Blood pressure monitoring has become a cornerstone of preventive cardiovascular care. Whether done in a clinical setting or at home, accurate blood pressure readings play a vital role in diagnosing, managing, and preventing hypertension and other cardiovascular disorders. With the rise of personal health monitoring devices, many individuals now routinely check their own blood pressure—but understanding how to read a BP monitor accurately is just as critical as taking the measurement itself. For those asking, “How do I read a blood pressure monitor?” or “How do you read a blood pressure meter correctly?” this article will serve as a comprehensive guide. It explains not only the practical steps of interpretation but also the physiological significance of each reading, empowering readers to take a proactive role in their heart health.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Understanding the Components of a Blood Pressure Reading
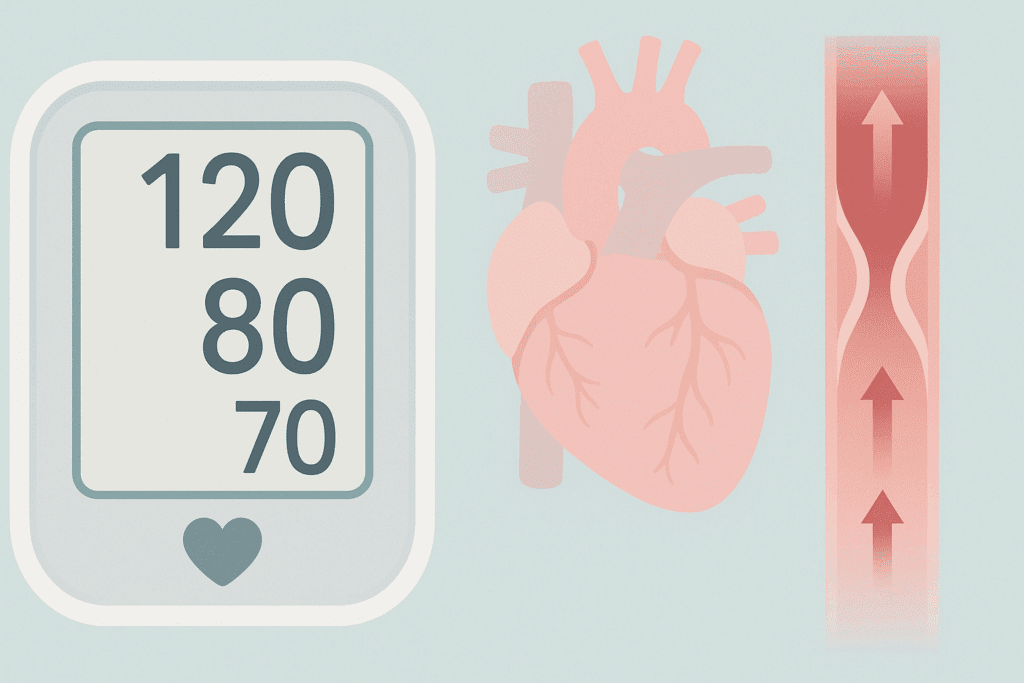
A blood pressure monitor provides two key numbers: systolic and diastolic pressure. The systolic pressure, which appears on top or is listed first, measures the force your heart exerts on arterial walls with each contraction. Diastolic pressure, the bottom number, reflects the force during the heart’s resting phase between beats. These values are expressed in millimeters of mercury (mm Hg) and are fundamental in determining cardiovascular risk.
When learning how to read a BP monitor, it’s essential to grasp the significance of these numbers. A reading of 120/80 mm Hg is considered normal, according to the American Heart Association. Readings consistently above this range may indicate elevated blood pressure or hypertension, whereas significantly lower readings may suggest hypotension. However, isolated readings should not be taken as diagnostic. Context, including age, activity level, and medical history, must be considered.
Moreover, modern blood pressure monitors often include pulse readings, which show how many times your heart beats per minute. While not part of the blood pressure measurement per se, heart rate can provide additional insight into cardiovascular function and overall health.
