Understanding Ischemia and Infarction
Ischemia and infarction are two closely related but distinct medical conditions that play a crucial role in cardiovascular health. Both involve a disruption of blood flow, but their implications and consequences differ significantly. Understanding ischemia vs infarction is essential for recognizing early warning signs, seeking timely medical intervention, and preventing severe complications. In the realm of cardiovascular disorders, these conditions are particularly significant because they can lead to life-threatening events such as heart attacks and strokes. The distinction between ischemia and infarction is not just an academic discussion; it has real-world consequences for diagnosis, treatment, and long-term prognosis.
You may also like: How to Naturally Reverse 20 Years of Arterial Plaque: Science-Backed Strategies for a Healthier Heart
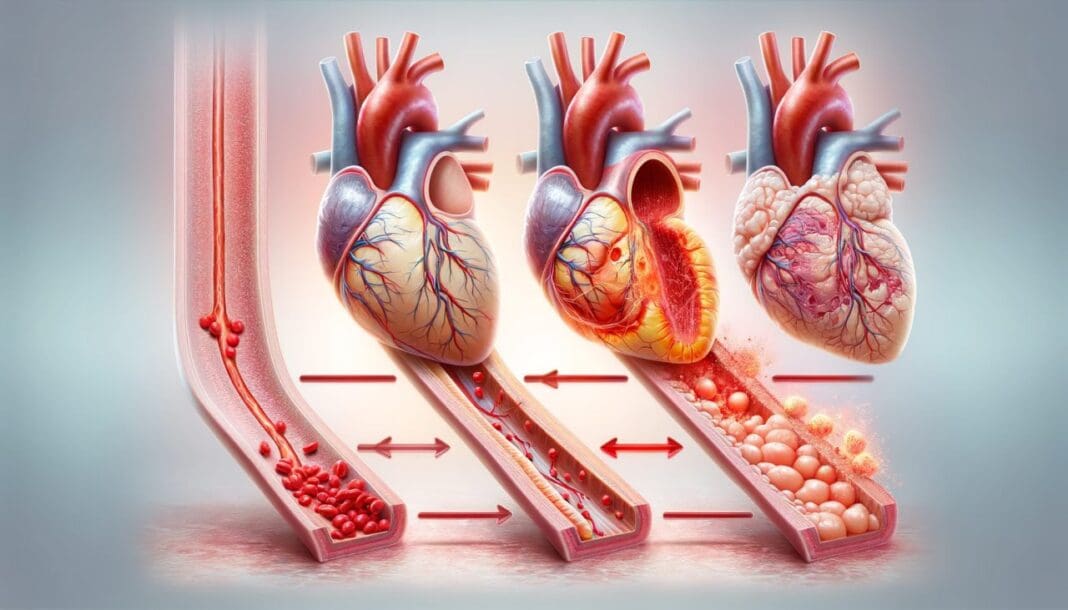
Ischemia is a condition in which blood supply to an organ or tissue is restricted, leading to a deficiency of oxygen and essential nutrients. This restriction can result from a variety of factors, including arterial blockages, vasospasms, or external compression of blood vessels. Ischemia does not always lead to permanent damage; in some cases, the condition can be reversed if blood flow is restored quickly enough. However, prolonged ischemia can result in infarction, which refers to tissue death due to a complete and sustained lack of blood supply. Infarction is often irreversible and can lead to severe health consequences, including organ failure and death. Given these distinctions, it is crucial to explore the causes, symptoms, and treatment options for each condition to fully grasp their implications on cardiovascular health.
What Is Ischemia?
The ischemia definition refers to an inadequate blood supply to an organ or part of the body, especially the heart and brain. Ischemia can be caused by atherosclerosis, blood clots, embolisms, or arterial spasms that lead to a significant reduction in oxygenated blood reaching vital tissues. One of the most common forms is myocardial ischemia, which affects the heart muscle and can lead to chest pain (angina), shortness of breath, and fatigue. Myocardial ischemia symptoms vary depending on the severity of the blockage and the duration of reduced blood flow. Some individuals may experience silent ischemia, a condition in which there are no noticeable symptoms but significant damage may still occur over time.
