Understanding Coronary Artery Disease: A Global Health Challenge
Coronary artery disease (CAD) remains one of the most pressing public health concerns worldwide. Affecting millions each year, it is a leading cause of death and disability across industrialized and developing nations alike. As modern medicine evolves, the question continues to arise: is coronary artery disease treatable? The answer is both encouraging and nuanced. While CAD is not always curable in the traditional sense, a wide range of highly effective treatments now exist to manage the disease, minimize complications, and improve long-term outcomes. Understanding the underlying pathology of CAD is essential to appreciate the modern therapeutic landscape and why advancements in coronary treatment are helping patients live longer and healthier lives.
You may also like: How to Naturally Reverse 20 Years of Arterial Plaque: Science-Backed Strategies for a Healthier Heart
CAD occurs when the coronary arteries—the blood vessels that supply oxygen-rich blood to the heart muscle—become narrowed or blocked due to the accumulation of plaque. This plaque, composed of cholesterol, fatty substances, and cellular waste, gradually reduces blood flow, potentially leading to angina (chest pain), heart attacks, or even heart failure. Importantly, CAD is a chronic, progressive condition. This means that while the disease may not be entirely reversible, it can be effectively managed through comprehensive medical treatment, lifestyle modification, and in some cases, surgical intervention. Addressing both the symptoms and the root causes of atherosclerosis is at the heart of every modern CAD treatment strategy.

The Science of CAD: Anatomy, Pathophysiology, and Risk Factors
To fully grasp how to treat CAD, one must first understand the intricate anatomy and pathophysiology underlying this condition. At its core, CAD is a disease of the arterial wall, where damage to the endothelium (the inner lining of blood vessels) initiates a cascade of inflammatory and lipid accumulation processes. This leads to the formation of atherosclerotic plaques that stiffen the arteries and reduce their ability to dilate in response to increased oxygen demand.
This dysfunction in the coronary artery anatomy has significant downstream effects. Reduced blood flow limits the delivery of oxygen and nutrients to myocardial tissue, especially during times of exertion or stress. When the oxygen supply-demand mismatch becomes severe, myocardial ischemia occurs. Over time, persistent ischemia can weaken the heart muscle, contributing to the development of ischemic cardiomyopathy and chronic heart failure. Recognizing these pathophysiological changes is key to selecting appropriate medical therapies aimed at reducing plaque burden, controlling symptoms, and preventing major cardiovascular events.
Several well-established risk factors contribute to the development of CAD. These include both modifiable and non-modifiable elements. High blood pressure, elevated LDL cholesterol, diabetes, smoking, and sedentary lifestyle are among the most influential modifiable risk factors. Genetics, age, and male sex are non-modifiable, but understanding their influence can still help guide preventive strategies. Contemporary medical treatment for CAD increasingly focuses on individualized risk assessment to tailor interventions based on a person’s unique profile.
Is Coronary Artery Disease Treatable? Clarifying the Concept of Treatment vs. Cure
The terminology surrounding CAD can sometimes be confusing for patients. When people ask, “Is coronary artery disease curable?” or “Can coronary heart disease be cured?”, they may be expecting a definitive fix—a cure in the traditional sense. However, the medical consensus is that while CAD may not be curable in the sense of permanent reversal, it is very much treatable. The phrase “cure for CAD” should be reframed to reflect the reality that modern medicine allows for long-term disease management and often, the prevention of progression.
A more accurate question may be: how can coronary artery disease be treated? Or, how to treat CVD in a way that improves both quality of life and longevity? The answer involves a multipronged approach that combines pharmacological interventions, lifestyle modification, risk factor control, and, in certain cases, procedural or surgical interventions. Advances in cardiovascular pharmacology and interventional cardiology have transformed what was once a fatal disease into a chronic, manageable condition. In this sense, while we may not speak of a definitive “cure for CAD,” modern medicine offers tools that can halt its progression and, in some cases, reverse certain aspects of the disease process.
Pharmacologic Foundations: The Role of CAD Medications in Disease Management
One of the most powerful tools in the fight against coronary artery disease is pharmacotherapy. The medical treatment of coronary artery disease relies on a sophisticated array of medications designed to target different aspects of the disease process. Drugs for coronary heart disease include statins, beta-blockers, ACE inhibitors, calcium channel blockers, nitrates, and antiplatelet agents, among others. Each class plays a distinct role in modifying disease progression, reducing symptoms, and lowering the risk of cardiovascular events.
