Introduction
Heart attacks, medically known as myocardial infarctions, remain one of the leading causes of death worldwide. The ability to prevent, recognize, and treat a heart attack promptly can make the difference between life and death. Understanding how to stop a heart attack before it happens is crucial for individuals at risk and their loved ones. This article explores comprehensive strategies to prevent heart attacks, immediate first-aid measures to mitigate damage, and advanced medical treatments available to those who experience a myocardial infarction. With a focus on scientifically backed methods, we aim to provide a thorough, expert-level discussion suitable for those seeking an in-depth understanding of heart attack prevention and treatment.
You may also like: How to Naturally Reverse 20 Years of Arterial Plaque: Science-Backed Strategies for a Healthier Heart

Understanding the Risk Factors for Heart Attacks
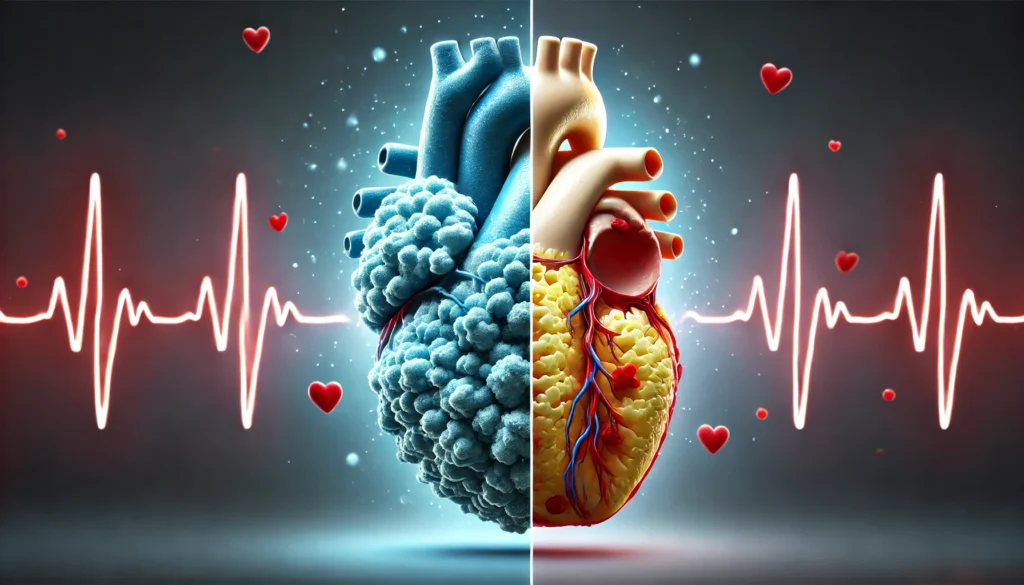
To effectively prevent heart attacks, it is essential to understand their root causes. Several risk factors contribute to the development of coronary artery disease (CAD), which is the primary cause of heart attacks. These factors can be classified into modifiable and non-modifiable categories.
Non-modifiable risk factors include age, gender, and genetics. As people age, their risk of myocardial infarction increases. Men are generally at a higher risk than women, although postmenopausal women see a rise in heart attack incidents. A family history of heart disease also significantly raises the likelihood of experiencing a cardiac event.
Modifiable risk factors, on the other hand, are those that individuals can control to reduce their heart attack risk. These include hypertension, high cholesterol levels, obesity, smoking, diabetes, and sedentary lifestyles. Making specific lifestyle changes can drastically decrease the probability of developing coronary artery disease and experiencing a heart attack.
How to Stop a Heart Attack from Happening: Lifestyle and Dietary Changes
One of the most effective ways to prevent a heart attack is by adopting a heart-healthy lifestyle. This includes maintaining a balanced diet, engaging in regular exercise, managing stress, and avoiding harmful substances.
A diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce cholesterol levels and lower blood pressure. The Mediterranean diet, for example, has been widely recommended by cardiologists for its ability to promote heart health. This diet emphasizes the consumption of healthy fats, such as those found in olive oil, nuts, and fish, while minimizing processed foods, refined sugars, and unhealthy trans fats.
Regular physical activity plays a critical role in cardiovascular health. Engaging in at least 150 minutes of moderate-intensity exercise per week can help maintain a healthy weight, improve circulation, and reduce stress. Activities such as brisk walking, cycling, and swimming are excellent choices for promoting cardiovascular fitness.
Managing stress is another crucial factor in preventing heart attacks. Chronic stress contributes to high blood pressure and inflammation, both of which increase heart attack risk. Practices such as meditation, deep breathing exercises, and engaging in hobbies can help individuals manage stress effectively.
What Prescribed First Aid for Heart Attack Should You Know?
If a heart attack occurs, immediate intervention is critical in minimizing damage to the heart muscle. The first step is to recognize the symptoms, which may include chest pain, shortness of breath, nausea, dizziness, and pain radiating to the arm, jaw, or back.
