High blood pressure, or hypertension, is often referred to as a silent killer due to its subtle symptoms and severe long-term consequences. Affecting nearly half of the adult population in the United States, this common cardiovascular disorder has been closely examined through the lens of lifestyle, diet, stress, and more recently, genetics. As scientific inquiry continues to unravel the origins of this condition, a critical question arises: is hypertension hereditary? This article delves into the growing body of research exploring whether high blood pressure is passed down through family lines and how inherited traits may predispose individuals to this chronic condition. We will also explore what can be done—despite a potential genetic burden—to prevent, monitor, and manage high blood pressure effectively.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Defining Hypertension and Its Health Consequences
To fully appreciate the significance of hypertension as a hereditary disease, one must first understand what hypertension entails and why it matters. Blood pressure is the force exerted by circulating blood on the walls of the arteries. It is measured in millimeters of mercury (mmHg) and recorded as two values: systolic pressure (the higher number), which measures pressure when the heart beats, and diastolic pressure (the lower number), which reflects pressure when the heart is at rest. A normal reading typically falls below 120/80 mmHg, while readings consistently above 130/80 mmHg are classified as hypertensive.
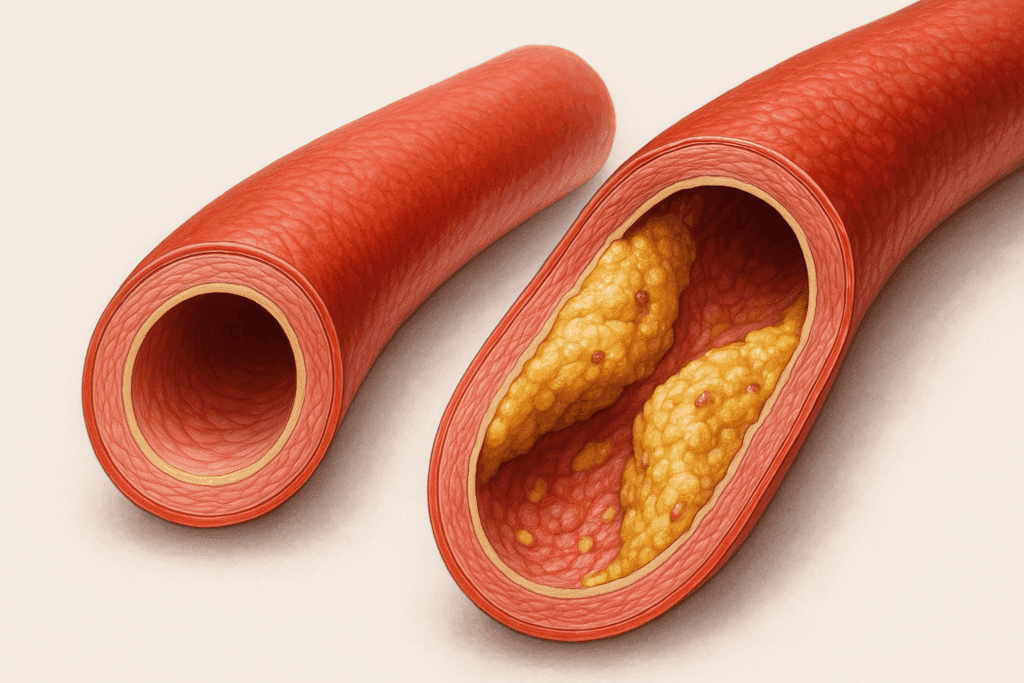
Unchecked, hypertension can lead to a host of cardiovascular disorders. These include heart attacks, strokes, heart failure, kidney disease, and aneurysms. Additionally, chronic high blood pressure can damage arteries, making them less elastic and more prone to the buildup of plaque—a condition known as atherosclerosis. These outcomes highlight why identifying risk factors, including potential genetic ones, is essential in the fight against this disease.
What Does It Mean for a Condition to Be Hereditary?
