In the realm of cardiovascular health, few metrics are as telling as heart rate. Whether you’re an athlete tracking your fitness, a patient managing cardiovascular disease, or simply someone concerned about overall wellness, understanding how to raise heart rate safely and effectively is critical. A healthy heart rate not only reflects current cardiac function but also serves as a window into the broader state of circulatory efficiency. In medical and wellness contexts alike, improving circulation and supporting cardiovascular function can contribute to reduced disease risk, enhanced energy, and better quality of life. For many, this involves understanding how to increase heart rate in a controlled, safe manner that aligns with individual health needs.
You may also like: Top Cardiologist-Approved Cardio Workouts to Improve Cardiovascular Fitness and Heart Health Naturally
This article offers a comprehensive, evidence-based exploration of safe heart rate elevation strategies, grounded in the principles of cardiovascular physiology and aligned with medical best practices. We’ll examine natural methods to stimulate cardiac output, uncover the factors that increase heart rate and blood pressure, and clarify when heart rate elevation is beneficial versus potentially harmful. Throughout, the advice remains rooted in expert recommendations and the latest scientific evidence, ensuring that readers receive medically accurate, trustworthy information suitable for publication under the cardiovascular health category at MedNewsPedia.com.
Why Raising Heart Rate Matters for Cardiovascular Health
Heart rate is more than a number—it is a vital sign that reflects how efficiently the heart pumps blood through the body. A temporarily elevated heart rate can be a healthy and adaptive response, particularly during physical exertion or emotional arousal. When managed properly, this increase supports oxygen delivery to muscles and organs, enhances metabolic function, and improves the elasticity and responsiveness of blood vessels. This is especially relevant when developing exercise regimens or managing conditions like hypotension, bradycardia, or peripheral circulation issues.