Statins, for instance, are cornerstone therapies in CAD medicine. They reduce LDL cholesterol levels, stabilize atherosclerotic plaques, and have anti-inflammatory properties. Numerous large-scale trials have demonstrated that statin therapy significantly reduces the incidence of heart attacks and strokes in both primary and secondary prevention populations. Beta-blockers are another mainstay, particularly useful in patients with a history of myocardial infarction or those experiencing angina. They work by reducing heart rate and myocardial oxygen demand, helping to prevent ischemia.
ACE inhibitors and ARBs (angiotensin receptor blockers) contribute to the medical treatment for CAD by improving endothelial function, lowering blood pressure, and providing protective effects on the heart muscle. Nitrates, which dilate blood vessels and relieve chest pain, are often used for symptomatic relief. Antiplatelet drugs like aspirin and clopidogrel play a preventive role by reducing the risk of clot formation within narrowed coronary arteries. The choice of medication for coronary heart disease is often personalized, taking into account the severity of disease, patient comorbidities, and specific therapeutic goals.

Evolving Therapies: Novel Drugs and Personalized CAD Medicine
In recent years, significant strides have been made in developing novel therapies to treat CAD. Beyond traditional statins and antihypertensives, newer classes of drugs are redefining how we approach coronary artery disease medication. PCSK9 inhibitors, for example, represent a breakthrough in lipid management. These injectable monoclonal antibodies dramatically reduce LDL cholesterol levels and are especially beneficial for patients with familial hypercholesterolemia or those who do not achieve target levels with statins alone.
Similarly, the emergence of SGLT2 inhibitors and GLP-1 receptor agonists has revolutionized cardiovascular care for patients with type 2 diabetes. Originally developed as glucose-lowering agents, these drugs have shown impressive cardioprotective effects, including reductions in heart failure hospitalization and major adverse cardiovascular events. These developments underscore the importance of integrating CAD treatment with broader cardiometabolic strategies.
Moreover, the field of CAD anatomy medicine is becoming increasingly personalized. Genetic testing, biomarker analysis, and advanced imaging techniques allow clinicians to tailor medical treatment of coronary artery disease based on individual pathophysiology. For example, high-sensitivity CRP levels can help guide the use of anti-inflammatory agents, while coronary calcium scoring can identify patients at highest risk. Personalized medicine is not just a futuristic ideal—it is actively reshaping how we treat CAD today.
Beyond Medication: Interventional and Surgical Coronary Treatment Options
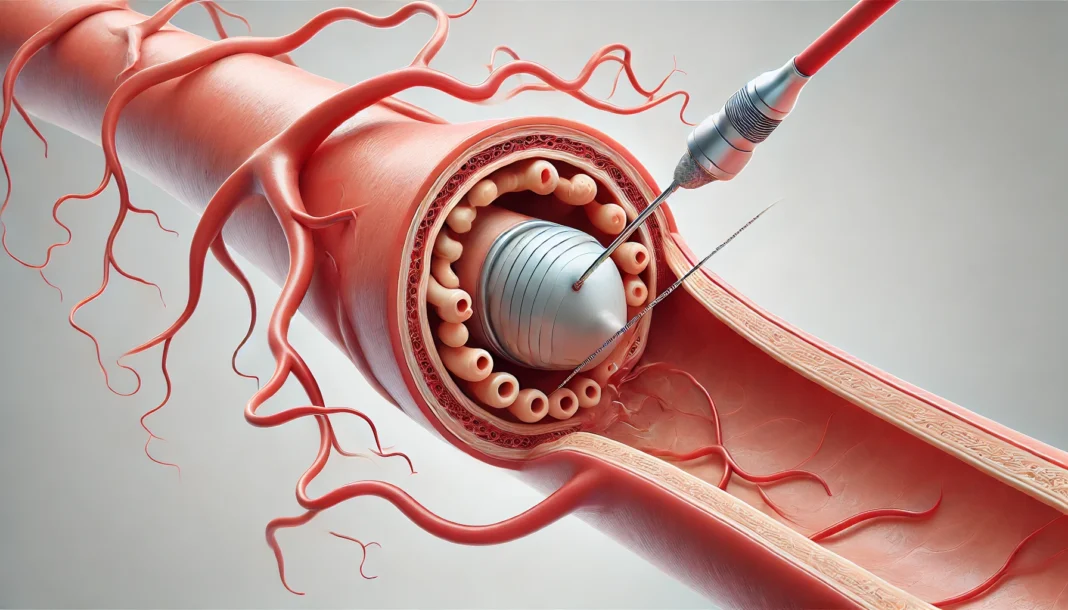
While medications play a central role, certain cases of CAD require mechanical revascularization to restore adequate blood flow to the heart. Percutaneous coronary intervention (PCI), commonly known as angioplasty with stent placement, is one of the most widely used procedures in modern coronary treatment. It is especially beneficial for patients with acute coronary syndromes or those with significant symptomatic disease despite optimal medical therapy.