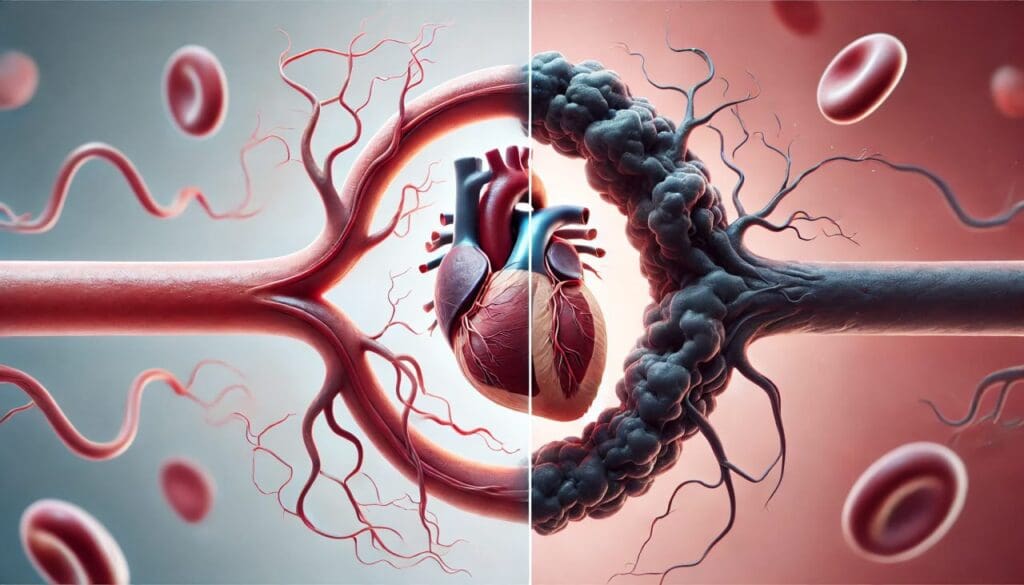
Heart ischemia occurs when there is a partial or complete blockage of the coronary arteries, which supply blood to the heart muscle. This condition is a major component of ischemic heart disease (IHD), also known as coronary artery disease. IHD cardiac complications can lead to serious outcomes such as heart attacks, arrhythmias, and heart failure. The progression of ischemia depends on multiple factors, including the presence of underlying conditions such as diabetes, hypertension, and hyperlipidemia. If untreated, ischemia can cause significant damage to the heart and other organs, making early detection and intervention critical.
What Is Infarction?
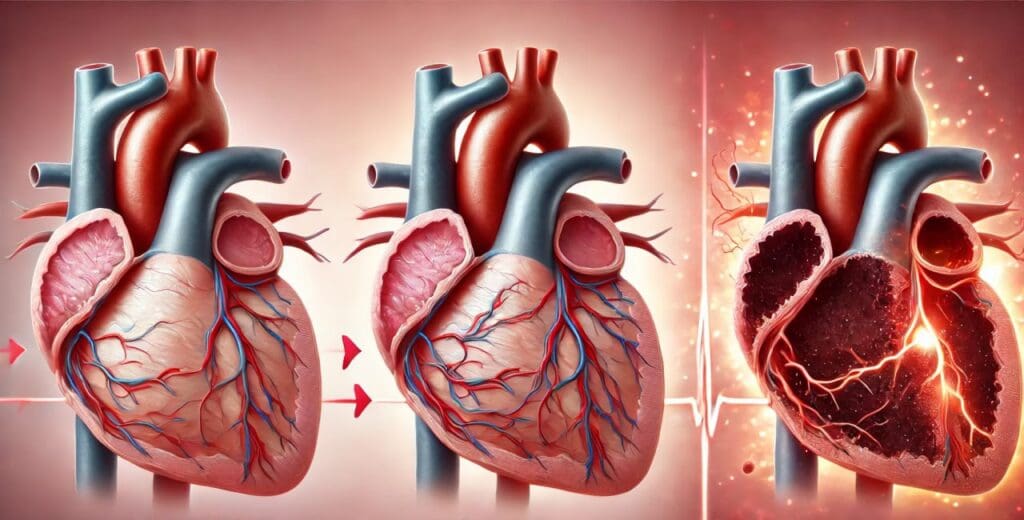
Infarction occurs when prolonged ischemia results in permanent tissue damage or necrosis. This happens when the affected tissue is deprived of oxygen for an extended period, leading to cell death. The most well-known form is myocardial infarction, commonly referred to as a heart attack. Ischemic myocardial infarction occurs when blood flow to a portion of the heart is completely blocked, usually due to a clot forming at the site of an atherosclerotic plaque rupture. Unlike ischemia, which may be reversible if treated promptly, infarction typically results in permanent damage and scarring of the affected tissue.