Raising heart rate through safe, doctor-recommended methods can improve cardiac output, boost cardiovascular endurance, and contribute to lower resting heart rates over time. This paradoxical benefit—where increasing heart rate during activity leads to a lower resting rate—occurs due to improved cardiac efficiency and autonomic nervous system balance. It’s important to recognize that not all heart rate increases are created equal; some are the result of healthy stressors like exercise, while others may stem from pathological factors like fever, infection, or anxiety. For individuals wondering how to raise heart rate effectively, the answer lies in selecting the right stimuli at the right time, guided by medical insight.
Understanding Resting Heart Rate and When to Increase It
Resting heart rate (RHR) is the number of heartbeats per minute when you are at complete rest. For most healthy adults, a normal RHR ranges between 60 to 100 beats per minute. Athletes and those with high cardiovascular fitness often have lower resting rates, sometimes dipping below 60 BPM—a condition known as physiological bradycardia. While a lower RHR generally signifies strong cardiac efficiency, a heart rate that is too low or unresponsive to activity may indicate underlying concerns.
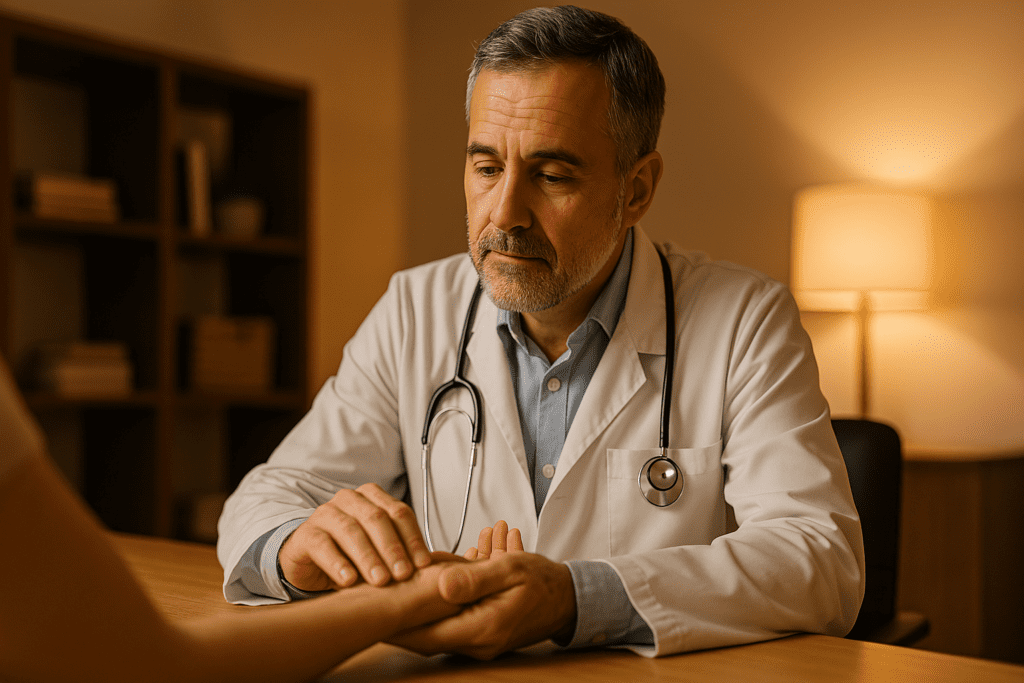
There are several scenarios where a person may need to actively consider how to increase heart rate. These include cases of fatigue, hypotension, poor circulation, dizziness on standing (orthostatic hypotension), or cardiac dysautonomia. In such instances, temporarily raising heart rate through movement or dietary interventions can promote blood flow and relieve symptoms. Importantly, decisions around heart rate modulation should always take place in consultation with a healthcare provider, particularly for those with pre-existing cardiovascular or metabolic conditions.
Doctors often evaluate the broader clinical picture when deciding whether a patient would benefit from interventions that raise heart rate. These evaluations may include blood pressure measurements, tilt table tests, electrolyte panels, and cardiac stress testing. Understanding this context helps demystify the concept for those seeking to improve circulation and cardiovascular function in a medically responsible way.
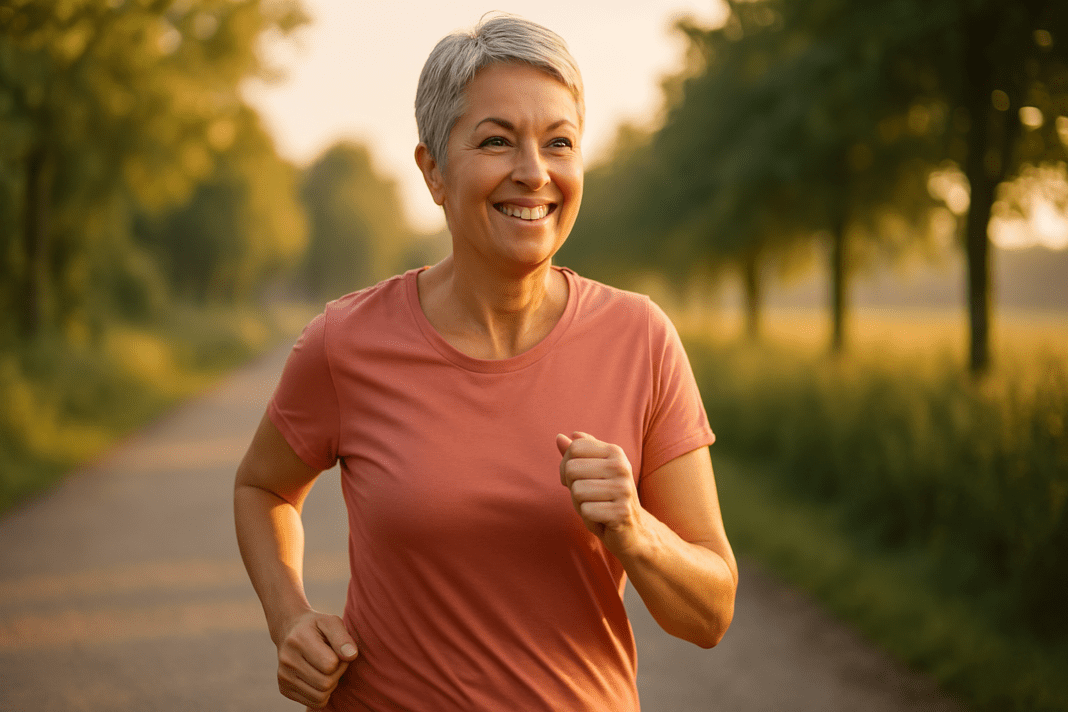
Exercise: The Safest and Most Effective Way to Raise Heart Rate
Physical activity remains the gold standard for raising heart rate in a controlled and beneficial way. Exercise increases heart rate by activating the sympathetic nervous system and increasing the body’s demand for oxygen. This triggers vasodilation in the muscles, promotes cardiac output, and enhances oxygen delivery. Whether one is walking briskly, cycling, swimming, or engaging in strength training, any form of structured movement elevates heart rate and stimulates cardiovascular function.
