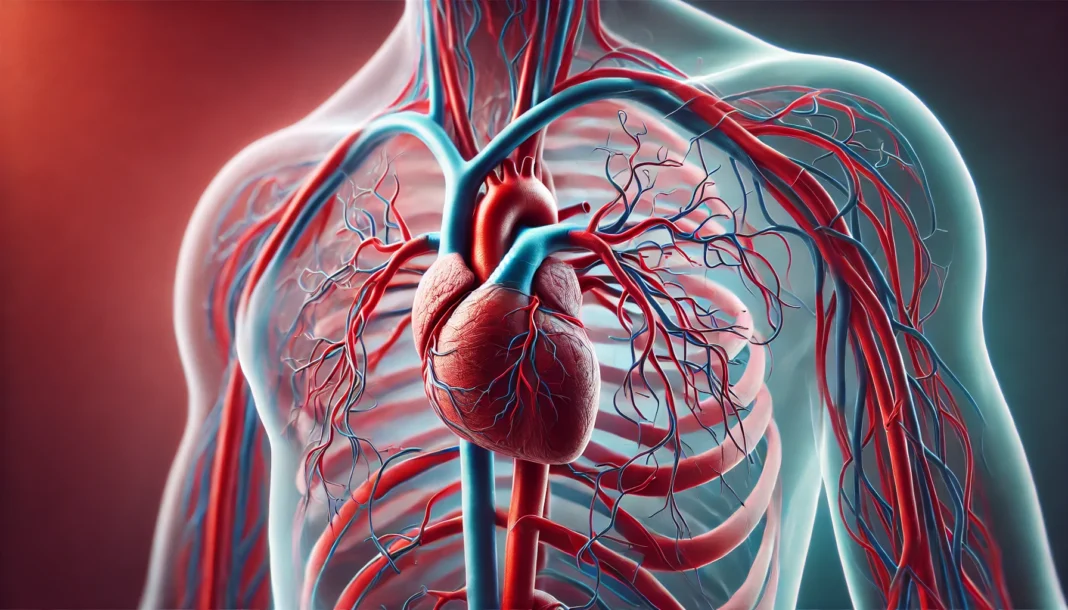
The cardiovascular system is one of the most complex and essential networks in the human body, responsible for sustaining life by facilitating the circulation of oxygenated and deoxygenated blood. Central to this intricate system are the arteries, which serve as conduits for blood to travel from the heart to various organs and tissues. Understanding the function of arteries, the relationship between heart arteries and veins, and the structure of heart vessels provides crucial insight into cardiovascular health and disease prevention. This article explores the anatomy, function, and importance of arteries, offering a comprehensive look into the role they play in circulation and overall health.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
Understanding the Role of Arteries in Circulation
To appreciate how arteries function, it is essential first to understand the overall circulatory system. The human body relies on a continuous flow of blood to transport oxygen, nutrients, and hormones to cells while simultaneously removing waste products like carbon dioxide and metabolic byproducts. Arteries are responsible for carrying oxygen-rich blood away from the heart and distributing it to tissues throughout the body. Unlike veins, which return deoxygenated blood to the heart, arteries are equipped with thick, muscular walls that withstand high-pressure blood flow generated by the heart’s contractions.
The primary function of arteries is to ensure the efficient delivery of oxygenated blood to meet the metabolic demands of organs and tissues. This process is critical for maintaining cellular function, energy production, and overall physiological balance. Any disruption in arterial function, such as blockages or narrowing, can lead to severe health conditions, including heart attacks, strokes, and peripheral artery disease.