Coronary artery bypass grafting (CABG) is a surgical option typically reserved for patients with complex multivessel disease, left main coronary artery disease, or diabetes with diffuse atherosclerosis. CABG improves survival in selected populations and can provide long-lasting symptom relief. Both PCI and CABG are supported by robust clinical evidence and are integral components of comprehensive CAD treatment strategies.
However, these procedures do not replace the need for ongoing pharmacotherapy. They are most effective when combined with aggressive risk factor modification and continued medical management. Patients must understand that interventions are not curative but are part of a broader approach to how we treat CVD. The question is not merely can blocked arteries be treated with medication or surgery, but how these strategies complement each other in improving outcomes.
Lifestyle Medicine: Treating CAD from the Ground Up
No discussion of how to treat CHD is complete without addressing the critical role of lifestyle modification. In fact, for many patients, the most transformative interventions begin not with a prescription, but with changes to daily habits. Dietary modification, regular exercise, smoking cessation, and stress management are foundational elements of any effective CAD treatment plan.
A heart-healthy diet, such as the Mediterranean or DASH (Dietary Approaches to Stop Hypertension) diet, emphasizes fruits, vegetables, whole grains, lean protein, and healthy fats while minimizing processed foods and added sugars. These dietary patterns have been shown to reduce LDL cholesterol, improve blood pressure, and decrease inflammation—all key contributors to atherosclerosis. Exercise is equally important. Aerobic activity improves endothelial function, enhances insulin sensitivity, and promotes favorable lipid profiles.
Smoking cessation is perhaps the single most effective lifestyle change for those seeking a cure for CAD in a practical sense. The benefits begin within days of quitting and accumulate over time, significantly reducing cardiovascular risk. Stress management and adequate sleep also play vital roles in supporting cardiovascular health. Lifestyle medicine is not an alternative to pharmacologic therapy but a necessary partner in the long-term management of coronary artery disease.
Prevention and Early Detection: Halting CAD Before It Starts
Preventive cardiology is gaining momentum as healthcare systems increasingly recognize that the best way to treat CAD is to prevent it in the first place. Early identification of risk factors and implementation of preventive strategies can significantly reduce the burden of disease. Regular screenings, including lipid panels, blood pressure monitoring, and blood glucose tests, help identify individuals at high risk.
Public health campaigns that promote physical activity, healthy eating, and smoking cessation are essential tools in reducing the global prevalence of CAD. Educational efforts aimed at demystifying coronary artery disease medication and encouraging adherence to prescribed treatments are equally important. When patients understand how CAD medications work and why they matter, they are more likely to stick with them long-term.
In some cases, advanced imaging techniques such as coronary CT angiography or calcium scoring may be used to assess subclinical atherosclerosis. These tools provide a window into early disease and allow for proactive interventions. As the question “Is heart disease treatable?” continues to resonate, the growing emphasis on prevention offers a hopeful answer: by treating risk factors early and aggressively, we can often delay or even prevent the onset of symptomatic disease.

Frequently Asked Questions: Understanding and Advancing CAD Treatment
What are the lesser-known medications used in CAD treatment, and how do they work?
In addition to commonly prescribed statins and beta-blockers, several lesser-known medications are increasingly being used in modern CAD treatment. For example, ivabradine, which selectively reduces heart rate without affecting blood pressure, is particularly useful in patients who cannot tolerate beta-blockers. Another emerging option is ranolazine, which works by improving myocardial efficiency and reducing angina symptoms without significantly altering blood pressure or heart rate. These alternatives expand the therapeutic landscape for those who require personalized medical treatment for CAD. Incorporating newer coronary artery disease medication options can also enhance patient outcomes when traditional approaches prove insufficient.