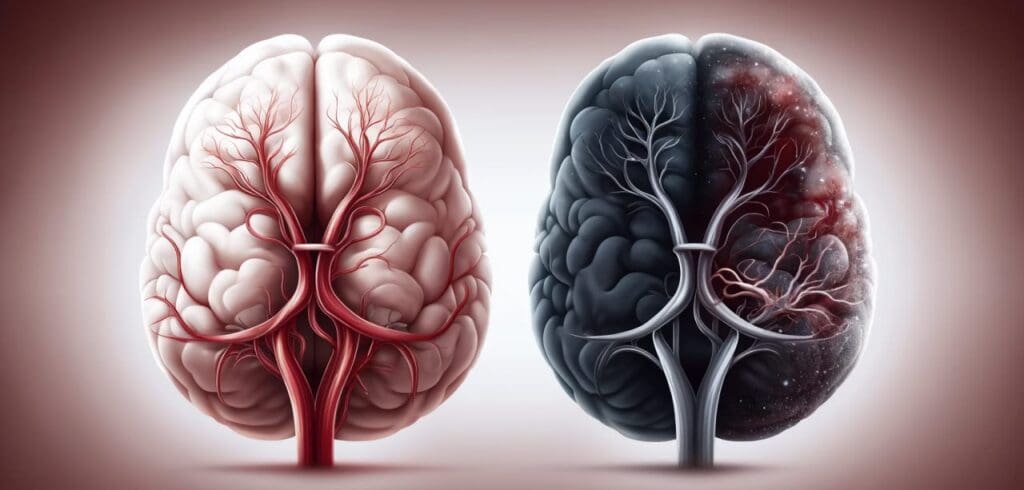
The process of infarction can occur in various organs, including the brain (resulting in ischemic stroke), kidneys, intestines, and extremities. Anterolateral ischemia, inferior ischemia, and inferolateral ischemia are terms used to describe specific regions of the heart that may be affected by infarction. Identifying the location and extent of the infarction helps physicians determine the best course of treatment and the potential for recovery. The severity of infarction depends on factors such as the duration of the blockage, the presence of collateral circulation, and the overall health of the patient.
Ischemia and Myocardial Infarction: Key Differences
While ischemia and myocardial infarction are related, they differ in their impact on the heart. Myocardial infarction vs ischemia can be distinguished by the presence of irreversible damage. Ischemia is a warning sign that blood flow is compromised but can often be corrected if intervention occurs in time. Myocardial infarction, on the other hand, indicates that tissue death has already taken place, making recovery more complex. Early detection of myocardial ischemia symptoms can help prevent infarction and reduce long-term cardiovascular risks.
The differences between ischemia and infarction also have implications for treatment. Ischemia treatment typically involves restoring blood flow through lifestyle modifications, medications, or procedures such as angioplasty and stent placement. In contrast, treatment for infarction focuses on minimizing further damage, restoring circulation, and preventing complications such as heart failure. Understanding how to diagnose ischemic heart disease and differentiate it from infarction is crucial for effective management.
When to Seek Medical Help
Recognizing the signs of ischemia and infarction is critical for seeking timely medical assistance. Heart ischemia symptoms include chest pain, shortness of breath, dizziness, and fatigue. These symptoms may be mild or severe and can vary based on the individual’s overall health and the extent of the blockage. Symptoms of myocardial infarction are often more intense and may include crushing chest pain, radiating pain to the left arm or jaw, nausea, sweating, and a sense of impending doom. Immediate medical attention is required to prevent life-threatening complications.