Anatomy of Arteries: Structure and Composition
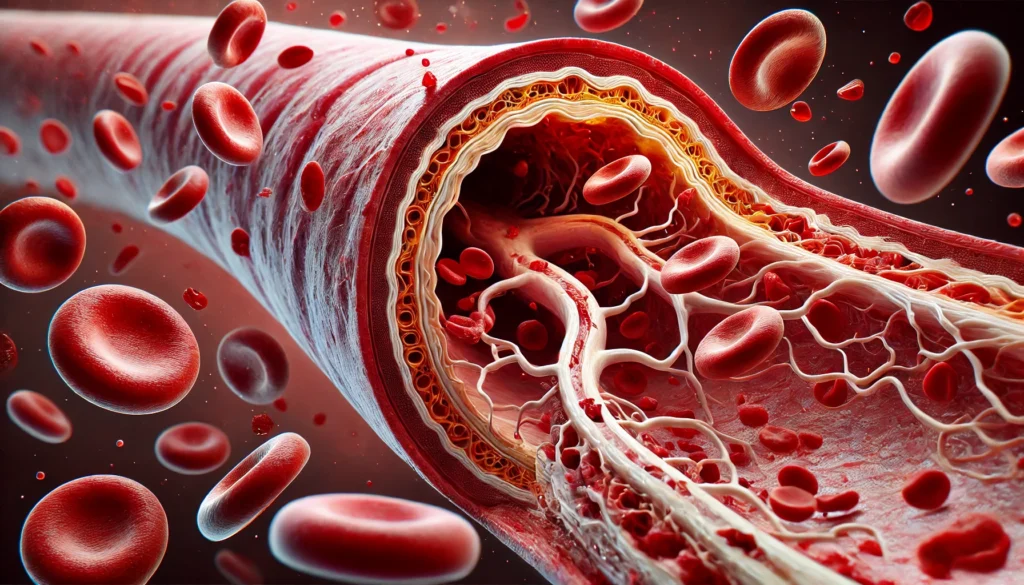
Arteries are composed of three primary layers that contribute to their strength, flexibility, and ability to regulate blood flow. The innermost layer, known as the tunica intima, is lined with endothelial cells that create a smooth surface to reduce friction and promote unobstructed blood movement. The middle layer, or tunica media, consists of smooth muscle and elastic fibers that allow arteries to expand and contract in response to blood pressure changes. This elasticity is crucial for maintaining consistent blood pressure and ensuring adequate circulation. The outermost layer, the tunica externa, provides structural support and protection against external forces that could damage the artery.
Different types of arteries serve specific functions within the circulatory system. Elastic arteries, such as the aorta, contain a high proportion of elastic fibers that enable them to absorb the pressure exerted by the heart’s pumping action. Muscular arteries, including the femoral and radial arteries, have a greater concentration of smooth muscle, allowing for precise regulation of blood flow to specific regions of the body. Arterioles, the smallest branches of arteries, play a crucial role in controlling blood distribution and pressure by adjusting their diameter in response to physiological demands.
The Main Arteries in the Body and Their Functions
The human body contains several major arteries that facilitate blood circulation to essential organs and tissues. The aorta, the largest and most important artery, originates from the left ventricle of the heart and distributes oxygenated blood to systemic circulation. Branching from the aorta are the carotid arteries, which supply blood to the brain and head, and the subclavian arteries, which deliver blood to the arms and upper body.
The coronary arteries are vital for cardiac function, providing oxygen and nutrients to the heart muscle itself. Any obstruction in these arteries can result in coronary artery disease, leading to angina or myocardial infarction. The renal arteries supply blood to the kidneys, playing a crucial role in filtering waste and regulating blood pressure. The iliac and femoral arteries ensure blood flow to the lower extremities, while the pulmonary arteries transport deoxygenated blood from the heart to the lungs for oxygenation.
How Arteries Facilitate Oxygen Transport and Circulation
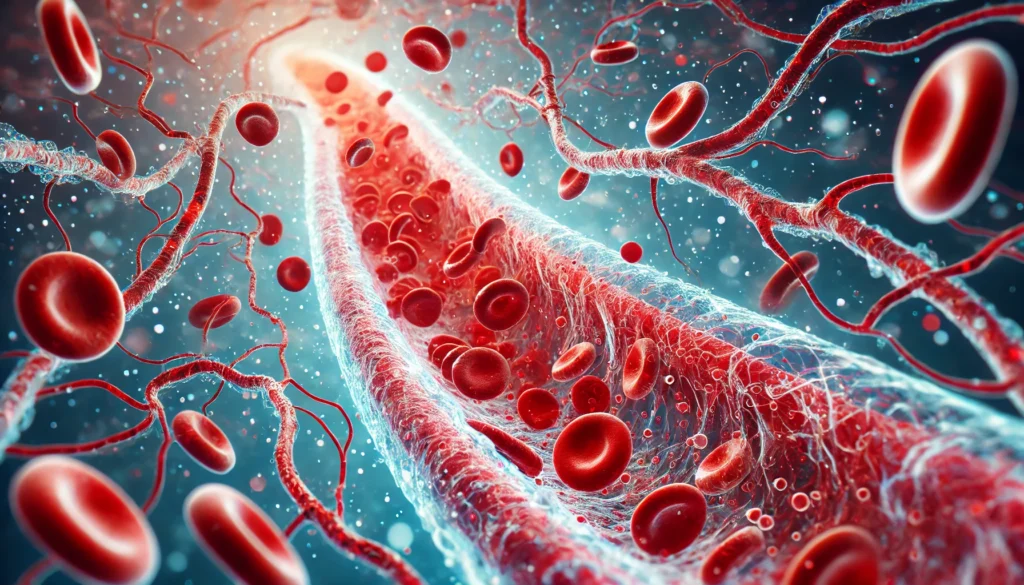
Arteries function as the primary transport system for oxygenated blood, ensuring that each organ receives the necessary nutrients for optimal function. The heart generates the force needed to propel blood through the arterial network, with the aorta serving as the main highway for distribution. As blood travels through progressively smaller arteries and arterioles, pressure decreases, and velocity slows, allowing for effective gas exchange at the capillary level.
