Understanding Hypertension and Its Widespread Impact
Hypertension Prevention, more commonly referred to as high blood pressure, is one of the most pervasive chronic conditions affecting global public health. It is a silent yet potent contributor to cardiovascular morbidity and mortality, often progressing without noticeable symptoms until significant damage has occurred. The condition arises when the force of blood against artery walls remains consistently elevated, placing stress on the cardiovascular system and increasing the risk for serious complications such as stroke, heart attack, and kidney failure. Despite being preventable in many cases, hypertension remains a leading cause of premature death worldwide, underscoring the urgent need for robust public awareness, primary prevention strategies, and personalized safety considerations for hypertension management.
In recent years, the medical community has emphasized a shift toward hypertension primary prevention as a critical component of long-term cardiovascular health. By identifying at-risk populations and intervening before blood pressure reaches pathological levels, healthcare providers can drastically reduce the overall burden of disease. This proactive approach is especially vital considering the socioeconomic disparities in hypertension prevalence, which often mirror gaps in access to preventive healthcare and education. Understanding the root causes and risk factors of hypertension is the first step in crafting effective, individualized prevention plans.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Key Risk Factors in the Development of Hypertension
Hypertension does not arise in isolation but is influenced by a complex interplay of genetic, behavioral, and environmental factors. Age, family history, and ethnicity can all predispose individuals to higher baseline blood pressure levels, but lifestyle choices often act as the tipping point. Diets high in sodium and saturated fats, physical inactivity, chronic stress, and excessive alcohol consumption are among the most modifiable risk factors contributing to the development of hypertension. Additionally, comorbid conditions such as diabetes, obesity, and metabolic syndrome further elevate risk, often creating a cycle of worsening cardiovascular health.
Identifying these risk factors early is essential for effective hypertension prevention. Regular blood pressure monitoring, even in individuals without a formal diagnosis, can reveal subtle upward trends that warrant lifestyle intervention. For healthcare providers, integrating screenings into routine primary care visits offers a valuable opportunity to educate patients and establish a baseline for future comparison. In doing so, practitioners support a culture of prevention that empowers individuals to take charge of their cardiovascular well-being before irreversible damage occurs.
The Importance of Hypertension Primary Prevention
Hypertension primary prevention is not merely a concept—it is a clinical imperative. This strategy focuses on preventing the onset of elevated blood pressure in individuals who are currently normotensive but may be at heightened risk due to genetic or lifestyle-related factors. The rationale is grounded in the well-documented progression of hypertension; what begins as a slight elevation often advances into a chronic, difficult-to-manage condition that can precipitate a cascade of vascular complications.
Primary prevention hinges on early identification of risk factors and timely implementation of interventions such as dietary modification, increased physical activity, weight management, and stress reduction. These efforts are supported by a growing body of clinical evidence demonstrating their efficacy in delaying or even averting the need for pharmacologic treatment. Moreover, primary prevention strategies are cost-effective and sustainable, offering long-term benefits not only to individuals but also to healthcare systems struggling with the economic burden of chronic disease management.

Dietary Strategies for Hypertension Prevention
One of the cornerstones of hypertension prevention lies in dietary modification. The Dietary Approaches to Stop Hypertension (DASH) diet has gained widespread recognition for its ability to lower blood pressure through the consumption of nutrient-dense foods rich in potassium, magnesium, and calcium. This eating plan emphasizes fruits, vegetables, whole grains, lean proteins, and low-fat dairy while limiting sodium, red meat, and added sugars. Clinical trials have consistently shown that adherence to the DASH diet can result in significant reductions in both systolic and diastolic blood pressure, particularly among individuals with prehypertension or high-normal readings.
Beyond DASH, broader principles of heart-healthy eating—such as reducing processed food intake, avoiding trans fats, and incorporating plant-based meals—can support hypertension primary prevention. Importantly, these dietary shifts should be framed as sustainable lifestyle changes rather than temporary fixes. Educational interventions, including nutritional counseling and cooking workshops, can enhance adherence and empower individuals to make informed choices in various food environments.

The Role of Physical Activity in Cardiovascular Health
Physical activity is another foundational pillar of hypertension prevention. Regular aerobic exercise has been shown to improve vascular function, enhance insulin sensitivity, and promote weight loss—all of which contribute to lower blood pressure. The American Heart Association recommends at least 150 minutes of moderate-intensity exercise per week, such as brisk walking, swimming, or cycling, to maintain cardiovascular health. Even modest increases in physical activity among sedentary individuals can yield measurable benefits.