When a disease is described as hereditary, it means there is a genetic component that may be passed from parents to offspring. In other words, inherited genes can influence the likelihood of developing a condition, though the presence of such genes does not guarantee the disease will manifest. For complex diseases like hypertension, multiple genes—each with small effects—are involved, and their expression may be influenced by environmental factors, lifestyle choices, and other medical conditions.
So, is blood pressure hereditary in the same way that eye color or blood type is? The answer is more nuanced. Unlike monogenic disorders such as cystic fibrosis or Huntington’s disease, which are caused by mutations in a single gene, hypertension is considered a polygenic disorder. It involves many genetic variations, each contributing incrementally to overall risk. This complexity makes it more difficult to predict and manage based solely on family history, but it also underscores the importance of individualized prevention strategies.
The Genetic Architecture of Hypertension
Advances in genomic research have begun to illuminate how genetics influences blood pressure regulation. Several large-scale genome-wide association studies (GWAS) have identified over a hundred gene variants associated with blood pressure regulation. Some of these genes affect the renin-angiotensin-aldosterone system (RAAS), which plays a key role in blood volume and arterial constriction. Others impact kidney function, sodium balance, vascular tone, and sympathetic nervous system activity.
For example, variants in the AGT gene, which codes for angiotensinogen, have been associated with increased blood pressure. Similarly, mutations in the ADD1 gene, involved in sodium retention, have been linked to salt-sensitive hypertension. These findings provide compelling evidence that yes, high blood pressure can be inherited through a complex web of genetic predispositions. Still, the presence of these genes does not guarantee hypertension will occur, reinforcing the interplay between nature and nurture.
Family History as a Risk Indicator
Clinicians often consider family history as a key risk factor when assessing a patient’s likelihood of developing hypertension. If one or both parents have high blood pressure, the probability of their child developing it increases significantly. Epidemiological studies suggest that individuals with a family history of hypertension are approximately twice as likely to develop the condition themselves.
However, while family history serves as a strong indicator, it also reflects shared environmental and lifestyle influences. Families tend to share dietary habits, levels of physical activity, stress-coping mechanisms, and even socioeconomic status. Thus, the question of whether hypertension is hereditary or shaped by a shared lifestyle often becomes a matter of degree rather than dichotomy. Nonetheless, the evidence remains strong that genetics play a substantial role.
Twin and Adoption Studies: Isolating Genetic Influence
Twin studies offer a unique opportunity to distinguish between genetic and environmental factors. Identical twins share 100% of their DNA, while fraternal twins share about 50%. If a trait is significantly more common in identical twins compared to fraternal twins, this suggests a genetic influence. Multiple studies have demonstrated higher concordance rates for high blood pressure among identical twins, lending further support to the notion that is hypertension hereditary is more than just a rhetorical question—it’s an observable pattern in real-world data.
Adoption studies further isolate genetic factors by examining individuals raised apart from their biological parents. In such studies, adoptees whose biological parents had hypertension were more likely to develop the condition, even when raised in a different environment. These findings help to disentangle the hereditary nature of high blood pressure from environmental confounders.
Epigenetics and Gene-Environment Interactions
A rapidly growing area of research known as epigenetics is shedding light on how environmental factors can influence gene expression without altering the underlying DNA sequence. Mechanisms such as DNA methylation and histone modification can activate or silence genes, thereby affecting physiological outcomes like blood pressure. For instance, chronic stress, poor diet, and exposure to toxins can trigger epigenetic changes that elevate hypertension risk—even in individuals who may not carry traditionally “high-risk” genes.
Moreover, prenatal and early childhood exposures play a critical role. Studies have shown that low birth weight and maternal malnutrition are associated with higher blood pressure later in life. These findings suggest that the question of whether high blood pressure is inherited must also consider the intrauterine environment and early life conditions. Gene-environment interactions thus represent a dynamic and evolving field that continues to inform our understanding of hypertension’s hereditary dimensions.