When someone experiences a heart attack, calling emergency medical services (EMS) should be the top priority. While waiting for medical professionals to arrive, providing first aid can be life-saving. Aspirin is often recommended as an initial treatment because it helps thin the blood and prevent further clot formation. Chewing an aspirin (typically 325 mg) can improve survival chances.
If the person is conscious and able to follow instructions, sitting in a comfortable position and taking slow, deep breaths can help reduce strain on the heart. If unconscious, cardiopulmonary resuscitation (CPR) should be administered if the person is not breathing or has no pulse. Chest compressions should be performed at a rate of 100-120 compressions per minute to maintain blood circulation until professional help arrives.

Can You Stop a Heart Attack? Emergency Medical Treatments
While first-aid measures are critical, professional medical treatment is essential for stopping a heart attack. Once at the hospital, doctors will administer immediate interventions to restore blood flow to the heart. The most common treatments include thrombolytic therapy, percutaneous coronary intervention (PCI), and coronary artery bypass grafting (CABG).
Thrombolytic therapy involves the use of clot-dissolving drugs, such as tissue plasminogen activators (tPA), which help restore blood flow in blocked arteries. This treatment is most effective when administered within the first few hours of a heart attack.
Percutaneous coronary intervention (PCI), commonly known as angioplasty, is a procedure in which a catheter with a small balloon is inserted into the blocked artery. The balloon is then inflated to open the artery, and a stent may be placed to keep it open. PCI is often the preferred treatment for heart attacks because it provides immediate relief and reduces the risk of future cardiac events.
For individuals with severe coronary artery disease, coronary artery bypass grafting (CABG) may be necessary. This surgical procedure involves grafting a healthy blood vessel from another part of the body to bypass the blocked artery and restore proper blood flow to the heart.
How to Save Yourself from a Heart Attack: Long-Term Management and Prevention
Surviving a heart attack is not the end of the journey; it marks the beginning of long-term management and prevention. Patients who have experienced a myocardial infarction must adhere to lifestyle changes, take prescribed medications, and undergo regular medical evaluations to reduce the risk of future heart attacks.
Medications such as beta-blockers, ACE inhibitors, statins, and antiplatelet drugs are commonly prescribed to heart attack survivors. These medications help control blood pressure, reduce cholesterol levels, and prevent further clot formation.
Cardiac rehabilitation programs provide structured support for individuals recovering from a heart attack. These programs include supervised exercise, dietary counseling, stress management, and education on heart-healthy living. Participation in cardiac rehabilitation has been shown to improve survival rates and quality of life for heart attack survivors.
Frequently Asked Questions (FAQ) on Preventing and Treating Heart Attacks
1. Can you stop a heart attack from happening by making lifestyle changes?
Yes, adopting heart-healthy habits can significantly reduce the likelihood of experiencing a heart attack. Regular physical activity, a diet rich in fruits, vegetables, and lean proteins, and maintaining a healthy weight all contribute to improved cardiovascular health. Avoiding smoking and limiting alcohol consumption can also lower the risk of coronary artery disease, a primary cause of heart attacks. Additionally, managing stress through mindfulness techniques, meditation, and adequate sleep helps regulate blood pressure and reduces overall cardiac strain. While these changes cannot completely eliminate the possibility of a heart attack, they can substantially decrease the risk and enhance overall heart function.
2. What do doctors do for a heart attack once a patient arrives at the hospital?
Emergency medical personnel begin heart attack treatment the moment a patient arrives by stabilizing vital signs and administering medications such as aspirin, nitroglycerin, and blood thinners. If necessary, a myocardial infarction medical procedure like percutaneous coronary intervention (PCI) is performed to reopen blocked arteries. In cases where PCI is not an option, thrombolytic drugs may be used to dissolve the clot. Cardiac monitoring continues throughout the process to detect any arrhythmias or complications that may arise. Following the immediate emergency response, long-term treatment plans involving medication and lifestyle changes are developed to prevent future heart attacks.
3. How to stop a heart attack in 30 seconds—Is it possible?
Contrary to some myths, there is no scientifically proven method to stop a heart attack in 30 seconds. However, recognizing early warning signs and acting quickly can make a life-or-death difference. If symptoms such as chest pain, shortness of breath, or dizziness occur, immediately chewing aspirin and calling emergency services are the most effective steps. Staying calm and avoiding physical exertion can also prevent further strain on the heart. While certain techniques, like coughing or drinking water, have been circulated as potential emergency measures, they are not substitutes for professional medical intervention. Rapid response and proper medical treatment remain the best ways to minimize heart damage.
4. What prescribed first aid for heart attack should everyone know?
Recognizing the symptoms early and taking immediate action is crucial. If someone experiences severe chest pain, call emergency medical services right away. Providing aspirin (typically 325 mg) helps thin the blood and prevent further clot formation. Keeping the individual calm, seated, and avoiding unnecessary movement can reduce the strain on the heart. If they become unresponsive, performing CPR while awaiting medical assistance can improve survival chances. Using an automated external defibrillator (AED) in cases of cardiac arrest can also be life-saving, making first aid knowledge essential for everyone.