One of the most critical aspects of arterial function is vasodilation and vasoconstriction, which regulate blood flow based on physiological needs. During physical activity, for example, arteries expand to accommodate increased blood flow to muscles, while during rest, they constrict to maintain optimal circulation. The ability of arteries to adjust their diameter ensures that blood pressure remains stable and that tissues receive adequate perfusion under various conditions.
The Impact of Arterial Health on Overall Well-being
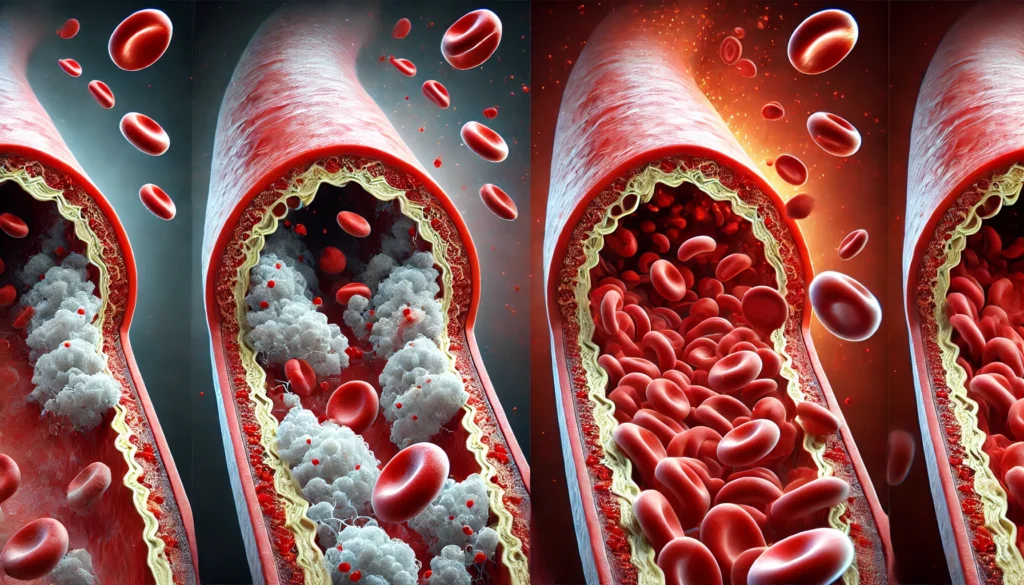
Maintaining healthy arteries is essential for preventing cardiovascular diseases and promoting longevity. Atherosclerosis, a condition characterized by the buildup of plaque within arterial walls, is one of the leading causes of heart attacks and strokes. Plaque consists of cholesterol, fatty deposits, and inflammatory cells that narrow arteries, restricting blood flow and increasing the risk of clot formation.
Several lifestyle factors influence arterial health, including diet, physical activity, and smoking. A diet rich in fruits, vegetables, whole grains, and lean proteins supports arterial function by reducing inflammation and preventing cholesterol buildup. Regular exercise enhances circulation, strengthens arterial walls, and promotes the production of nitric oxide, a molecule that aids in vasodilation. Conversely, smoking damages endothelial cells, accelerates plaque accumulation, and contributes to arterial stiffness, significantly increasing the risk of cardiovascular disease.