Types of Blood Pressure Monitors and Their Accuracy
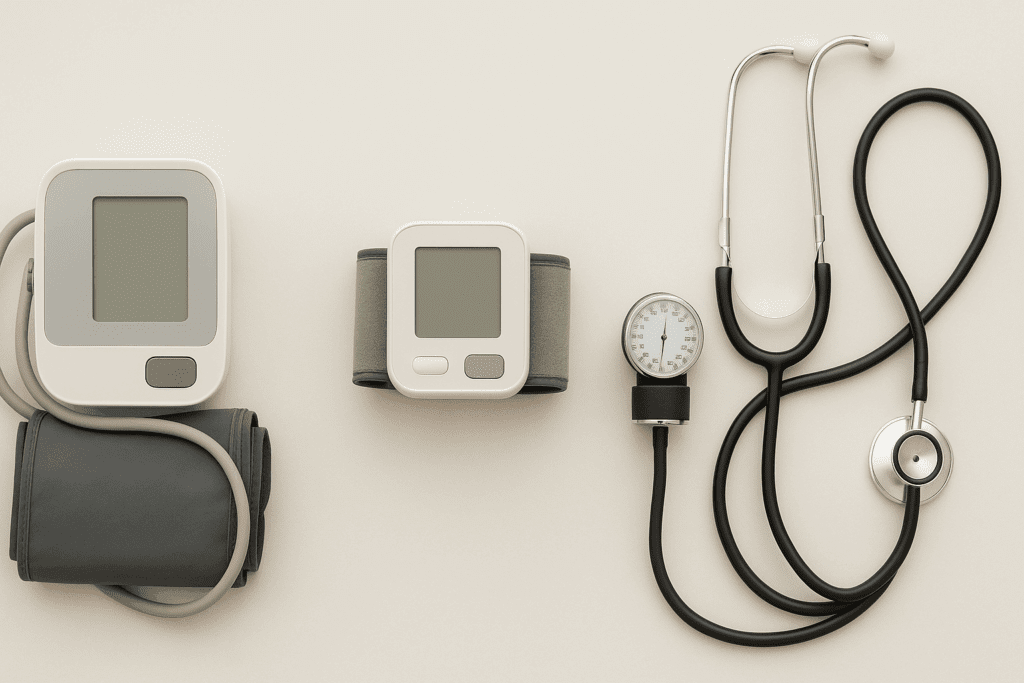
There are several types of blood pressure monitors, each with unique features and varying degrees of accuracy. The most common for home use is the automatic (digital) upper arm cuff monitor. These devices are easy to use and provide quick results, often with additional features such as memory storage, irregular heartbeat detection, and averaging of multiple readings.
Wrist monitors are also available but tend to be more sensitive to body position and movement, potentially leading to less accurate readings if not used properly. Manual monitors with a stethoscope and sphygmomanometer remain the gold standard in clinical settings, requiring professional training for accurate use.
To ensure that the readings are reliable, it’s crucial to use a validated monitor that has been tested for accuracy against clinical standards. Organizations such as the Association for the Advancement of Medical Instrumentation (AAMI) and the British Hypertension Society (BHS) maintain lists of approved devices. Choosing a trustworthy device lays the groundwork for understanding how to read a blood pressure monitor with confidence.

Proper Technique for Measuring Blood Pressure at Home
Accurate readings begin with proper technique. Sit quietly for at least five minutes before taking a reading, with feet flat on the floor and back supported. The arm should be at heart level, supported on a table or armrest, and the cuff must be wrapped snugly around the upper arm, with the lower edge about an inch above the elbow crease.
It’s important not to talk, move, or cross your legs during the measurement. These actions can temporarily raise blood pressure and skew results. Ideally, take two or three readings one minute apart, then average them to get the most accurate picture.
Time of day can also affect blood pressure. Many healthcare professionals recommend measuring in the morning before medications and in the evening before dinner to capture a comprehensive view of daily fluctuations. Consistency in timing, posture, and technique enhances the reliability of home monitoring.
Common Mistakes and How to Avoid Them
One of the most common errors when using a home monitor is incorrect cuff placement. A cuff that’s too loose or placed too low on the arm can result in falsely elevated or reduced readings. Additionally, not sitting in a relaxed position or measuring immediately after physical activity can yield inaccurate results.
