Description
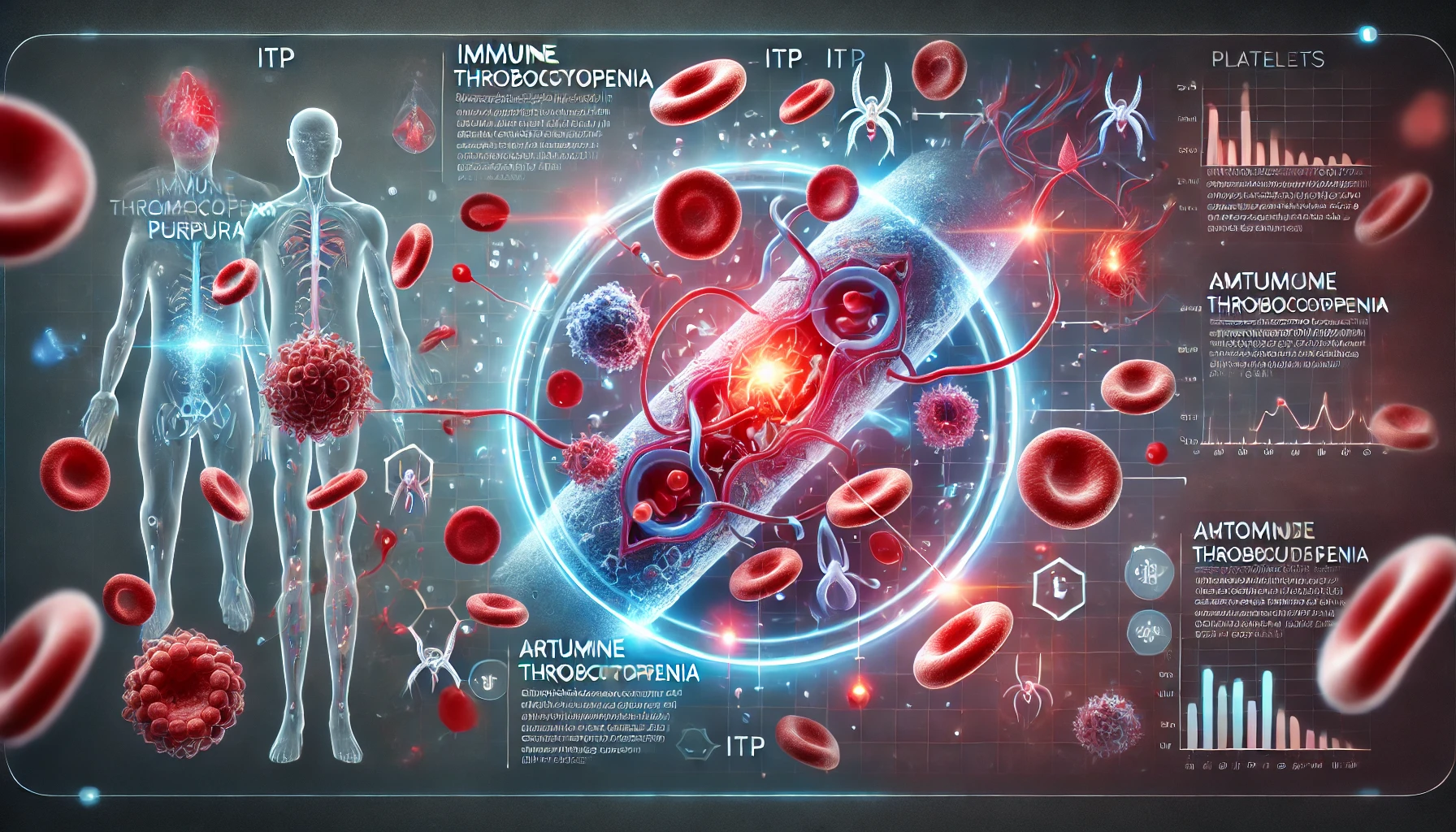
Immune thrombocytopenia (ITP), sometimes called autoimmune thrombocytopenia or autoimmune thrombocytopenic purpura, represents a rare hematologic condition marked by low platelet counts that raises the risk of bleeding. A lower platelet count largely characterizes ITP because of immune system dysfunction that results in both impaired production and platelet destruction. The primary defining feature of ITP is a lower platelet count, which is caused by immune system dysfunction that results in both platelet breakdown and impaired production. Bleeding disorders including purpura and petechiae can result from a reduction in platelets, which are essential for blood clotting. Furthermore, in more serious situations, ITP may cause internal bleeding.