The Relationship Between Arteries, Veins, and Capillaries
Arteries, veins, and capillaries work together to maintain an efficient circulatory system. While arteries transport oxygenated blood away from the heart, veins return deoxygenated blood back to the heart for reoxygenation. Capillaries, the smallest blood vessels, serve as intermediaries between arteries and veins, facilitating the exchange of oxygen, nutrients, and waste products between blood and tissues.
Veins contain valves that prevent backflow and ensure unidirectional blood movement toward the heart. Unlike arteries, which rely on the heart’s pumping force, veins depend on skeletal muscle contractions and respiratory movements to propel blood upward against gravity. This intricate network ensures continuous circulation and prevents complications such as deep vein thrombosis and varicose veins.
Recognizing the Signs of Arterial Disease and Seeking Treatment
Early detection of arterial disease is crucial for preventing severe complications. Common symptoms of arterial blockages include chest pain, shortness of breath, leg pain, and dizziness. In cases of peripheral artery disease, individuals may experience numbness or weakness in the legs, indicating reduced blood flow to the extremities.
Medical interventions for arterial disease range from lifestyle modifications to surgical procedures. Medications such as statins and antihypertensives help manage cholesterol levels and blood pressure, reducing the risk of plaque buildup. In severe cases, angioplasty and stent placement restore arterial patency, while bypass surgery creates alternate pathways for blood flow.
Frequently Asked Questions (FAQ) About Arteries and Circulation
1. How do arteries function differently from veins and capillaries?
Arteries function as high-pressure blood vessels that carry oxygen-rich blood away from the heart to various organs and tissues. They have thick, muscular walls that allow them to expand and contract in response to the force of blood being pumped by the heart. In contrast, veins carry deoxygenated blood back to the heart and contain valves to prevent backflow due to lower pressure. Capillaries serve as the intermediary network between arteries and veins, facilitating the exchange of oxygen, nutrients, and waste products between blood and tissues. This intricate relationship between arteries, veins, and capillaries ensures efficient circulation and oxygen delivery throughout the body.
2. Why is arterial elasticity important for maintaining cardiovascular health?
The elasticity of arteries plays a crucial role in regulating blood pressure and ensuring consistent circulation. When the heart pumps blood, elastic arteries such as the aorta expand to accommodate the surge in blood flow and then recoil to maintain pressure when the heart relaxes. If arteries lose elasticity due to conditions like atherosclerosis, the heart must work harder to pump blood, leading to hypertension and increased cardiovascular risk. Healthy arterial function depends on maintaining flexibility through a balanced diet, regular exercise, and avoiding habits that damage the artery body, such as smoking. Maintaining arterial elasticity is key to preventing conditions like stroke, heart attack, and peripheral artery disease.
3. What factors contribute to artery blockage and reduced blood flow?
Several factors contribute to artery blockage, leading to restricted blood flow and potential cardiovascular complications. Atherosclerosis, the buildup of fatty plaques within the artery walls, is a primary cause. High cholesterol levels, excessive intake of saturated fats, and chronic inflammation accelerate plaque formation. Other contributing factors include high blood pressure, smoking, diabetes, and genetic predisposition. When arteries become narrowed or blocked, blood vessels that carry blood to the heart may struggle to supply enough oxygen, increasing the risk of angina or myocardial infarction. Managing these risk factors through a heart-healthy lifestyle can significantly reduce the likelihood of arterial blockages.
4. How do the main arteries in the body support systemic circulation?
The main arteries in the body play a pivotal role in distributing oxygenated blood to various regions. The aorta, the largest artery, branches into major arteries such as the carotid arteries, which supply blood to the brain, and the subclavian arteries, which supply the arms. The coronary arteries ensure that the heart muscle receives adequate blood supply, while the renal arteries support kidney function. The femoral and iliac arteries deliver blood to the lower extremities, ensuring mobility and tissue nourishment. Each important artery within this network is essential for sustaining vital functions and preventing tissue damage due to inadequate blood supply.
5. How does physical activity improve arterial health?
Regular physical activity strengthens heart function and promotes arterial health by enhancing blood vessel flexibility and reducing the risk of arterial stiffness. Exercise increases nitric oxide production, a molecule that helps arteries dilate and maintain smooth blood flow. Activities like aerobic exercise, strength training, and stretching improve circulation by increasing blood vessel efficiency and reducing plaque buildup. Sedentary lifestyles contribute to sluggish blood circulation and arterial hardening, increasing the risk of cardiovascular diseases. Engaging in at least 150 minutes of moderate exercise per week can significantly benefit the overall function of arteries, veins, and capillaries.