Aerobic exercise is particularly effective at increasing heart rate while also providing long-term benefits such as improved endothelial function, reduced arterial stiffness, and better autonomic regulation. High-Intensity Interval Training (HIIT), which alternates short bursts of intense activity with periods of rest, has been shown in numerous studies to improve both maximal heart rate and heart rate variability—a key indicator of cardiac resilience. Importantly, individuals can start with low-intensity activities and gradually progress, tailoring programs to their age, fitness level, and medical history.
Patients frequently ask how to raise heart rate without overexerting themselves. For beginners, this may involve 20 to 30 minutes of moderate activity such as walking, water aerobics, or light cycling. Even short, frequent sessions throughout the day can provide cumulative cardiovascular benefits. Resistance training also contributes, though its heart rate elevation may be less sustained than aerobic workouts. Importantly, consistent activity not only raises heart rate during exercise but contributes to long-term adaptations that improve overall heart function.
Lifestyle Factors That Naturally Increase Heart Rate and Support Circulation
Beyond exercise, a range of lifestyle factors can gently and safely increase heart rate while promoting healthy circulation. One of the most accessible is hydration. When the body is dehydrated, blood volume decreases, making the heart work harder to maintain adequate perfusion. Drinking sufficient water supports stroke volume and helps prevent reflex tachycardia caused by low circulating volume.
Temperature also influences heart rate. Warm environments cause vasodilation and modestly increase cardiac output to help regulate core temperature. Saunas, warm showers, and thermotherapy have been shown to elevate heart rate while supporting vascular flexibility. However, these should be used with caution in individuals with heart failure or uncontrolled blood pressure.
Caffeine is another common and medically acknowledged stimulant that raises heart rate by activating the central nervous system. Found in coffee, tea, and certain supplements, caffeine increases both systolic blood pressure and pulse rate in the short term. For those wondering how to increase heart rate quickly, moderate caffeine intake can be effective, although it should be limited to under 400 mg per day for most healthy adults to avoid overstimulation or palpitations.
Stress, particularly acute stress, also raises heart rate through activation of the hypothalamic-pituitary-adrenal (HPA) axis and release of catecholamines. While chronic stress is harmful, controlled exposure to mild stressors—such as cold exposure or time-limited challenges—can trigger hormetic responses that improve cardiovascular conditioning. These adaptive stressors are useful when applied intentionally and with awareness of personal health status.
Dietary Considerations for Supporting a Healthy Heart Rate
Nutritional choices can play a significant role in cardiovascular stimulation and overall heart rate regulation. Foods rich in antioxidants, nitrates, and electrolytes support vascular tone and blood flow, thereby modulating heart rate responses. Leafy greens like spinach and arugula contain high levels of nitrates, which convert to nitric oxide and help improve vasodilation and cardiac output.
Electrolytes such as potassium, magnesium, and calcium are essential for maintaining electrical conductivity in the heart muscle. A deficiency in these nutrients can result in arrhythmias, bradycardia, or exaggerated heart rate responses. Potassium-rich foods like bananas, avocados, and sweet potatoes, alongside magnesium sources like almonds and dark chocolate, contribute to more stable cardiovascular activity. In cases where individuals feel sluggish or experience dizziness upon standing, increasing electrolyte intake may offer both circulatory and heart rate benefits.
