Respiratory infections, including the flu, represent a significant burden on global health systems every year. From seasonal influenza outbreaks to more persistent infections like the common cold, bronchitis, and even pneumonia, these illnesses continue to affect millions of individuals worldwide. Understanding the mechanisms behind these infections, coupled with effective strategies for prevention from flu and related respiratory conditions, is vital for maintaining public health and individual well-being. As we delve into the various dimensions of flu prevention, we will explore scientifically supported practices, lifestyle interventions, and real-world applications that can significantly reduce the risk of contracting and spreading respiratory illnesses.
You may also like: Pulmonary Artery Health: Understanding Its Role in Circulation and Common Disorders
Understanding Influenza and Respiratory Infections
Influenza, commonly referred to as the flu, is a contagious respiratory illness caused by influenza viruses that infect the nose, throat, and sometimes the lungs. It can result in mild to severe illness, and at times, can lead to hospitalization or even death, particularly in vulnerable populations such as young children, the elderly, and individuals with compromised immune systems. While influenza tends to garner the most attention due to its potential for widespread outbreaks and significant public health implications, it is only one of many respiratory infections.
Common respiratory infections also include rhinoviruses (which cause the common cold), respiratory syncytial virus (RSV), parainfluenza viruses, adenoviruses, and coronaviruses. These infections often share overlapping symptoms such as coughing, sneezing, sore throat, nasal congestion, and fever, which can make initial diagnosis challenging. Additionally, bacterial infections like Streptococcus pneumoniae may complicate or follow viral infections, adding to the severity and duration of illness. Understanding the broad landscape of respiratory pathogens is essential when discussing how to prevent influenza and other similar infections.
The Importance of Prevention from Flu in Public Health
Preventing influenza and other respiratory infections is not only beneficial for individual health but is also crucial from a broader public health perspective. Influenza epidemics strain healthcare systems every year, leading to increased doctor visits, hospital admissions, and even temporary shortages in medical supplies. Moreover, during peak flu season, the economic toll of lost productivity due to absenteeism can be profound. Therefore, effective prevention from flu not only reduces personal risk but also alleviates pressure on medical infrastructure and supports a more resilient society.
From a medical standpoint, prevention is far superior to treatment, especially given the limitations of antiviral medications and the evolving resistance patterns of certain viruses. Influenza viruses mutate rapidly, which can render specific treatments or vaccines less effective if not properly updated. Consequently, a multi-faceted approach to prevention becomes indispensable. This involves public education, access to preventive tools such as vaccines, personal hygiene practices, and broader community-level interventions like social distancing and environmental sanitation during outbreaks.
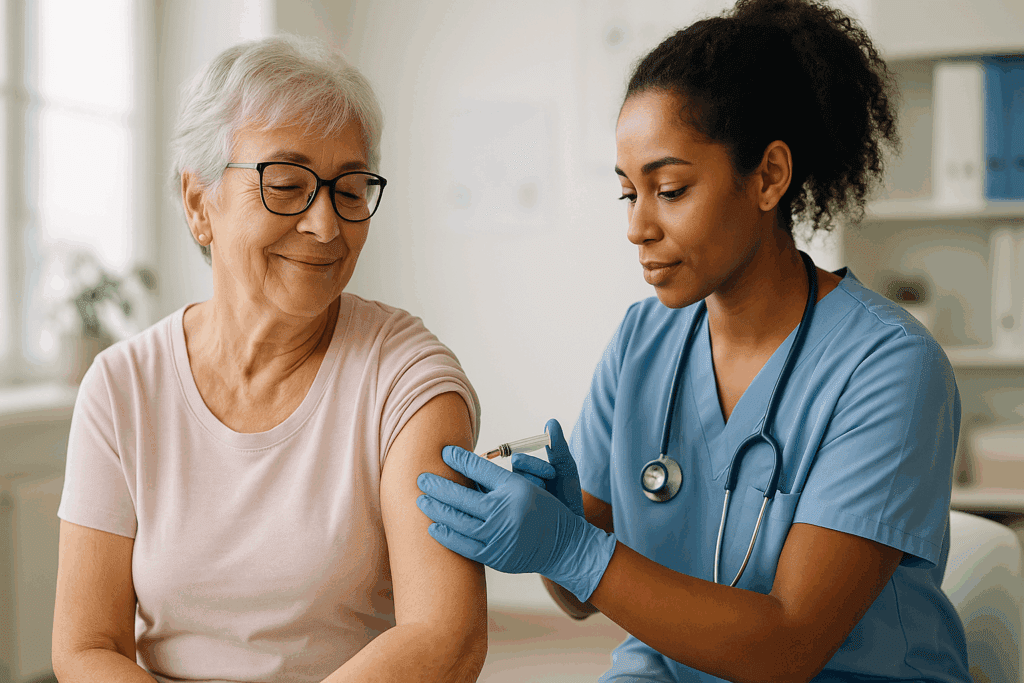
Vaccination: The Cornerstone of Flu Prevention
Among the most effective strategies for preventing influenza is vaccination. The flu vaccine, developed annually based on predictions about the most prevalent strains, significantly reduces the risk of illness and severity of symptoms for those who do get infected. While no vaccine offers 100% protection, the influenza vaccine has consistently demonstrated efficacy in reducing flu-related complications, hospitalizations, and deaths, particularly among high-risk populations.
Vaccination also plays a crucial role in establishing herd immunity, which protects individuals who are unable to receive the vaccine due to age, medical conditions, or allergies. By lowering the overall incidence of flu in the community, vaccination helps to prevent transmission to vulnerable groups. Annual vaccination is strongly recommended for most individuals over the age of six months, especially those working in healthcare, education, or other high-contact professions.
It’s also worth noting that advancements in vaccine technology have led to improved formulations, such as high-dose vaccines for seniors and cell-based or recombinant vaccines that offer alternative options for those with egg allergies. As ongoing research continues to refine vaccine efficacy and delivery methods, the importance of widespread immunization in prevention from flu remains paramount.