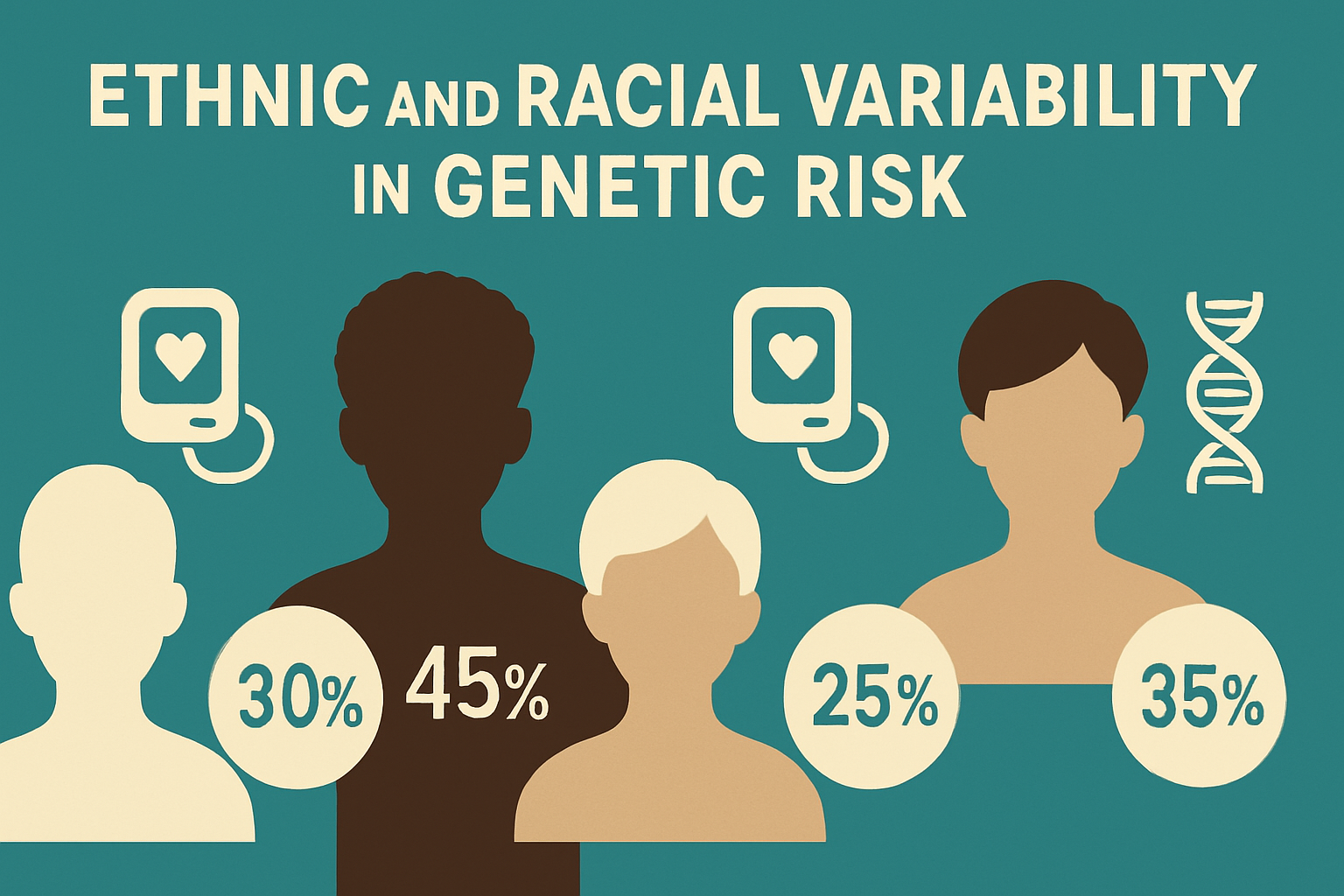
Ethnic and Racial Variability in Genetic Risk
Hypertension does not affect all populations equally. African Americans, for example, experience higher rates of high blood pressure and its complications compared to other racial or ethnic groups. While social determinants of health, including access to care and dietary patterns, play crucial roles, genetics may also contribute to these disparities. Certain gene variants that influence salt sensitivity and vascular reactivity appear more frequently in individuals of African descent.