Spicy foods, such as those containing capsaicin from chili peppers, have also been shown to temporarily increase heart rate and metabolic rate by stimulating the sympathetic nervous system. This thermogenic effect, while short-lived, can enhance circulation and serve as a mild cardiovascular activator. However, individuals with gastrointestinal sensitivities or acid reflux should approach spicy foods with caution, balancing stimulation with comfort.
For those looking for how to increase heart rate naturally and sustainably, focusing on whole foods, minimizing processed sugar, and maintaining adequate hydration remain foundational strategies. It’s not simply about a one-time spike in pulse but cultivating a physiological environment that supports efficient and responsive cardiovascular function.
Medical Conditions and Physiological Factors That Influence Heart Rate
Understanding the underlying mechanisms of heart rate elevation also involves examining internal factors that modulate cardiac activity. The autonomic nervous system (ANS) plays a central role, with the sympathetic branch responsible for stimulating heart rate and the parasympathetic branch for slowing it. Imbalances in ANS tone can result in either excessive heart rate (tachycardia) or an insufficient response to stimuli (bradycardia).
Endocrine function is another key player. Thyroid hormones, particularly T3 and T4, have direct effects on cardiac contractility and heart rate. Hyperthyroidism often presents with elevated resting heart rates and palpitations, while hypothyroidism may suppress cardiac output. Likewise, adrenal hormones like cortisol and epinephrine influence heart rate by modulating vascular tone and metabolic readiness. These hormonal pathways illustrate how internal health conditions can become primary factors that increase heart rate and blood pressure, including during non-exertional activities.
In some cases, medications or medical devices are necessary to regulate heart rate, particularly in individuals with arrhythmias, autonomic dysfunction, or postural orthostatic tachycardia syndrome (POTS). Beta blockers, for instance, intentionally lower heart rate, while certain stimulants may raise it. For those with pacemakers or implantable devices, heart rate modulation is managed through external programming. These medical interventions demonstrate the importance of tailoring heart rate strategies to each individual’s clinical profile.
Moreover, age, sex, and fitness level all influence how easily and how high one’s heart rate can rise. Younger individuals typically have higher maximal heart rates, while older adults often exhibit a blunted response due to reduced beta-adrenergic sensitivity. Women may have slightly higher resting heart rates than men due to hormonal influences and smaller average heart size. Recognizing these nuances helps patients and practitioners alike determine the best approach when deciding how to raise heart rate for optimal benefit.
Recognizing Unhealthy Heart Rate Elevation and When to Seek Help
While there are many benefits to learning how to raise heart rate safely, it is equally important to recognize when elevated heart rate becomes a concern. Not all heart rate increases are benign. Persistent tachycardia—especially at rest—may indicate arrhythmias, dehydration, fever, anemia, or underlying cardiovascular dysfunction. It can also be a side effect of medications, withdrawal from certain drugs, or overuse of stimulants.
If heart rate elevation is accompanied by chest pain, shortness of breath, dizziness, fainting, or palpitations, it is essential to seek medical attention. These symptoms may signal conditions such as supraventricular tachycardia, atrial fibrillation, or even early stages of heart failure. In such cases, interventions that raise heart rate may do more harm than good and should only be undertaken under direct clinical supervision.
It’s also important to understand that some factors that increase heart rate and blood pressure include emotional stress, infections, stimulant use, and pain. While these may be temporary or adaptive responses, they can become maladaptive when sustained. Tracking heart rate trends using wearable devices or clinical monitoring can help patients identify patterns and distinguish between healthy activation and pathological overactivity.
Healthcare providers may perform electrocardiograms (ECGs), echocardiograms, or Holter monitor testing to evaluate irregular heart rate patterns. These diagnostics help clarify whether interventions are needed to slow, stimulate, or stabilize heart rate. Patients should never attempt aggressive heart rate modification strategies without professional evaluation, especially if they have cardiovascular or metabolic conditions.