Many individuals wonder, “How long can cardiac ischemia last before causing irreversible damage?” The answer depends on several factors, including the severity of the blockage and the presence of collateral circulation. In some cases, brief episodes of ischemia, known as transient ischemic attacks (TIAs), resolve without permanent damage. However, prolonged ischemia increases the risk of infarction, making early intervention essential.
Frequently Asked Questions (FAQ) About Ischemia and Infarction
1. What is the primary difference between ischemia and infarction?
The key distinction between ischemia vs infarction lies in the extent of damage caused by reduced blood supply. Ischemia refers to a temporary restriction in blood flow, often leading to tissue hypoxia but not necessarily causing permanent damage. In contrast, infarction occurs when the deprivation of blood supply becomes prolonged, leading to irreversible tissue death. For example, myocardial ischemia may present with transient chest pain, while an ischemic myocardial infarction results in permanent damage to the heart muscle. Identifying ischemia early can help prevent the progression to infarction through timely medical intervention.
2. How does myocardial ischemia affect overall heart function?
Myocardial ischemia occurs when there is insufficient blood flow to the heart muscle, reducing its ability to pump efficiently. This can result in myocardial ischemia symptoms such as chest pain, shortness of breath, and fatigue, which indicate the heart is not receiving adequate oxygen. If left untreated, persistent ischemia can lead to structural changes in the heart, increasing the risk of cardiac ischemic events such as heart attacks and arrhythmias. Patients with IHD cardiac conditions may develop compensatory mechanisms like collateral circulation, where new blood vessels form to bypass blockages, but this is not always sufficient. Preventative measures, including lifestyle changes and medication, are crucial for managing heart ischemia and improving cardiac function.
3. What factors contribute to the development of ischemia?
Several risk factors contribute to ischemia, including atherosclerosis, hypertension, diabetes, and smoking. In ihd heart disease, plaque buildup within the coronary arteries narrows the blood vessels, reducing oxygen-rich blood flow to the heart muscle. Additionally, conditions like arterial vasospasms can trigger sudden episodes of inferior ischemia or anterior ischemia, particularly in individuals with high stress or stimulant use. Sedentary lifestyles and poor dietary habits also accelerate the development of ischemic heart conditions. Identifying and managing these risk factors early can significantly reduce the likelihood of progressing from ischemia to infarction.
4. How can ischemia be reversed, and what treatments are available?
The ability to reverse ischemia depends on early detection and prompt intervention. Ischemia treatment may include lifestyle modifications, medications like antiplatelets and vasodilators, or interventional procedures such as angioplasty. In some cases, ischemia can be reversed by improving blood circulation through exercise and dietary changes that reduce cholesterol levels. However, if left untreated, ischemia may progress to irreversible infarction, necessitating more aggressive interventions such as coronary artery bypass grafting (CABG). The goal of ischemia treatment is to restore normal blood flow and prevent long-term complications like ischemic heart failure.
5. How long can cardiac ischemia last before causing permanent damage?
The duration of cardiac ischemia that leads to permanent damage varies depending on the severity of the blockage and the presence of collateral circulation. In some cases, ischemia can last for several minutes without causing infarction, especially if blood flow is quickly restored. However, prolonged ischemia, lasting 20-40 minutes or more, increases the risk of myocardial infarction vs ischemia progression. In acute settings, timely medical intervention such as thrombolytic therapy can prevent infarction. Recognizing early heart ischemia symptoms and seeking immediate medical attention can be life-saving.
6. What are the early signs and symptoms of ischemic heart disease?
Ischemic heart disease diagnosis often begins with recognizing early symptoms, such as angina, fatigue, and palpitations. These symptoms may become more pronounced during physical exertion when the heart demands increased oxygen supply. In some individuals, ischemic heart disease presents as silent ischemia, where no obvious symptoms are noticed despite significant arterial blockage. Symptoms can also vary depending on the affected coronary region; for example, anterolateral ischemia may manifest with pain radiating to the left arm, while inferolateral ischemia may present as discomfort in the lower chest or back. Seeking medical evaluation at the first sign of cardiac distress can prevent disease progression.