Incorporating exercise into daily routines does not require a gym membership or elaborate equipment. Simple strategies like walking during lunch breaks, taking the stairs instead of the elevator, or engaging in home-based workouts can have a cumulative effect. Community initiatives, including workplace wellness programs and public fitness campaigns, also play a pivotal role in promoting an active lifestyle. By making physical activity accessible and enjoyable, these efforts can facilitate long-term adherence and reduce the population-wide incidence of hypertension.
Weight Management as a Preventive Strategy
Obesity is one of the most potent risk factors for hypertension, with excess adiposity contributing to increased blood volume, vascular resistance, and sympathetic nervous system activation. As such, weight management is a central component of hypertension prevention and control. Studies have shown that even modest weight loss—on the order of 5 to 10 percent of body weight—can produce clinically significant reductions in blood pressure.
Effective weight management requires a multi-pronged approach that includes dietary changes, increased physical activity, and behavioral support. Cognitive-behavioral therapy, for example, can help individuals identify emotional eating triggers and develop healthier coping mechanisms. Additionally, weight loss interventions should be tailored to individual needs, accounting for factors such as cultural preferences, socioeconomic constraints, and comorbid conditions. A personalized and compassionate approach increases the likelihood of success and reinforces the message that hypertension prevention is both achievable and worthwhile.

Stress Reduction and Its Influence on Blood Pressure
Chronic psychological stress is a frequently overlooked contributor to hypertension. The body’s stress response—marked by the release of cortisol and adrenaline—can lead to temporary spikes in blood pressure. When this response becomes chronic, it may result in sustained vascular constriction and hypertension. Techniques such as mindfulness meditation, deep breathing, progressive muscle relaxation, and yoga have been shown to reduce stress levels and improve overall cardiovascular health.
Integrating stress management into daily routines can be challenging, particularly for individuals juggling multiple responsibilities. However, even brief moments of intentional relaxation can yield benefits. Employers and community organizations can support these efforts by offering mental health resources, promoting work-life balance, and creating spaces for stress relief. By acknowledging and addressing the psychosocial dimensions of hypertension prevention, healthcare providers can offer more holistic and effective care.
Safety Considerations for Hypertension Prevention and Lifestyle Changes
While lifestyle modification is generally safe and beneficial, certain hypertension precautions are necessary to ensure that preventive strategies do not inadvertently cause harm. For example, individuals with underlying medical conditions may require medical clearance before beginning a new exercise regimen. Likewise, significant dietary changes should be implemented under the guidance of a registered dietitian or physician, particularly in individuals with renal disease or electrolyte imbalances.
Monitoring for adverse effects is also crucial when initiating lifestyle interventions. Rapid weight loss, over-exercise, or extreme dietary restrictions can have unintended consequences, including nutrient deficiencies or exacerbation of existing conditions. As such, the principles of hypertension prevention must be applied thoughtfully and with attention to individual variability. By emphasizing informed, gradual change over drastic overhauls, healthcare providers can help patients implement safe, sustainable strategies.
Hypertension Precautions in Special Populations
Certain populations require tailored hypertension precautions due to their unique physiological or socioeconomic circumstances. Older adults, for instance, may have age-related changes in vascular elasticity that necessitate more frequent blood pressure monitoring and medication adjustments. Similarly, pregnant individuals with preeclampsia or gestational hypertension face increased risks and require specialized management strategies to protect both maternal and fetal health.
Individuals from marginalized communities often face barriers to preventive care, including limited access to healthy foods, safe exercise spaces, and culturally competent healthcare. Addressing these social determinants of health is essential for equitable hypertension prevention. Community health initiatives, mobile clinics, and multilingual education campaigns can help bridge these gaps and ensure that all individuals receive appropriate guidance and support.
The Interplay Between Medication and Lifestyle in Hypertension Prevention
Although lifestyle modification is the cornerstone of hypertension prevention, pharmacologic intervention may be necessary in certain high-risk individuals. In these cases, medications should be viewed not as a replacement for healthy habits but as an adjunct to comprehensive risk reduction. Evidence supports the combined use of antihypertensive drugs with dietary and exercise interventions to achieve optimal outcomes.