This variability complicates the question, is hypertension a hereditary disease, by introducing population-specific risk factors. It underscores the need for tailored public health strategies and precision medicine approaches that consider genetic ancestry alongside social and behavioral determinants. Understanding these intersections helps improve the effectiveness of both prevention and treatment strategies in diverse populations.
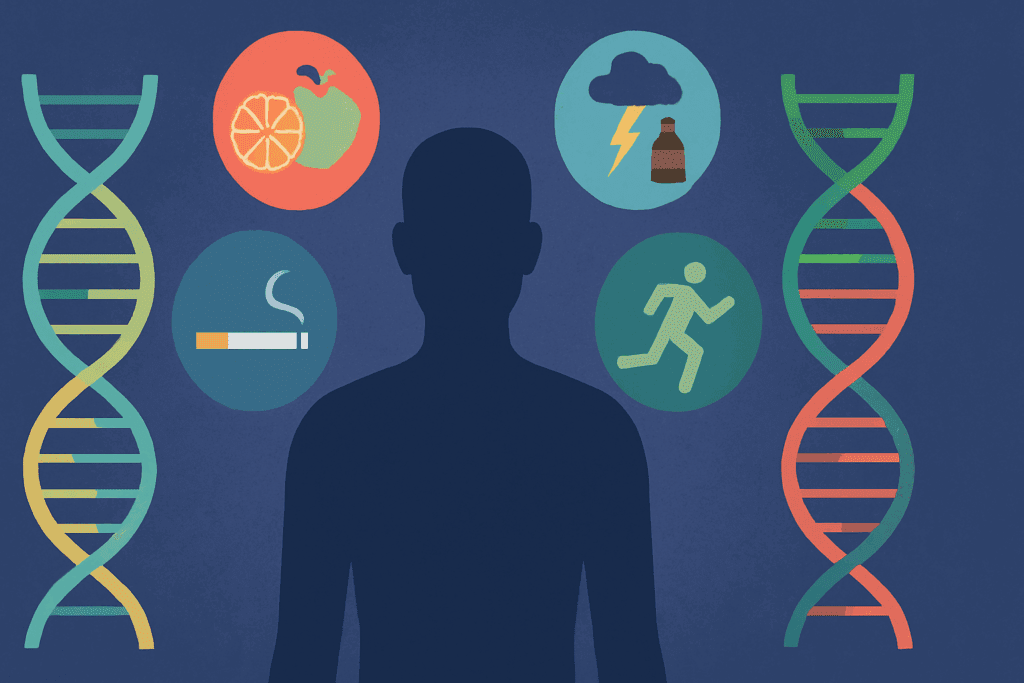
Can Lifestyle Override Genetics?
Although genetics play an undeniable role, they do not constitute destiny. The notion that high blood pressure can be inherited must be balanced with the reality that modifiable lifestyle factors remain powerful tools in prevention and management. Regular physical activity, a diet rich in fruits and vegetables and low in sodium, stress reduction techniques, maintaining a healthy weight, and avoiding tobacco and excessive alcohol can dramatically reduce the risk of developing hypertension—even in those with a strong family history.
The DASH (Dietary Approaches to Stop Hypertension) diet is a prime example of a lifestyle intervention that has proven efficacy. Research indicates that this eating plan can lower systolic blood pressure by up to 11 mmHg, a clinically meaningful result. Moreover, individuals who engage in regular aerobic exercise and mindfulness-based stress reduction report lower blood pressure readings over time. These findings provide hope and empowerment for individuals concerned about hereditary risk.
The Role of Genetic Testing in Hypertension Management
As the science of genomics continues to evolve, the potential for personalized medicine becomes increasingly viable. Genetic testing for hypertension-related variants is already available, although its use remains largely confined to research settings or high-risk cases. Knowing one’s genetic predisposition could one day inform customized prevention plans, medication choices, and lifestyle interventions.
Pharmacogenomics—the study of how genes affect a person’s response to drugs—is a promising field with direct implications for hypertension treatment. For instance, some individuals respond better to certain antihypertensive drugs based on their genetic makeup. Understanding these interactions can lead to more effective, less trial-and-error-based treatment protocols.