7. How is ischemic heart disease diagnosed?
Physicians use various diagnostic tools to confirm ischemic heart disease diagnosis, including electrocardiograms (ECGs), stress tests, and coronary angiography. ECG readings can detect patterns of inferior ischemia or anterior ischemia, providing insights into which areas of the heart are affected. Cardiac imaging techniques, such as echocardiography and nuclear stress tests, help assess the heart’s function under stress. Blood tests measuring cardiac enzymes can also indicate whether an ischemic event has progressed to infarction. Accurate diagnosis allows for timely intervention and better management of ischemic conditions.
8. Can ischemia lead to heart failure?
Yes, prolonged or recurrent ischemia can contribute to the development of ischemic heart failure. When blood supply to the heart is consistently restricted, myocardial cells become weakened, impairing the heart’s ability to pump efficiently. Over time, this can lead to left ventricular dysfunction, arrhythmias, and reduced cardiac output. In ihd cardiac patients, ischemic heart failure often develops gradually as a result of chronic ischemic episodes. Managing ischemia through medication, lifestyle changes, and surgical interventions can reduce the risk of heart failure and improve long-term prognosis.
9. What lifestyle modifications can help manage ischemia and myocardial infarction risk?
Adopting a heart-healthy lifestyle is crucial for individuals at risk of ischemia and myocardial infarction. Regular physical activity enhances circulation and strengthens the heart, reducing the likelihood of ischemic events. Dietary changes, such as consuming omega-3-rich foods and avoiding trans fats, can help lower cholesterol levels and prevent arterial blockages. Stress management techniques, including mindfulness and deep breathing exercises, may reduce the risk of stress-induced anterolateral ischemia or vasospasm-related ischemic episodes. Quitting smoking and maintaining optimal blood pressure levels further decrease the chances of progressing from ischemia to infarction. These lifestyle modifications play a pivotal role in preventing and managing ischemic heart disease.
10. Are there emerging treatments for ischemic heart disease?
Advancements in medical research are continually improving the treatment landscape for ischemic heart conditions. Novel therapies, such as regenerative medicine using stem cells, show promise in repairing ischemic myocardial tissue. Gene therapy is also being explored to enhance the development of collateral blood vessels, potentially reversing ischemia without surgical intervention. Innovative devices like bioresorbable stents are being developed to improve long-term outcomes for patients with ihd heart disease. Additionally, artificial intelligence and machine learning are enhancing early detection methods, allowing for more personalized ischemia treatment approaches. As research progresses, the future of ischemic heart disease management is expected to become more precise and effective.
Conclusion: Understanding and Managing Ischemia and Infarction
In summary, ischemia vs infarction represents a critical distinction in cardiovascular health. Ischemia involves a temporary reduction in blood flow, which, if not corrected, can lead to infarction and irreversible tissue damage. Recognizing myocardial ischemia symptoms, understanding ischemic heart disease diagnosis, and seeking prompt medical intervention can make a significant difference in preventing heart attacks and other severe complications. Can ischemia be reversed? In many cases, yes—if detected early and managed appropriately. However, once infarction occurs, treatment focuses on preventing further damage and improving overall cardiovascular function. By staying informed and proactive, individuals can take control of their heart health and reduce the risk of life-threatening events.
cardiac blood flow restriction, coronary artery blockage, cardiovascular ischemic conditions, myocardial oxygen deprivation, heart circulation disorders, arterial plaque buildup, cardiac perfusion issues, vascular disease symptoms, reduced heart oxygen supply, cardiovascular risk factors, coronary thrombosis, heart muscle damage, chronic angina management, silent heart conditions, blood clot in arteries, heart rhythm disturbances, ischemic cardiovascular care, advanced cardiac imaging, early heart disease detection, heart health maintenance
Further Reading:
What is the difference between myocardial ischemia and myocardial infarction?
Myocardial ischemia/reperfusion: Translational pathophysiology of ischemic heart disease
Myocardial ischemia and infarction: growth of ideas
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.