Patient education is critical in this context. Individuals must understand the purpose, potential side effects, and importance of medication adherence, especially when lifestyle changes alone prove insufficient. Clear communication between patients and providers fosters trust and encourages a proactive approach to health. Ultimately, an integrated model of care—one that respects the value of both medical and behavioral interventions—offers the greatest promise for long-term hypertension control.
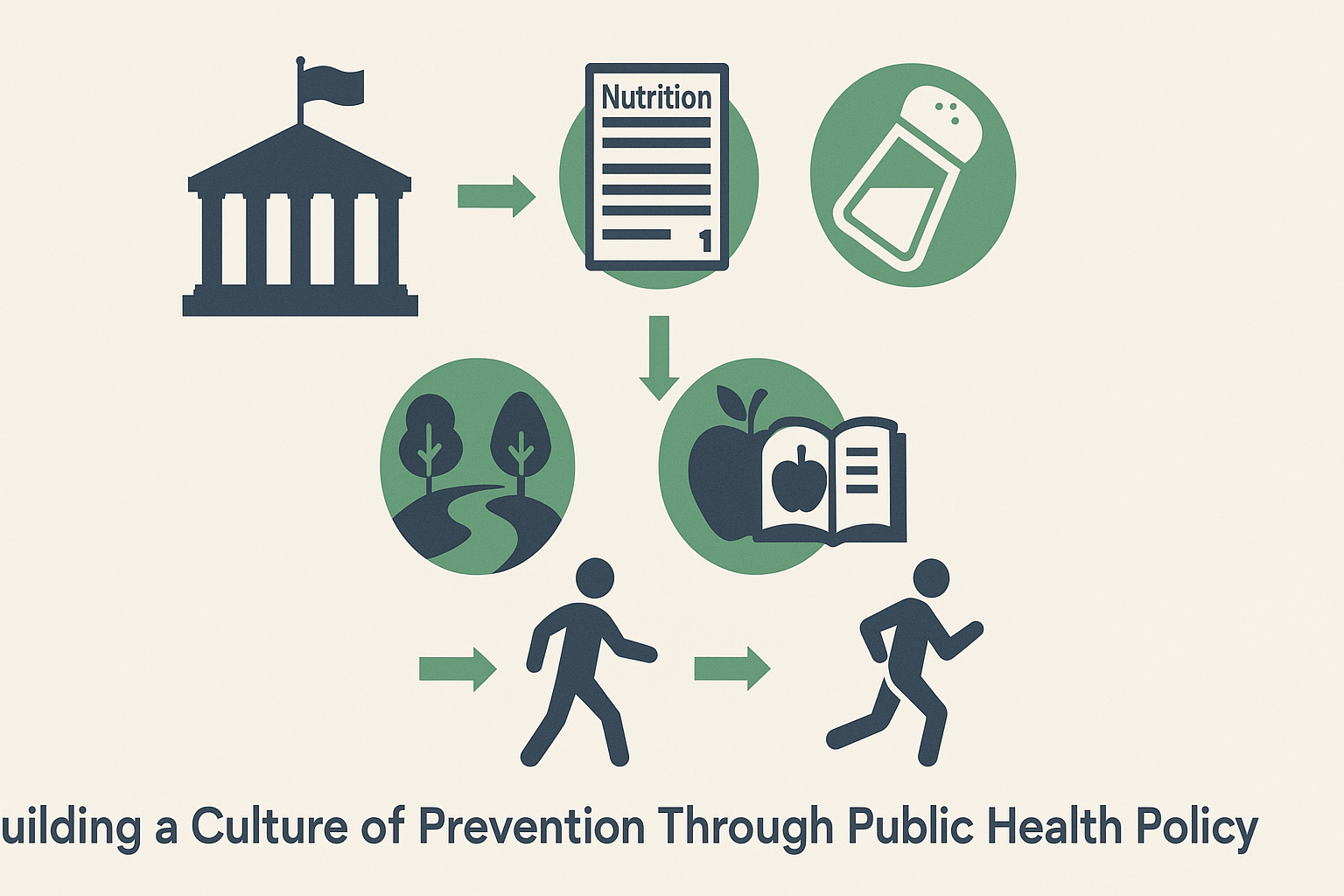
Building a Culture of Prevention Through Public Health Policy
The success of hypertension prevention efforts hinges not only on individual behavior but also on systemic support. Public health policies play a vital role in shaping the environments in which people make health-related decisions. Initiatives such as sodium reduction in processed foods, mandatory food labeling, and taxes on sugar-sweetened beverages have demonstrated effectiveness in shifting population-level dietary habits.