Practical Daily Habits That Support Heart Rate Responsiveness and Cardiovascular Strength
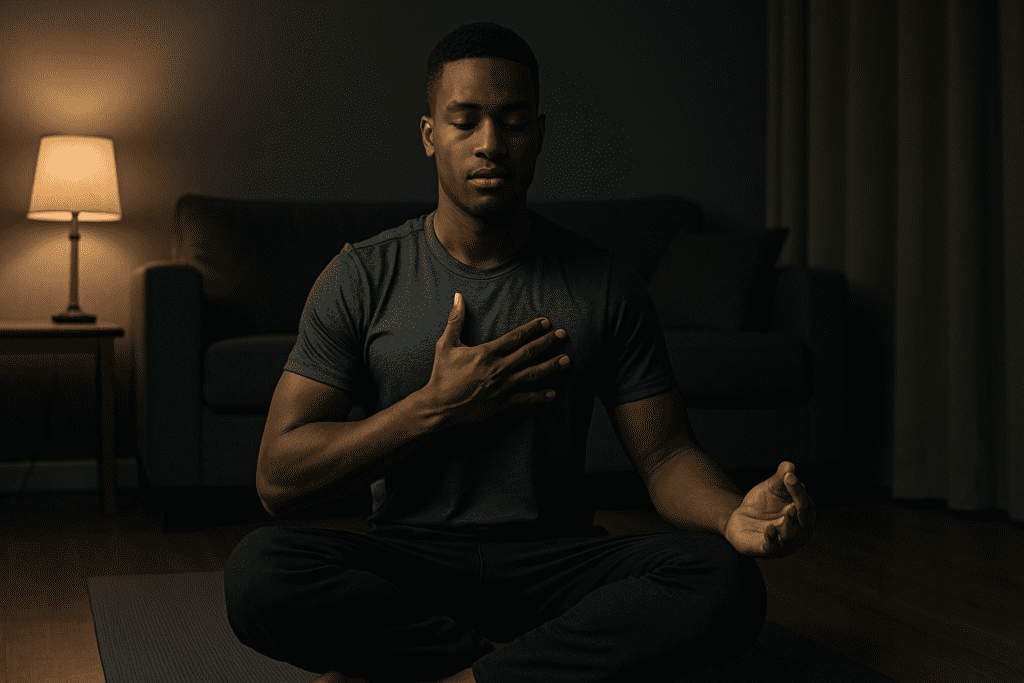
A proactive approach to cardiovascular health involves integrating small, sustainable habits that support both heart rate flexibility and circulatory robustness. These include prioritizing sleep, as inadequate rest disrupts autonomic balance and leads to erratic heart rate behavior. Good sleep hygiene—such as maintaining a consistent bedtime, limiting blue light, and managing caffeine intake—directly influences the body’s recovery and heart rate stability.
Mind-body practices such as yoga, breathwork, and meditation enhance vagal tone and promote heart rate variability, a marker of autonomic adaptability. Paradoxically, while these practices may lower heart rate during rest, they improve the body’s ability to raise and regulate it appropriately during exertion. Over time, this balance supports resilience and reduces cardiovascular risk.
Social interaction and emotional well-being also impact heart rate regulation. Positive relationships, laughter, and reduced isolation correlate with healthier autonomic profiles. Conversely, chronic stress, conflict, and emotional trauma are among the lesser-known factors that increase heart rate and blood pressure. Addressing these emotional contributors is just as important as focusing on physical activity or diet.
Daily movement—even outside of formal exercise—is also beneficial. Taking stairs instead of elevators, walking after meals, and incorporating standing desks can provide gentle cardiovascular activation throughout the day. For many, learning how to raise heart rate naturally involves stringing together these micro-movements to build a baseline of circulatory stimulation that adds up over time.
Frequently Asked Questions (FAQ): How to Raise Heart Rate Safely
1. Can mental imagery or visualization techniques help increase heart rate and improve circulation?
Yes, mental imagery—particularly when focused on movement or adrenaline-inducing scenarios—can stimulate the autonomic nervous system and cause a modest rise in heart rate. Athletes often use visualization to prepare for competition, which primes the cardiovascular system even before physical exertion begins. If you’re exploring how to raise heart rate without moving, guided imagery involving high-intensity physical activity or emotionally stimulating experiences can create a sympathetic response. This practice, while not a substitute for exercise, can support individuals with mobility limitations or during recovery phases. Among the lesser-known factors that increase heart rate and blood pressure include emotional arousal triggered by memory, visualization, and even music.