You May Also Like:
Henoch-Schönlein purpura / IgA vasculitis: Description, Causes, and Treatment Protocol
Immune-mediated necrotizing myopathy (IMNM): Description, Causes, and Treatment Protocol
Immune thrombocytopenia (ITP) / Autoimmune thrombocytopenic purpura / Autoimmune thrombocytopenia: Description, Causes, and Treatment Protocol is an original (MedNewsPedia) article.
Possible Causes
Many times, the precise etiology of ITP is still unknown. However, several reasons and contributing variables have been linked to its emergence. Among these causes are the following:
Immune Reaction: An autoimmune condition is the most commonly recognized theory about ITP. Platelets get attacked and destroyed by antibodies that the immune system incorrectly creates because it perceives them as foreign bodies. Platelets in the blood drop as a result of this.
Genetic Vulnerability: Some people may be more susceptible to developing ITP due to a hereditary predisposition. The specific genetic elements that result in ITP are likely complex and not fully known.
Viral Infections: ITP development or aggravation has been connected to specific viral infections. Viruses that can cause the breakdown of platelets include HIV, hepatitis C, Epstein-Barr virus (EBV), varicella-zoster virus (VZV), and cytomegalovirus (CMV).
Medications: ITP has been linked to the onset of certain drugs. Medications that can cause or worsen ITP in those who are vulnerable include anticonvulsants, heparin (a particular blood thinner), some antibiotics (like penicillin), and other drugs. Immune-mediated processes are thought to have a role in this.
Childhood Infections: Some childhood diseases, which include bacterial or viral infections, may occur before ITP manifests in pediatric instances. An atypical immunological reaction that targets platelets can be brought on by these infections.
Pregnancy: Sometimes ITP happens right after giving birth or even during pregnancy. An increased risk of developing or exacerbating ITP may result from changes in immune system activity and hormone levels during pregnancy.
Other Autoimmune Disorders: People who already suffer from other autoimmune conditions, like rheumatoid arthritis, autoimmune thyroid disorders, or systemic lupus erythematosus, are more susceptible to ITP. These ailments could be a factor in the immune system’s instability, which could trigger ITP.
Exacerbating and Mitigating Factors
ITP symptoms and progression can be made worse or better by a variety of circumstances. It is essential to comprehend these elements to successfully manage the illness. The following are the variables that aggravate and alleviate ITP:
The exacerbating factors include:
Infections: By boosting the body’s immune response and increasing platelet breakdown, bacterial or viral infections can either cause or exacerbate ITP. ITP is frequently associated with Helicobacter pylori, HIV, hepatitis C, and pulmonary viral infections.
Stress: Psychological stress or physical stressors can potentially exacerbate ITP symptoms. Stress might influence the immune system and trigger immune responses that affect platelet destruction.
Pregnancy: Due to hormone fluctuations and the increased strain on the body during pregnancy, people with ITP may experience difficulties. Careful monitoring and control are necessary as it may cause variations in platelet levels.
Chronic Conditions: ITP can be made more difficult and exacerbated by the coexistence of other autoimmune conditions including rheumatoid arthritis or systemic lupus erythematosus (SLE).
Medications: There is a link between the onset or worsening of ITP and some drugs. Medications that can cause or exacerbate ITP in vulnerable patients include blood thinner heparin, some antibiotics, anti-seizure medicines, and more.

The mitigating factors include:
Infection Prevention: It is possible to lessen the chance that infections can cause or exacerbate ITP by maintaining proper hygiene, receiving the required immunizations, and taking preventative measures.
Stress Management: Techniques for lowering stress, like mindfulness, relaxation, and stress-relieving activities, may be able to control immunological reactions and hence aid in the management of ITP symptoms.
Avoiding Triggers: The chance of flare-ups can be reduced by recognizing and avoiding factors that might aggravate ITP, including specific drugs known to cause or worsen the condition.
Continual Medical Examination: Regular visits with healthcare experts are necessary to ensure consistent assessment of platelet levels and general health. If management is required, this aids in the prompt identification of variations in platelet counts.
Healthy Lifestyle: Upholding a healthy lifestyle that includes regular exercise, a well-balanced diet, enough sleep, abstaining from tobacco and excessive alcohol use, and so on, can enhance general well-being and possibly even boost immune system performance.
Medication Administration: Maintaining close communication with medical professionals to guarantee proper medication management, which includes choosing medications carefully so they don’t worsen ITP, is essential.
Standard Treatment Protocol
The extent of the disease, the existence of bleeding signs, and whether the patient has persistent or acute ITP all influence the typical treatment plan for the condition. Increasing platelet levels, averting bleeding episodes, and managing symptoms are the main objectives of treatment. This is a summary of the typical therapies for ITP that are often employed:
Monitoring without Medical Intervention: Close observation without prompt action may be advised for people with mild instances of ITP who do not exhibit bleeding symptoms. Monitoring platelet counts and scheduling routine examinations are crucial for identifying any shifts in the severity of the illness.