Investment in preventive infrastructure—such as walking trails, community gardens, and health education programs—further reinforces healthy choices. Schools, workplaces, and faith-based organizations can serve as powerful platforms for disseminating information and promoting behavioral change. When prevention is embedded in the fabric of society, the benefits extend far beyond blood pressure control, encompassing broader gains in wellness, productivity, and health equity.
Emerging Research and Future Directions in Hypertension Prevention
Ongoing research continues to refine our understanding of hypertension and how best to prevent it. Advances in genomics and personalized medicine offer the potential to identify individuals with a genetic predisposition to high blood pressure and tailor interventions accordingly. Wearable technologies and mobile health applications provide real-time data that can enhance self-monitoring and engagement.
Furthermore, researchers are exploring the gut microbiome, inflammation, and other novel mechanisms as potential contributors to blood pressure regulation. These insights may pave the way for new therapeutic targets and more precise prevention strategies. As the scientific landscape evolves, it is essential to translate emerging knowledge into actionable guidance that empowers both clinicians and patients.
Frequently Asked Questions: Hypertension Prevention and Lifestyle Safety Considerations
What are some overlooked early indicators that someone should consider hypertension primary prevention?
Many people assume that the absence of symptoms equates to good cardiovascular health, but hypertension often develops silently. Subtle changes like frequent tension headaches, occasional dizziness, or even increased irritability after minor exertion can serve as red flags. Those with sedentary lifestyles or elevated waist circumference should particularly consider engaging in hypertension primary prevention. Additionally, a family history of cardiovascular disease—even in relatives under the age of 60—warrants preemptive action. These early indicators, while often dismissed, can be the tipping point for initiating dietary adjustments, consistent physical activity, and stress management strategies to prevent high blood pressure before it takes root.
How does sleep quality affect hypertension prevention strategies?
Sleep is a critical, yet underappreciated, component of hypertension prevention. Individuals who experience poor sleep—characterized by frequent waking, snoring, or insomnia—often have elevated sympathetic nervous system activity, which contributes to blood pressure elevation. Moreover, inadequate or fragmented sleep disrupts the body’s hormonal regulation, exacerbating inflammation and increasing cortisol levels. As part of a comprehensive hypertension primary prevention plan, improving sleep hygiene through consistent sleep-wake cycles, limiting screen exposure before bedtime, and managing sleep apnea can significantly improve cardiovascular resilience. Addressing sleep disturbances should be viewed as an essential, not peripheral, element of long-term hypertension precautions.
Are there any psychological benefits to adopting a hypertension prevention lifestyle?
Absolutely. Beyond the measurable physical benefits, adopting hypertension prevention strategies often leads to improved emotional well-being. Regular physical activity and nutrient-rich diets positively affect brain chemistry, promoting the release of endorphins and serotonin. Stress-reduction practices, such as mindfulness or yoga, not only support vascular health but also foster emotional regulation and improved resilience. This holistic approach to health encourages a deeper connection between body and mind, creating a reinforcing cycle where improved mental clarity and reduced anxiety further motivate adherence to prevention practices. Therefore, engaging in hypertension primary prevention is not only a physical commitment but also a profound investment in mental wellness.
What are practical ways to implement hypertension precautions in high-stress work environments?
Workplace stress is a pervasive factor that undermines hypertension prevention efforts. Implementing hypertension precautions in high-pressure environments involves both systemic and personal strategies. Employers can help by promoting mental health support, offering flexible schedules, and providing on-site wellness programs. On an individual level, incorporating short, structured breaks for deep breathing or stretching, limiting caffeine intake during peak stress hours, and maintaining ergonomic postures can mitigate risk. Over time, these small, intentional adjustments contribute significantly to a culture of prevention—even in demanding workplaces—and align with broader goals of hypertension primary prevention.
Can technology aid in advancing hypertension primary prevention efforts?
Yes, technological innovation plays a transformative role in modern hypertension prevention. Wearable devices that monitor heart rate variability, sleep quality, and physical activity can provide real-time feedback, empowering users to make immediate lifestyle adjustments. Mobile applications tailored to dietary tracking, guided meditation, and exercise planning help build consistent habits that align with hypertension precautions. Furthermore, AI-driven health platforms can offer personalized insights based on user data, making hypertension primary prevention more accessible and adaptive. As digital health tools evolve, they will continue to support more nuanced and effective safety considerations for hypertension across diverse populations.