However, ethical considerations abound. Issues of privacy, data security, potential discrimination, and psychological stress must be carefully navigated. Additionally, the predictive power of current genetic tests is limited; they can indicate risk, but not guarantee outcomes. For now, integrating family history with clinical assessments and lifestyle evaluations remains the gold standard in managing hypertension risk.
Public Health Implications and Education
If the answer to “can high blood pressure be inherited” is yes—as mounting evidence suggests—then the implications extend beyond the individual to the community and population levels. Public health campaigns should place greater emphasis on educating families about their health history and encouraging early screening. Primary care providers can play a vital role by routinely asking patients about family history and using this information to guide monitoring and prevention strategies.
In schools, workplaces, and community centers, educational programs can empower people with the knowledge to take control of their health. Teaching the signs of hypertension, its risk factors, and the role of genetics can lead to earlier detection and intervention. When individuals understand that having a parent or sibling with high blood pressure increases their own risk, they may be more inclined to adopt preventive behaviors and seek regular medical evaluations.
Rethinking Prevention: From One-Size-Fits-All to Precision Health
Traditional public health strategies often employ a one-size-fits-all approach, offering uniform guidelines regardless of individual risk profiles. However, as research continues to demonstrate that is high blood hereditary in many cases, the need for more nuanced approaches becomes apparent. Precision health—a model that incorporates genetics, lifestyle, and environmental data—may be the future of hypertension prevention and treatment.
Under this model, individuals with a known family history or identified genetic variants could receive earlier and more frequent blood pressure screenings. Their treatment plans might emphasize dietary changes or medications tailored to their specific genetic makeup. Meanwhile, those at lower genetic risk but with adverse lifestyle factors would still benefit from interventions targeted to their needs. The goal is not to replace existing strategies but to enhance them through personalization.
Frequently Asked Questions: Understanding the Hereditary Nature of Hypertension
1. If hypertension runs in my family, does that mean I will definitely develop it?
Having a family history of hypertension increases your risk, but it does not guarantee that you will develop the condition. While research supports that high blood pressure is hereditary to some degree, lifestyle factors play a major role in whether genetic risk translates into an actual diagnosis. For example, maintaining a balanced diet, managing stress, and exercising regularly can offset some of the inherited risk. This is especially true for people who begin healthy practices early in life, before elevated blood pressure sets in. So while the answer to “is blood pressure hereditary” is yes, your choices still have substantial influence.
2. Are there any genetic tests available to determine if I’m at risk for hereditary hypertension?
Yes, there are genetic tests that can identify certain markers associated with increased blood pressure, though they are not yet common in routine clinical settings. These tests are more often used in research or for individuals with a strong family history of cardiovascular disease. They look for gene variants in pathways such as the renin-angiotensin system and salt regulation mechanisms. While they can offer insight, knowing that is hypertension a hereditary disease already helps inform early screening and preventive actions. Genetic testing may become more personalized and accessible as the science matures.
3. Can children or teenagers show signs of inherited high blood pressure?
Yes, pediatric hypertension is an increasingly recognized condition, especially in children with a family history. While it used to be considered rare, recent studies suggest that inherited high blood pressure can manifest earlier than once thought. Risk is heightened when hereditary factors combine with obesity, poor diet, or inactivity. Pediatricians now monitor blood pressure during regular check-ups, especially for children whose parents or close relatives have been diagnosed with hypertension. Understanding that is high blood hereditary informs proactive care from a young age.
4. How do lifestyle and environment interact with inherited risk for hypertension?
Genetics can set the stage, but lifestyle often determines the outcome. A person may carry genes that make them more sensitive to salt or more likely to retain fluid, both of which can raise blood pressure. However, if that individual maintains a heart-healthy diet and stays physically active, they can significantly reduce their risk. The concept that is hypertension hereditary should be balanced with knowledge of epigenetics, which shows that environment and behavior can modify how genes are expressed. In short, inheritance may load the gun, but lifestyle pulls the trigger.