6. What are the warning signs of an arterial disorder?
Recognizing the early symptoms of arterial disease is crucial for preventing serious cardiovascular complications. Symptoms such as chest pain, shortness of breath, fatigue, and numbness in the limbs may indicate restricted blood flow. Peripheral artery disease often presents with leg pain, cramping, and difficulty walking due to insufficient circulation in the lower extremities. In severe cases, skin discoloration or non-healing wounds may signal advanced arterial blockages. If you experience any of these symptoms, seeking medical evaluation is essential for diagnosing conditions affecting the heart vessels and determining appropriate treatment options.
7. How do arteries respond to changes in blood pressure?
Arteries function by dynamically adjusting their diameter to accommodate fluctuations in blood pressure and maintain stable circulation. When blood pressure rises, arteries constrict to regulate flow and prevent excessive force on vessel walls. Conversely, when blood pressure drops, arteries dilate to allow increased blood volume to reach essential organs. Chronic high blood pressure can damage artery walls, making them prone to plaque accumulation and increasing the risk of cardiovascular disease. Lifestyle modifications, such as reducing sodium intake and managing stress, help support optimal artery function and blood vessel health.
8. Why is the diagram of the arteries useful for medical diagnosis?
A diagram of the arteries provides a visual representation of how blood flows throughout the body, aiding in medical diagnosis and treatment planning. Physicians use arterial diagrams to locate blockages, assess blood flow efficiency, and determine areas at risk for reduced circulation. Imaging techniques such as angiography and Doppler ultrasound help create detailed maps of arteries labeled with potential obstructions or abnormalities. These diagnostic tools allow healthcare providers to recommend targeted interventions, such as lifestyle modifications, medications, or surgical procedures, to restore healthy blood circulation. Understanding arterial structure through diagrams is crucial for both medical professionals and individuals seeking to improve their cardiovascular health.
9. How does diet influence the function of arteries?
Diet plays a significant role in maintaining arterial health by influencing cholesterol levels, inflammation, and blood pressure regulation. Foods high in fiber, antioxidants, and healthy fats, such as fruits, vegetables, nuts, and fish, help prevent plaque buildup and reduce arterial inflammation. On the other hand, excessive consumption of processed foods, trans fats, and refined sugars contributes to arterial stiffness and increased cardiovascular risk. Omega-3 fatty acids, found in fatty fish and flaxseeds, promote arterial flexibility and reduce clot formation. Maintaining a balanced diet rich in heart-friendly nutrients is essential for sustaining the function of arteries and preventing cardiovascular complications.
10. What are the long-term effects of arterial disease if left untreated?
If arterial disease is left untreated, it can lead to severe and potentially life-threatening complications. Chronic arterial blockages can result in ischemia, a condition where tissues receive insufficient oxygen, leading to organ damage or failure. Coronary artery disease may progress to heart attacks, while cerebrovascular disease can increase the risk of strokes. Peripheral artery disease can cause ulcers, gangrene, and mobility issues due to restricted blood flow in the limbs. Over time, untreated arterial dysfunction can reduce overall quality of life and significantly shorten life expectancy. Early intervention through medical treatment and lifestyle changes is essential for preventing the progression of arterial disease and preserving cardiovascular health.
Conclusion: Preserving Arterial Health for a Strong Cardiovascular System
Understanding how arteries function is fundamental to maintaining cardiovascular health and preventing disease. The intricate network of heart arteries and veins, along with the regulatory mechanisms that govern blood flow, highlights the importance of arterial integrity. By adopting a heart-healthy lifestyle, individuals can protect their arteries from damage, reduce the risk of cardiovascular complications, and ensure optimal circulation throughout life. As research continues to advance, new insights into arterial health will further enhance our ability to diagnose, treat, and prevent cardiovascular conditions, promoting longevity and overall well-being.
circulatory system health, cardiovascular wellness, blood circulation improvement, heart and vascular health, oxygenated blood flow, arterial blood supply, vascular anatomy, healthy blood flow, cardiovascular disease prevention, maintaining arterial elasticity, blood vessel structure, improving circulation naturally, reducing arterial plaque, heart health strategies, blood pressure regulation, arterial health tips, vascular disease awareness, healthy cardiovascular function, lifestyle for heart health, preventing clogged arteries
Further Reading:
Heart Anatomy, Function, and Blood Circulation
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.