Another frequent issue is using a cuff that doesn’t fit properly. Cuffs that are too small may overestimate blood pressure, while oversized cuffs can underestimate it. It’s essential to use the appropriate cuff size for your arm circumference, a detail often overlooked.
Understanding how to read a BP monitor accurately also involves recognizing when readings may be affected by external factors. Stress, caffeine, cold temperatures, and even conversations during measurement can influence the results. By controlling these variables, you can ensure that your blood pressure data reflects your true cardiovascular status.
Interpreting the Readings: What the Numbers Mean
Interpreting blood pressure readings involves more than comparing numbers against standard charts. While general guidelines classify blood pressure as normal, elevated, stage 1 or stage 2 hypertension, and hypertensive crisis, individual circumstances matter. For example, a reading of 135/85 mm Hg might be cause for concern in one individual but acceptable in another with certain comorbidities or age-related adjustments.
It’s also vital to track trends rather than fixate on single readings. Fluctuations from day to day are normal, and occasional spikes can result from temporary factors such as stress or lack of sleep. If you find yourself asking, “How do I read a blood pressure monitor and know if my numbers are dangerous?”—the answer lies in consistent patterns. Keep a log and discuss it with your healthcare provider to determine if treatment or lifestyle changes are necessary.
Furthermore, consider the role of systolic versus diastolic pressure. Elevated systolic readings are a stronger predictor of cardiovascular risk in older adults, whereas diastolic elevation may be more concerning in younger individuals. Understanding these nuances adds depth to the question, “How do you read a blood pressure meter in a way that helps prevent long-term heart issues?”

When to Be Concerned: Recognizing Abnormal Patterns
Persistent readings above 130/80 mm Hg typically suggest hypertension, especially if confirmed across multiple measurements. This condition is often silent, lacking symptoms until complications arise. Thus, knowing how to read a BP monitor regularly can be lifesaving.
On the opposite end, hypotension—defined generally as readings below 90/60 mm Hg—can lead to dizziness, fainting, and risk of falls. In some cases, low blood pressure may indicate underlying endocrine or neurological disorders, dehydration, or medication side effects.
Irregular heartbeats or dramatic swings in blood pressure from one reading to another warrant medical attention. These could be signs of arrhythmias, autonomic dysfunction, or other cardiovascular anomalies. If your monitor detects such issues or you notice dramatic changes, contact your healthcare provider promptly.
Incorporating Blood Pressure Monitoring into Your Health Routine
Monitoring your blood pressure at home offers a valuable window into your cardiovascular health, particularly for individuals with hypertension, diabetes, or chronic kidney disease. Establishing a routine makes it easier to detect changes early and adjust interventions accordingly.
Consistency is key. Choose a regular time each day, use the same arm, and maintain similar conditions to build a reliable data set. Many people find it helpful to create a logbook or use apps connected to Bluetooth-enabled monitors for automatic tracking.
Share your readings with your healthcare provider during routine visits. This collaborative approach helps fine-tune treatment plans and reinforces shared decision-making, a core tenet of patient-centered care. Learning how to read a BP monitor is not just about numbers—it’s about fostering an informed partnership with your care team.
Lifestyle Factors That Influence Blood Pressure
Blood pressure is not a static measurement; it fluctuates with numerous lifestyle variables. Diet, physical activity, stress, alcohol consumption, and sleep quality all play roles in shaping your cardiovascular profile. Recognizing these influences helps contextualize your readings.
A diet high in sodium or processed foods can raise blood pressure, while increased potassium intake—through fruits, vegetables, and legumes—can counteract these effects. Regular aerobic exercise strengthens the heart, enabling it to pump more efficiently and with less effort, which lowers pressure on arterial walls.
Chronic stress, poor sleep, and excessive alcohol or caffeine can elevate blood pressure, sometimes significantly. Awareness of these factors helps you avoid unnecessary alarm when encountering an occasional spike. It also empowers you to make sustainable changes that support long-term heart health.