5. Can you stop a heart attack from happening by taking medication?
Yes, medications play a crucial role in preventing heart attacks, especially for those with existing heart conditions. Statins help lower cholesterol, beta-blockers reduce blood pressure and heart rate, and antiplatelet drugs prevent clot formation. In some cases, doctors prescribe anticoagulants to reduce the risk of clotting in high-risk patients. While these medications can significantly lower the chances of a heart attack, they work best when combined with lifestyle modifications such as a healthy diet and regular exercise. Regular medical check-ups ensure that the prescribed heart attack medical treatment remains effective and adjusted as needed.
6. How do myocardial infarction treatments vary depending on the severity of the heart attack?
The treatment of a myocardial infarction depends on its severity and type. For a mild heart attack with partial artery blockage, doctors may manage it with medications such as blood thinners and lifestyle modifications. More severe cases require urgent interventions like percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) to restore blood flow. If a heart attack is caused by a completely blocked artery, immediate medical procedures are necessary to prevent extensive heart damage. Long-term cardiac rehabilitation, including exercise programs and dietary adjustments, ensures continued recovery and prevention of future episodes.
7. How to save yourself from a heart attack when alone?
If you suspect you are having a heart attack while alone, immediately call emergency services and alert someone nearby if possible. Chewing aspirin can slow clot formation and improve blood flow. If prescribed, taking nitroglycerin can help alleviate chest pain by widening blood vessels. Try to remain calm, avoid exertion, and sit in a comfortable position while waiting for emergency responders. While techniques such as deep coughing have been suggested as ways to treat a heart attack, they are not scientifically proven and should not replace professional medical assistance.
8. What are the latest advancements in myocardial infarction medical procedures?
Advancements in myocardial infarction medical procedures have significantly improved survival rates and recovery times. Minimally invasive techniques such as transradial catheterization allow stents to be placed through a wrist artery, reducing complications and speeding up recovery. Robotic-assisted heart surgeries provide greater precision in procedures like coronary artery bypass grafting (CABG). Research is also advancing in regenerative medicine, where stem cell therapy aims to repair heart tissue damaged by myocardial infarctions. Additionally, wearable technology and artificial intelligence-driven diagnostics are helping doctors detect early warning signs before a heart attack occurs, enabling more proactive treatment.
9. How to treat a heart attack effectively in the golden hour?
The first 60 minutes after a heart attack, known as the “golden hour,” are critical for preventing long-term heart damage and improving survival chances. Immediate administration of aspirin, oxygen therapy, and nitroglycerin can reduce the impact of the attack. Emergency responders often perform an electrocardiogram (ECG) to diagnose the severity and initiate the appropriate heart attack medical treatment. For complete artery blockages, percutaneous coronary intervention (PCI) or thrombolytic therapy is crucial in restoring blood flow quickly. Ensuring quick access to a hospital with specialized cardiac care can make a life-saving difference in these situations.
10. How to stop a heart attack before it happens using emerging prevention methods?
New research is continually identifying advanced ways to prevent heart attacks before they occur. Genetic testing now allows for early detection of hereditary heart disease risks, enabling personalized prevention plans. Smartwatches and wearable ECG monitors provide real-time heart rate tracking and early detection of arrhythmias, which can lead to cardiac events. Novel medications, including PCSK9 inhibitors, are showing promise in dramatically lowering cholesterol levels beyond traditional statins. Studies also suggest that anti-inflammatory drugs like colchicine may reduce heart attack risk by controlling chronic inflammation in blood vessels. Combining these emerging technologies with lifestyle modifications enhances prevention strategies, ensuring a proactive approach to cardiovascular health.
Conclusion
Preventing and managing heart attacks requires a comprehensive approach that includes lifestyle modifications, first-aid knowledge, and medical treatments. By understanding the risk factors and making proactive changes, individuals can significantly reduce their chances of experiencing a heart attack. Recognizing the symptoms and taking immediate action during an emergency can save lives. Additionally, long-term management through medication, rehabilitation, and lifestyle changes is essential for heart attack survivors. Through continued education and adherence to heart-healthy practices, we can work towards reducing the global burden of heart disease and improving cardiovascular health for future generations.
heart disease prevention, cardiac emergency response, heart attack warning signs, cardiovascular health tips, reducing heart attack risk, emergency heart care, recognizing heart attack symptoms, heart disease management, CPR for heart attacks, cardiac rehabilitation programs, arterial blockage treatment, cholesterol and heart health, lifestyle changes for heart health, heart attack survival strategies, first aid for cardiac arrest, stress and heart disease, diet for heart health, exercise for heart disease prevention, blood pressure control strategies, advanced cardiac treatments
Further Reading:
How to spot and treat a heart attack
Lifestyle Changes to Prevent a Heart Attack
Heart Attack First Aid: Essential Steps Everyone Should Know
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.