosis accounts for both primary and secondary causes.
Can Natural Remedies for Insomnia Actually Replace Medication?
Natural remedies for insomnia can be remarkably effective when used consistently and under the right circumstances. Herbs like valerian root and lemon balm, when used in therapeutic dosages, have demonstrated mild sedative properties in clinical trials. Magnesium, L-theanine, and glycine can also modulate neurotransmitters involved in the sleep-wake cycle. However, these options are generally more beneficial for mild to moderate insomnia and may not suffice for those with severe or chronic symptoms. When combined with behavioral strategies and lifestyle modifications, they can serve as a gentle yet impactful alternative or complement to conventional insomnia treatments.
How to Cure Insomnia in 12 Minutes: Is There Any Truth to Quick Fix Techniques?
The concept of how to cure insomnia in 12 minutes is mostly misleading if interpreted as a permanent solution. That said, rapid relaxation techniques—such as diaphragmatic breathing, the 4-7-8 method, or guided progressive muscle relaxation—can indeed facilitate quicker sleep onset for those experiencing transient stress. These techniques are especially helpful in interrupting cycles of rumination that contribute to why you can’t fall asleep. Used regularly, they can condition the body to associate bedtime with calmness. However, they should be part of a broader toolkit, not a stand-alone treatment, particularly when dealing with chronic insomnia treatment plans.
Will Insomnia Go Away on Its Own If I Just Wait It Out?
For some individuals, particularly those with sudden insomnia triggered by situational stress, sleep patterns may return to normal once the stressor resolves. However, for many, the act of struggling with sleep creates a learned association of anxiety and hyperarousal that perpetuates the problem. Waiting without intervention often allows these maladaptive patterns to become entrenched. The question “will insomnia go away on its own” depends on the underlying causes and the individual’s vulnerability to chronicity. Proactively addressing root causes and implementing insomnia therapies early increases the odds of full recovery without long-term consequences.
How to Know If You Have Sleep Insomnia Versus Normal Sleeplessness
Differentiating how to know if you have sleep insomnia versus experiencing normal sleeplessness depends largely on frequency, duration, and daytime impact. Normal sleeplessness is often situational and passes without significant interference in daily life. In contrast, insomnia symptoms linger for weeks or months and often lead to functional impairments like reduced concentration or emotional instability. Another marker is anticipatory anxiety about bedtime, which rarely occurs in transient cases. Recognizing this difference empowers people to stop minimizing their symptoms and seek appropriate insomnia treatments before the condition becomes debilitating.
Final Reflections: How to Know If You Have Insomnia and What to Do Moving Forward
Insomnia is far more than an occasional inconvenience—it is a medical condition with profound implications for physical, emotional, and cognitive health. Learning how to know if you have sleep insomnia means attuning to both the overt and subtle signals your body and mind are sending. From nighttime restlessness to daytime dysfunction, the signs are varied but interconnected, painting a comprehensive portrait of disordered sleep.
Understanding the causes—whether rooted in biology, psychology, or behavior—is the first step toward effective treatment. Whether you are struggling with sudden insomnia or have endured severe insomnia for years, there are solutions grounded in medical science and compassionate care. With tools ranging from cognitive-behavioral therapy to natural remedies, the path to better sleep is navigable for most individuals.
Above all, be patient with yourself. Sleep is a delicate balance of physiology and environment, and restoring it takes time. Whether you’re exploring insomnia therapies for the first time or revisiting treatment options after setbacks, know that improvement is possible. Let this knowledge inspire action, not fear. The sooner you begin, the sooner restful nights and brighter days can return.