Can CAD be treated without procedures or surgery?
Yes, many individuals can successfully treat CAD without resorting to procedures like angioplasty or bypass surgery. Medical treatment of coronary artery disease has become highly effective due to advancements in pharmacology and lifestyle-based interventions. Patients with stable CAD may rely solely on medication for coronary heart disease, such as antiplatelet agents, statins, and vasodilators, alongside comprehensive lifestyle changes. However, close monitoring is essential to ensure that symptoms do not escalate, warranting procedural intervention. For those wondering how can coronary artery disease be treated non-invasively, the answer often lies in adherence to a holistic care model tailored to individual risk profiles.
How does inflammation play a role in CAD, and can it be targeted through treatment?
Inflammation is increasingly recognized as a pivotal player in atherosclerosis, the underlying process of CAD. Elevated levels of high-sensitivity C-reactive protein (hs-CRP) are linked to increased cardiovascular risk, even in patients with well-controlled cholesterol. Some anti-inflammatory agents, such as colchicine and canakinumab, have shown promise in reducing cardiovascular events by directly targeting vascular inflammation. This adds a new dimension to CAD medicine by emphasizing not just cholesterol management but also immune modulation. As the concept of CAD anatomy medicine evolves, inflammation-targeted therapies may emerge as essential tools in the long-term medical treatment for CAD.
Can blocked arteries be treated with medication alone, and in what cases is this approach preferred?
While mechanical interventions remain the gold standard in acute settings, blocked arteries can sometimes be managed effectively with medication alone, especially in cases of stable angina. Medications that improve endothelial function, such as nitrates, calcium channel blockers, and ACE inhibitors, can enhance coronary perfusion without the need for invasive procedures. This conservative approach is often preferred in elderly patients or those with multiple comorbidities who may not tolerate surgery well. Understanding when to opt for medicine for blocked arteries instead of revascularization requires a nuanced risk-benefit analysis, often guided by stress tests or imaging studies. Ultimately, choosing the right CAD medications is crucial for balancing efficacy with safety in such scenarios.
What innovations are on the horizon for improving CAD treatment outcomes?
The future of coronary treatment is being shaped by innovations in gene therapy, regenerative medicine, and digital health integration. Gene-editing tools like CRISPR offer the potential to address genetic contributors to lipid metabolism and inflammation. Meanwhile, stem cell therapy is under investigation for its capacity to regenerate ischemic myocardium and restore vascular integrity. On the tech front, wearable biosensors and AI-driven risk prediction models are transforming how clinicians monitor and adjust medication for coronary heart disease in real time. As precision medicine advances, individualized cad treatment plans will become more adaptive, responsive, and potentially curative in select cases. These breakthroughs signal a shift toward more proactive and predictive medical care for cardiovascular disease.
How do psychological and emotional health impact CAD treatment success?
The psychological dimension of CAD is often overlooked, yet it significantly affects treatment adherence and recovery. Anxiety, depression, and chronic stress have been linked to poor cardiovascular outcomes, in part due to their influence on inflammatory markers and autonomic dysfunction. Incorporating mental health support into CAD treatment plans—through counseling, cognitive-behavioral therapy, or mindfulness training—can improve patient engagement and clinical outcomes. Studies have shown that patients with better emotional well-being are more likely to follow their medication regimens and maintain healthy lifestyle changes. Addressing emotional health is therefore not only compassionate care but also a strategic component of how to treat CVD effectively and sustainably.
What dietary strategies go beyond general advice to support CAD management?
Beyond standard dietary recommendations, emerging research supports the cardioprotective effects of specific nutrients such as omega-3 fatty acids, polyphenols, and dietary nitrates. Foods rich in polyphenols, such as berries and dark chocolate, may improve endothelial function and reduce oxidative stress. Nitrate-rich vegetables like spinach and beetroot can enhance nitric oxide production, aiding in vasodilation and blood pressure control. Furthermore, time-restricted eating and intermittent fasting protocols have shown preliminary benefits in reducing inflammatory markers and improving lipid profiles. These nuanced dietary strategies offer additional tools to support medical treatment of coronary artery disease in daily practice. For patients looking to treat CAD more holistically, diet becomes a powerful adjunct to meds for CAD.