Technology and the Future of Home Monitoring
As technology advances, blood pressure monitors are becoming smarter, more user-friendly, and increasingly integrated into broader digital health ecosystems. Devices now offer features such as cloud syncing, voice assistance, trend analysis, and real-time alerts for abnormal readings.
These innovations enhance the utility of home monitoring for patients and providers alike. For instance, remote patient monitoring platforms allow clinicians to receive real-time data, enabling faster adjustments to treatment plans. This is particularly beneficial for patients managing chronic conditions or recovering from cardiovascular events.
The growing prevalence of wearable devices also plays a role. Smartwatches with optical sensors can estimate blood pressure, though these are currently less accurate than cuff-based monitors. Nonetheless, they may prompt users to seek formal evaluation, thus acting as valuable screening tools.
How to Talk to Your Doctor About Your Readings
Effective communication with your healthcare provider maximizes the value of home monitoring. Bring your blood pressure log to appointments, and note any lifestyle changes, symptoms, or medication adjustments that may affect your readings.
Ask questions like, “How do I read a blood pressure monitor in a way that complements your clinical evaluation?” or “Do these readings suggest that my treatment needs adjustment?” These conversations deepen your understanding and support collaborative care.
Be prepared to discuss patterns, not just isolated readings. Highlight concerns such as morning spikes, post-exercise dips, or irregular heartbeat notifications from your device. Your doctor can help interpret these nuances within the context of your overall health.
Frequently Asked Questions: How to Read a Blood Pressure Monitor
1. Can emotional stress impact how I read a blood pressure monitor at home?
Yes, emotional stress can significantly alter your blood pressure readings, often causing temporary spikes that may lead to misinterpretation. If you’re wondering how to read a BP monitor under stress, it’s crucial to recognize that anxiety, anger, or nervousness can elevate systolic and diastolic values. To counter this, wait at least 10–15 minutes in a calm, quiet environment before taking a reading. It’s best to document your emotional state alongside the measurement in your log, as this context can help your doctor interpret the numbers more accurately. When considering how do I read a blood pressure monitor during emotionally charged moments, understand that consistency and calm surroundings are key to reliable results.
2. What role does arm positioning play in accurate readings, and how do you read a blood pressure meter correctly because of it?
Arm positioning is one of the most overlooked yet essential factors in accurate home blood pressure monitoring. If your arm is significantly below or above heart level, the reading can be misleading—either too high or too low. For those learning how do you read a blood pressure meter with precision, keeping the cuffed arm supported at heart level is non-negotiable. You might use a pillow or table to maintain this alignment. Misplacement not only affects accuracy but could also falsely indicate hypertension, making correct technique vital for trustworthy readings.
3. Is it normal for blood pressure readings to vary throughout the day, and how do I interpret these fluctuations?
Absolutely, it’s entirely normal for blood pressure to vary depending on the time of day, activity level, hydration, and other factors. If you’re trying to understand how to read a BP monitor accurately across different times, the key is recognizing daily patterns. Typically, blood pressure is lowest during sleep, begins to rise upon waking, and may spike during periods of stress or activity. Instead of worrying about each individual reading, focus on trends over time. Learning how do you read a blood pressure monitor in this context means understanding that context matters as much as the numbers.
4. How do I distinguish between a faulty monitor reading and an actual health concern?
One of the challenges for users learning how to read a BP monitor effectively is determining whether an unusually high or low reading is equipment-related or health-related. Start by retaking the reading after a five-minute rest. If the discrepancy persists across multiple attempts on different days, then it’s worth discussing with your healthcare provider. It’s also wise to calibrate your home monitor annually against a professional device. If you’re asking how do you read a blood pressure meter with confidence, regular maintenance and occasional clinical comparison go a long way in ruling out device errors.
5. Can frequent checking lead to anxiety or skewed results, and how should I manage this?
Frequent monitoring—especially without professional guidance—can sometimes lead to health anxiety, a phenomenon known as “white coat syndrome” even in home settings. If you find yourself obsessively asking how do I read a blood pressure monitor every hour or multiple times a day, consider scaling back. Monitoring once in the morning and once in the evening is generally sufficient unless otherwise advised. Practice mindfulness or relaxation exercises before taking readings to reduce psychological interference. Understanding how to read a BP monitor isn’t just about the numbers—it’s also about creating a healthy routine that encourages emotional balance.