What role does cultural sensitivity play in hypertension prevention efforts?
Cultural awareness is essential for successful hypertension prevention, especially in diverse communities where health beliefs and behaviors may differ. Dietary recommendations, for example, must be adapted to accommodate traditional foods and preparation methods. Similarly, physical activity guidelines should consider cultural norms related to gender roles or public exercise. Ignoring these factors can lead to poor adherence and mistrust in preventive initiatives. By integrating cultural sensitivity into hypertension primary prevention programs, healthcare providers can build trust and improve outcomes, ensuring that hypertension precautions are meaningful and actionable for everyone involved.
How do environmental factors complicate hypertension precautions for at-risk populations?
Environmental determinants such as air pollution, noise exposure, and lack of green spaces can undermine even the most diligent hypertension prevention efforts. Chronic exposure to pollutants increases systemic inflammation and oxidative stress, both of which are implicated in hypertension. High-decibel environments, particularly in urban settings, contribute to poor sleep and elevated stress hormones. These external stressors demand a more robust set of hypertension precautions, including public policy advocacy and community-level interventions. Strategies like urban greening, noise regulation, and improved public transportation access represent long-term solutions that complement individual efforts in hypertension primary prevention.
How can family dynamics support or hinder hypertension prevention goals?
Family involvement can be both a catalyst and a barrier to effective hypertension prevention. Supportive family structures encourage shared healthy meals, collective exercise routines, and emotional encouragement during lifestyle transitions. However, environments where unhealthy habits are normalized—such as excessive salt use or low physical activity—can sabotage personal efforts. Open communication, education, and involving family members in wellness planning help reinforce hypertension precautions across the household. Ultimately, making prevention a collective effort increases the likelihood of sustained success and fosters a supportive ecosystem for lasting cardiovascular health.
What are some of the lesser-known safety considerations for hypertension when using complementary therapies?
Complementary therapies such as herbal supplements, acupuncture, or essential oils are increasingly popular but require careful navigation within the context of hypertension precautions. For instance, some natural remedies like licorice root or ginseng can inadvertently raise blood pressure or interact negatively with prescribed medications. Even seemingly benign therapies should be vetted for safety and discussed with a healthcare provider, especially if a person is simultaneously undergoing pharmacologic treatment. Proper integration of these therapies into a hypertension primary prevention plan demands transparency, informed decision-making, and an understanding of potential contraindications. When done responsibly, they may complement—but never replace—evidence-based medical care.
How will future research enhance the effectiveness of hypertension primary prevention strategies?
Emerging research promises to refine and personalize hypertension prevention like never before. Advances in genomics and epigenetics may soon allow for risk assessments tailored to individual genetic profiles, enabling more precise hypertension precautions. Moreover, studies on gut microbiota and its influence on blood pressure regulation could lead to innovative dietary interventions. Behavioral science will also continue to shape how preventive messages are communicated, optimizing engagement through targeted health campaigns. As our understanding deepens, future prevention strategies will likely become more dynamic, multifaceted, and integrative—maximizing both efficacy and safety considerations for hypertension at the population and individual level.
Reflecting on Prevention: A Path Forward for Cardiovascular Health
The prevention of hypertension is a multifaceted endeavor requiring vigilance, education, and sustained effort. By embracing a proactive approach grounded in lifestyle modification, early risk identification, and individualized care, individuals can significantly reduce their risk of developing high blood pressure and its associated complications. Central to this approach are the principles of hypertension primary prevention, which emphasize the value of early intervention before pathology takes root.
Equally important are the safety considerations for hypertension that ensure prevention efforts do not introduce new health risks. These precautions, when thoughtfully applied, allow for the safe adoption of lifestyle changes that support long-term well-being. Recognizing the need for tailored strategies among diverse populations, healthcare systems and public health entities must work collaboratively to build environments conducive to health.
In summary, hypertension prevention is both a personal and societal responsibility. It requires not only individual commitment but also structural support and policy innovation. By integrating evidence-based practices, respecting patient diversity, and fostering a culture of prevention, we can make meaningful strides in reducing the burden of cardiovascular disease and improving population health outcomes for generations to come.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Lifestyle Strategies for Risk Factor Reduction, Prevention, and Treatment of Cardiovascular Disease
Prevention and Control of Hypertension: JACC Health Promotion Series