2. What are some emerging technologies that help monitor and regulate heart rate in real time?
Wearable fitness trackers and smartwatches have evolved far beyond step counters. Newer devices can track real-time changes in heart rate variability (HRV), detect irregular rhythms, and provide insights into stress recovery cycles. Some models are even integrating AI to recommend personalized suggestions on how to increase heart rate through movement or breathing exercises based on your historical data. Biofeedback tools now allow users to view fluctuations in their cardiovascular responses to meditation or posture changes, helping them learn how to raise heart rate appropriately without overshooting healthy thresholds. As technology advances, the ability to identify which factors that increase heart rate and blood pressure include subtle emotional or postural shifts will become even more refined.
3. How does body position impact heart rate, and can adjusting posture raise it safely?
Shifts in posture significantly influence heart rate through baroreceptor reflexes and blood pressure compensation. Moving from lying down to standing up prompts the heart to beat faster to counteract gravitational pooling of blood in the legs. For individuals with orthostatic intolerance, even mild positional changes can cause a dramatic pulse increase. For those looking into how to raise heart rate subtly and safely, alternating between sitting and standing, or even incorporating light dynamic stretching, can provide cardiovascular stimulation without formal exercise. Some of the more surprising factors that increase heart rate and blood pressure include prolonged sitting, which may prompt the body to compensate via elevated sympathetic tone.
4. What role does intermittent fasting play in heart rate regulation?
Intermittent fasting influences hormonal balance, including insulin, cortisol, and adrenaline—each of which impacts cardiovascular behavior. In the early hours of fasting, heart rate often decreases due to reduced metabolic activity, but prolonged fasting can cause a slight increase in heart rate due to rising catecholamine levels. For individuals seeking strategies on how to increase heart rate for metabolic enhancement, strategic fasting paired with hydration and electrolytes may support sympathetic tone. However, caution is warranted for those with low blood pressure or underlying conditions. Some factors that increase heart rate and blood pressure include fasting-induced stress responses, especially during prolonged caloric restriction without appropriate nutrient balance.
5. Is there a connection between social interaction and heart rate modulation?
Social connection—particularly involving meaningful conversation, laughter, or emotional engagement—can trigger subtle increases in heart rate by activating the sympathetic nervous system. Interestingly, social settings can also stimulate cardiovascular recovery depending on the emotional tone. For people wondering how to raise heart rate in non-exercise contexts, engaging in stimulating dialogue or participating in group activities like dancing or public speaking can provide a natural cardiovascular boost. Beyond behavioral causes, the emotional components of socializing are among the psychological factors that increase heart rate and blood pressure. These effects demonstrate the mind-heart connection and the value of emotional well-being in cardiovascular health.
6. Can cold exposure, such as ice baths or cold showers, increase heart rate?
Yes, brief exposure to cold environments initiates a stress response that sharply elevates heart rate as part of the body’s thermoregulatory process. While commonly used to reduce inflammation and support recovery, cold immersion can paradoxically serve as a method of cardiovascular stimulation. If you’re learning how to increase heart rate through environmental means, controlled cold exposure is both powerful and efficient—though not suitable for everyone. It’s essential to monitor duration and temperature carefully, as overexposure can lead to arrhythmias in sensitive individuals. Cold-induced vasoconstriction is also among the physiological factors that increase heart rate and blood pressure include during short-term sympathetic activation.
7. Are there pharmacological ways to raise heart rate, and when are they used clinically?
Medications such as atropine, epinephrine, or isoproterenol are sometimes used in emergency or clinical settings to raise heart rate in patients experiencing bradycardia or cardiac arrest. Outside acute care, drugs like midodrine or fludrocortisone may be prescribed to individuals with chronic hypotension or dysautonomia. However, for most healthy individuals seeking how to raise heart rate, pharmaceutical intervention is neither necessary nor recommended without a diagnosed medical condition. It’s critical to recognize that pharmacological methods often target very specific causes, and self-administration can pose significant cardiovascular risks. Among the clinical factors that increase heart rate and blood pressure include drug side effects, interactions, and underlying autonomic dysfunction.