6. What are the long-term benefits of mastering how to read a BP monitor correctly?
Over time, learning how do you read a blood pressure meter with accuracy enables early detection of trends that could signal the onset of cardiovascular issues. This allows for timely interventions through lifestyle changes or medication adjustments, potentially preventing strokes or heart attacks. It also fosters a sense of empowerment, putting you in greater control of your health. People who consistently understand how to read a BP monitor effectively tend to have better adherence to treatment and experience more informed healthcare conversations. Ultimately, this skill supports longevity and quality of life.
7. How can seasonal changes or weather affect my blood pressure readings?
Seasonal variations—especially shifts in temperature—can have a measurable impact on blood pressure. Cold weather causes blood vessels to constrict, which can lead to higher readings, while warmer temperatures may cause slight drops. If you’re wondering how do I read a blood pressure monitor in extreme climates, it’s important to measure in a temperature-controlled environment to avoid misinterpretation. Even humidity levels and barometric pressure changes can subtly influence readings. Understanding how to read a BP monitor means factoring in environmental elements that could skew results unexpectedly.
8. Can caffeine or certain foods affect how I should read a blood pressure monitor reading?
Yes, substances like caffeine, alcohol, and high-sodium meals can temporarily increase blood pressure, leading to potentially misleading readings if taken too soon after consumption. For those asking how do you read a blood pressure meter in light of dietary choices, it’s best to wait at least 30 to 60 minutes after eating or drinking caffeine before checking. Keeping a food diary alongside your blood pressure log can offer additional context for interpretation. If readings fluctuate based on what you eat or drink, that data is valuable for both personal insight and medical consultations.
9. Should I measure blood pressure in both arms, and how do I interpret differences?
It is advisable to check both arms initially to identify if there’s a significant disparity—usually greater than 10 mm Hg—which may suggest vascular abnormalities. If you’re trying to figure out how to read a BP monitor when results differ between arms, consult your physician to determine which arm should be used for ongoing measurements. Once consistency is established, always use the same arm to maintain data integrity. This step is often overlooked but can greatly enhance how do I read a blood pressure monitor for long-term tracking. Not all differences are clinically significant, but large variations should never be ignored.
10. How is emerging technology changing the way we read and understand blood pressure monitors?
Technological advancements are revolutionizing how we approach personal health monitoring, especially for those keen on mastering how to read a BP monitor in real-time. Wearable devices and smart monitors now sync with mobile apps, allowing users to store, compare, and even share their readings with doctors instantly. Machine learning algorithms are beginning to analyze trends and provide predictive insights, offering a glimpse into potential future cardiovascular events. For those wondering how do you read a blood pressure meter in the era of digital health, the answer lies in integration—blending user literacy with technological innovation. As these tools become more sophisticated, they will likely improve early detection, compliance, and overall cardiovascular outcomes.
Conclusion: Taking Charge of Your Cardiovascular Health Through Informed Monitoring
Understanding how to read a BP monitor is a vital skill for anyone invested in their long-term heart health. It transforms a simple device into a powerful tool for early detection, ongoing management, and prevention of cardiovascular complications. By learning how to read a blood pressure monitor accurately and consistently, you gain insight into your circulatory system’s daily function and responsiveness to lifestyle choices, medication, and stress.
If you’ve ever wondered, “How do you read a blood pressure meter in a way that genuinely informs your health decisions?”—the answer lies in context, consistency, and collaboration with your healthcare provider. Home monitoring is not a replacement for professional care, but when done correctly, it enhances your role in the process, making you an active participant in your health journey.
As cardiovascular diseases remain a leading cause of death globally, taking proactive steps like learning how to read a BP monitor could be one of the simplest yet most impactful ways to protect your heart. By fostering a clear understanding of your readings, avoiding common errors, and integrating monitoring into your daily routine, you pave the way for more informed, empowered, and healthier living.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Home Blood Pressure Monitoring