Is coronary artery disease curable through lifestyle changes alone?
While lifestyle changes can dramatically slow progression and even reverse some aspects of atherosclerosis, labeling CAD as fully curable through lifestyle alone remains controversial. Intensive lifestyle interventions, such as those promoted by the Ornish Program, have demonstrated regression of arterial plaque in select patients. However, these programs require sustained, comprehensive changes in diet, exercise, stress management, and social support. The concept of a cure for CAD may apply in rare, highly controlled settings but is not broadly achievable without concurrent pharmacologic support. Still, for motivated individuals, these interventions offer a pathway to minimize or even eliminate the need for certain drugs for CAD.
What role do social determinants of health play in CAD outcomes?
Social determinants—such as income, education, housing stability, and access to care—play a substantial role in CAD incidence and treatment outcomes. Individuals in underserved communities often face higher exposure to risk factors and reduced access to consistent coronary treatment. These disparities can lead to delayed diagnosis, suboptimal use of coronary artery disease medication, and poorer long-term control. Addressing these systemic issues requires policy-level interventions and community health initiatives aimed at improving equity in cardiovascular care. Recognizing the social context is a key step in improving how we treat heart disease across diverse populations.
Can cardiovascular disease be cured with emerging biotech solutions?
Although there is currently no definitive cure for CAD, emerging biotechnology offers exciting potential to fundamentally alter the disease course. Nanomedicine, for example, is being explored to deliver targeted drugs for coronary heart disease directly to inflamed plaques, minimizing systemic side effects. Meanwhile, messenger RNA (mRNA)-based therapies, similar to those used in COVID-19 vaccines, may one day be employed to stimulate protective proteins or reverse endothelial damage. While still in early phases, these innovations highlight how the idea of whether cardiovascular disease can be cured may evolve in the future. These developments offer a glimpse into transformative approaches that go beyond current CAD medications and open the door to revolutionary treatments.
Conclusion: The Future of CAD Treatment—Managing a Chronic Condition with Precision and Hope
So, is coronary artery disease treatable? Unquestionably, yes—although the term “treatable” may not always equate to curable, it signifies the tremendous progress modern medicine has made in managing this complex condition. Today, patients diagnosed with CAD have more options than ever before. From powerful drugs for CAD and coronary artery disease medication to minimally invasive interventions and lifestyle therapies, we now possess an arsenal of tools to combat this once-devastating disease.
Medical treatment for CAD has evolved beyond the traditional model of symptom suppression. Instead, we now aim for risk reduction, disease stabilization, and in some cases, regression of atherosclerotic burden. Personalized care, driven by precision diagnostics and emerging therapies, allows us to tailor interventions in ways never before possible. Whether through medications, procedures, or holistic lifestyle changes, our approach to coronary treatment is dynamic, evidence-based, and continually improving.
The road ahead promises further innovation, with gene therapy, advanced imaging, and even AI-guided treatment protocols poised to shape the next generation of CAD care. While there may never be a one-size-fits-all cure for coronary heart disease, our growing understanding of its mechanisms has brought us closer to controlling its impact on individual lives and global health alike. For anyone facing a diagnosis of CAD, the takeaway is clear: with the right treatment plan, informed lifestyle choices, and adherence to medical guidance, there is every reason to hope for a long, active, and fulfilling life.
CAD is not the end of the road—it is a call to action. A diagnosis today is a prompt to engage with a comprehensive, strategic, and empowering plan to protect and preserve heart health for years to come.
atherosclerosis management, cardiovascular risk reduction, heart-healthy lifestyle, cholesterol lowering strategies, cardiac rehabilitation programs, endothelial function improvement, blood pressure control, ischemic heart conditions, myocardial ischemia treatment, cardiac pharmacology, vascular health support, heart attack prevention, chronic heart disease care, anti-inflammatory heart therapies, metabolic syndrome and heart disease, personalized cardiology care, cardiac imaging advances, non-invasive heart treatments, integrative cardiac medicine, emerging heart therapies
Further Reading:
What to know about coronary artery disease
What Is Coronary Artery Disease?
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.