5. Are there differences in hereditary hypertension risk among different populations?
Yes, genetic risk profiles can vary significantly across ethnic and racial groups. For instance, people of African descent are more likely to carry genes that influence salt sensitivity, which can elevate blood pressure. This partially explains why hypertension is more prevalent and often more severe in African American communities. Additionally, socioeconomic factors and access to healthcare often intersect with inherited risk, further complicating outcomes. Understanding that is high blood pressure hereditary in some populations more than others can guide culturally competent care and policy.
6. Can hereditary hypertension skip a generation?
While it may appear that high blood pressure has skipped a generation, it’s more likely that earlier cases went undiagnosed or unmanaged. Hypertension can be asymptomatic for years, especially in its early stages, and previous generations might not have had regular health screenings. It’s also possible that someone inherited a lower genetic load or benefited from healthier lifestyle factors, masking the presence of risk. Inheritance patterns for conditions like hypertension are complex and influenced by both dominant and recessive genes. Asking whether is blood pressure hereditary across generations requires both genetic insight and historical context.
7. Is pregnancy-related high blood pressure linked to hereditary hypertension?
Preeclampsia and gestational hypertension have genetic components that may increase the risk for chronic hypertension later in life. Women who experience high blood pressure during pregnancy are more likely to have close relatives with similar issues. Furthermore, daughters of women who had hypertensive pregnancies are at increased risk themselves, suggesting that is hypertension hereditary in part through maternal lines. Monitoring blood pressure before, during, and after pregnancy becomes even more critical when these familial patterns exist. These findings also support targeted postpartum care for women with a family history.
8. How can someone with hereditary risk for hypertension monitor their health proactively?
For those wondering if is hypertension a hereditary disease and how to respond, regular monitoring is key. Home blood pressure monitors are widely available and can help track changes over time. Keeping a blood pressure journal, especially when combined with wearable fitness trackers, provides actionable insights for both patients and doctors. Additionally, scheduling annual check-ups and advocating for early screening if there’s a strong family history can lead to early detection and better outcomes. This proactive approach acknowledges that can high blood pressure be inherited but need not be inevitable.
9. Are there specific symptoms that suggest hereditary high blood pressure versus lifestyle-related cases?
Unfortunately, high blood pressure tends to present similarly regardless of its cause—typically silent in early stages. However, when high blood pressure emerges in young, otherwise healthy individuals with no clear lifestyle risk factors, a hereditary cause becomes more likely. Sudden spikes in blood pressure, poor response to conventional treatment, or a history of kidney issues may also suggest a genetic component. While is high blood hereditary in such cases is likely, only detailed family history and, in some instances, genetic evaluation can confirm it. The absence of symptoms doesn’t rule out risk, making screening essential.
10. What emerging research is shaping our understanding of hereditary hypertension?
Recent studies in epigenetics and precision medicine are revolutionizing how we view hereditary diseases like hypertension. Scientists are exploring how genes associated with inflammation, circadian rhythm, and gut microbiota may influence blood pressure regulation. There’s also growing interest in how early life exposures—such as maternal stress or nutrient deficiency—affect gene expression related to hypertension. As more data becomes available, the question of whether is hypertension hereditary will be answered with increasing specificity, allowing for more tailored interventions. The future may include personalized dietary plans and medications based on one’s genetic profile, transforming hypertension care entirely.
Final Thoughts: Genetics and Empowerment in Hypertension Prevention
So, is hypertension hereditary? The science says yes—but not inevitably so. While there is no doubt that genetic factors contribute to an individual’s risk, they do not operate in isolation. Understanding that is blood pressure hereditary is only part of the equation; the rest lies in how one chooses to live. From diet and exercise to stress management and regular medical care, many tools are available to help mitigate genetic risk.
In a world where cardiovascular diseases continue to claim millions of lives annually, knowledge truly is power. By understanding your family history, staying informed about genetic research, and making proactive lifestyle choices, you can take meaningful steps to protect your heart health. Genetics may load the gun, but lifestyle pulls the trigger. Through awareness, education, and evidence-based action, it is possible to shift the odds in your favor—even if high blood pressure runs in your family.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Genetic predisposition to higher blood pressure increases coronary artery disease risk
Is High Blood Pressure Genetic? Understanding Familial Hypertension