8. How do cultural and spiritual practices like drumming or chanting affect heart rate?
Cultural rituals that involve rhythmic movement, chanting, or drumming have been shown to modulate both heart rate and respiratory rhythm. These practices create synchronization between breathing and cardiovascular cycles, subtly influencing autonomic tone. For those exploring unique approaches on how to increase heart rate, participating in structured rhythmic activities within cultural or spiritual settings may offer a holistic and community-driven method. These rituals often blend physical engagement, vocalization, and emotional intensity, leading to mild heart rate elevation and enhanced circulation. Beyond biology, psychological and spiritual engagement are lesser-known factors that increase heart rate and blood pressure include ceremonial intensity and collective emotional resonance.
9. What is the long-term impact of regularly raising your heart rate on brain health?
Long-term cardiovascular stimulation through exercise and structured heart rate elevation improves cerebral perfusion, neurogenesis, and cognitive resilience. Studies have shown that regular aerobic activity not only supports circulation but also increases brain-derived neurotrophic factor (BDNF), which enhances neural plasticity. For those learning how to raise heart rate safely as part of a wellness routine, it’s encouraging to know that doing so contributes to long-term neurological protection. This connection is particularly relevant in the context of aging, where declining circulation can contribute to cognitive decline. Among the overlooked factors that increase heart rate and blood pressure include cognitive stress, alertness demands, and mental workload—all of which can be harnessed strategically to support brain health.
10. Can gut health and microbiome diversity affect heart rate regulation?
Emerging research suggests that the gut-heart axis plays a surprisingly influential role in autonomic regulation and cardiovascular responsiveness. Dysbiosis, or microbial imbalance, has been linked to inflammation and altered vagal tone, both of which impact resting and reactive heart rate. Improving gut health through prebiotics, probiotics, and fiber-rich diets may indirectly influence how to increase heart rate appropriately during activity. Although this area of science is still evolving, there’s a growing recognition that systemic inflammation from poor gut health is among the more complex factors that increase heart rate and blood pressure include endotoxin absorption and altered metabolic signaling. Enhancing microbiome diversity may offer a novel, whole-body strategy to support cardiovascular function from the inside out.
Conclusion: How to Raise Heart Rate Safely While Supporting Lifelong Cardiovascular Health
Improving heart health begins with understanding how to raise heart rate safely and effectively. This is not merely about elevating pulse for its own sake, but about activating the cardiovascular system in ways that promote oxygen delivery, support metabolic function, and increase resilience. Through structured exercise, smart dietary choices, hydration, and attention to stress and lifestyle factors, individuals can stimulate their cardiovascular systems in ways that are both safe and sustainable. Importantly, these strategies work best when personalized to each individual’s age, fitness level, and health history.
The factors that increase heart rate and blood pressure include more than just movement or food—they encompass emotional, hormonal, and environmental dimensions as well. Recognizing this complexity allows for a more holistic, medically sound approach to heart rate management. Whether you’re recovering from illness, managing a chronic condition, or optimizing performance, the key lies in balancing activation with recovery, stimulation with stability.
Ultimately, learning how to increase heart rate should be part of a broader strategy to improve circulation and cardiovascular function over the long term. By following doctor-recommended approaches and listening to the body’s signals, individuals can take charge of their heart health with confidence, clarity, and scientifically supported insight.
heart rate variability improvement, boosting cardiovascular endurance, ways to improve blood circulation, safe cardio workouts, natural circulatory boosters, heart-healthy exercise tips, aerobic fitness benefits, sympathetic nervous system activation, lifestyle tips for heart health, signs of poor circulation, low heart rate causes, thermoregulation and heart function, vagal tone enhancement, autonomic nervous system balance, postural effects on heart rate, healthy blood pressure habits, improving oxygen delivery, cardiovascular conditioning techniques, non-exercise heart stimulation, metabolic impact of heart rate
Further Reading:
How To Boost Your Circulation (And Why It’s Important!)
DisclaimerThe information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.