Corticosteroids: For ITP, corticosteroids such as prednisolone or prednisone are frequently used as initial treatment. These drugs aid in immune system suppression, which lessens the amount of platelets that antibodies destroy. While corticosteroids are useful for quickly raising platelet counts, chronic use may result in adverse effects.
Thrombopoietin Receptor Agonist (TPO-RA): Romiplostim and eltrombopag include examples of TPO-RA medications that increase platelet synthesis in the bone marrow. In cases of chronic ITP or when alternative therapies are unable to sustain sufficient platelet counts, TPO-RA medicines are often utilized.

Rituximab: A monoclonal antibody called rituximab inhibits the immune system’s ability to destroy platelets by targeting particular cells. When alternative treatments have failed to improve the condition of someone with persistent ITP, it might be worth considering.
Intravenous Immunoglobulin (IVIG): Concentrated immunoglobulins from healthy donors are infused during IVIG. In individuals suffering from ITP, it can rapidly raise platelet counts and aid in regulating the immune system’s reaction. When quick platelet elevation is required to stop or prevent bleeding, IVIG is especially helpful.
Splenectomy: For patients with severe or persistent ITP, surgical splenectomy may be considered, particularly if other therapies have proven ineffective. Since the spleen serves as a significant site for platelet breakdown, removing it occasionally raises platelet levels.
Providing Supportive Care: Taking care of bleeding symptoms when they appear is another aspect of managing ITP. This includes avoiding activities that could raise the chance of injury and applying topical treatments or drugs to reduce bleeding.

Treatment Options
People suffering from ITP may discover that natural remedies and alternative therapies help manage their condition in addition to traditional medical therapy. Several researched supplemental therapies include the following:
Nutritional Supplements: Sustaining sufficient quantities of specific vitamins can benefit general health. Although a definite correlation between vitamin supplements and ITP treatment has not been shown, consuming enough iron, vitamins C and K, can improve overall health and may even help with platelet activity.
Natural Remedies: When seeking alternative treatments to traditional medical protocols, people with ITP frequently turn to natural solutions. These are a few herbal treatments that have been investigated for ITP:
Omega-3 Fatty Acids
Since they have anti-inflammatory qualities, omega-3 fatty acids may help reduce ITP-related inflammation. Omega-3-rich fish oil supplements may help lower signs of inflammation.
Turmeric/Curcumin
The key ingredient in turmeric, curcumin, is well-known for having anti-inflammatory qualities and has been researched for possible anti-inflammatory effects. Although turmeric might help manage inflammation associated with ITP, further research is needed to determine its specific impacts on platelet counts.
Herbal Remedies: Some herbs have been utilized traditionally for their possible immune-modulating qualities, even though their implications on ITP are still mostly unknown. Examples comprise:
Ginkgo Biloba
According to some research, ginkgo biloba may help people with ITP experience less bleeding and a rise in platelet counts. To prove its safety and efficacy, more research is necessary as the available data is limited.

Astragalus
Traditional Chinese medicine has utilized astragalus because of its well-known ability to modulate the immune system. Though further research is needed to fully understand its function in ITP management, some preliminary evidence suggests it may have an impact on the body’s immune system.
However, it is significant to note that these supplementary approaches and herbal remedies may be considered supplementary. That is, they must not supplant the conventional medical treatments that are provided by healthcare practitioners to manage ITP. Incorporating these adjunct therapies gradually with expert guidance is necessary to guarantee their safety and possible advantages in the overall treatment of ITP.
Conclusion
Effective management of Immune Thrombocytopenia (ITP) requires a holistic approach that integrates conventional medical treatments with supportive therapies. Alongside standard treatments like corticosteroids, IVIG, and thrombopoietin receptor agonists, certain supplements may provide additional benefits. These include Omega-3 fatty acids, which have anti-inflammatory properties, and Curcumin (from turmeric), known for its potential to reduce inflammation.
Natural remedies such as Ginkgo Biloba and Astragalus may offer immune-modulating benefits, but their use should be carefully monitored under medical guidance. These supplements and remedies should always complement—not replace—medical treatments and be part of a personalized care plan developed with a healthcare professional.
Additional resources for further reference
https://www.ncbi.nlm.nih.gov/books/NBK537240
https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(22)00009-3/fulltext
https://www.frontiersin.org/articles/10.3389/fimmu.2018.00880/full
https://onlinelibrary.wiley.com/doi/full/10.1111/ejh.13319
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.