Daily Habits that Strengthen Respiratory Defense
In addition to vaccination, everyday behaviors and lifestyle choices significantly influence one’s susceptibility to respiratory infections. One of the most basic yet powerful actions is regular handwashing with soap and water for at least 20 seconds. This practice reduces the likelihood of virus transmission via contact with contaminated surfaces, which is a common route of infection.
Respiratory hygiene is equally important. Covering the mouth and nose with a tissue or elbow when coughing or sneezing helps prevent the spread of infectious droplets. Avoiding close contact with individuals displaying flu-like symptoms and maintaining physical distance during peak infection seasons are also effective methods. Furthermore, disinfecting commonly touched surfaces such as doorknobs, phones, and keyboards adds another layer of protection.
Diet and hydration also play key roles in immune health. A diet rich in fruits, vegetables, whole grains, and lean proteins supports the immune system through essential vitamins and minerals, such as vitamin C, vitamin D, and zinc. Staying well-hydrated helps maintain mucosal barriers in the respiratory tract, which serve as the body’s first line of defense against pathogens. Lifestyle choices such as regular exercise, sufficient sleep, and stress management further contribute to immune resilience, forming a comprehensive approach to how to prevent influenza and other infections.

Environmental and Workplace Strategies for Flu Prevention
Public and private spaces alike can benefit from targeted strategies to minimize the spread of flu and respiratory infections. In workplaces, promoting a culture that encourages employees to stay home when ill can significantly reduce the risk of outbreaks. Employers should consider implementing flexible sick leave policies and remote work options during peak flu season.
Improved ventilation in indoor spaces helps dilute airborne pathogens, reducing transmission risk. This is particularly relevant in schools, offices, and healthcare facilities where large numbers of people gather. The use of high-efficiency particulate air (HEPA) filters, open windows, and HVAC system maintenance are practical measures that support air quality.
Educational campaigns that remind individuals about the symptoms of influenza and the importance of early intervention can also foster a more proactive health culture. Posters, digital displays, and public service announcements are effective tools for spreading awareness about prevention from flu. By integrating these efforts into community and workplace infrastructures, the collective risk of respiratory outbreaks can be substantially lowered.

The Role of Masks and Personal Protective Equipment (PPE)
The COVID-19 pandemic brought widespread attention to the role of masks and personal protective equipment in controlling respiratory illnesses. Although public use of masks during flu season was not a widespread practice before the pandemic, there is growing evidence supporting their utility in reducing transmission.
Wearing a well-fitted mask, particularly in crowded or enclosed spaces, can block respiratory droplets that may carry influenza or other viruses. Masks are especially important for individuals who are symptomatic, as they can contain the spread of infection to others. In healthcare and caregiving settings, the use of N95 respirators and other forms of PPE remains a standard for preventing transmission.
Importantly, mask-wearing should not replace other preventive measures but should be used in conjunction with them. When combined with vaccination, hand hygiene, and physical distancing, masks offer an added layer of defense. Public acceptance of mask usage during flu season continues to evolve, and normalized adoption could become a valuable tool in long-term prevention strategies.
Boosting Immunity Through Nutritional and Supplemental Support
Strengthening the immune system is an essential component of preventing flu and other respiratory infections. While no supplement can guarantee immunity, a well-nourished body is better equipped to fend off pathogens and recover from illness more efficiently. Nutritional strategies should focus on ensuring adequate intake of immune-supporting nutrients.
Vitamin D has emerged as a critical nutrient in respiratory health, with research indicating that deficiency may increase susceptibility to infections, including the flu. During winter months, when sunlight exposure is limited, supplementation may be necessary to maintain optimal levels. Similarly, zinc has been shown to support immune cell function and may reduce the duration and severity of respiratory infections.
Probiotics, which support gut health, also play an indirect role in immune modulation. Since a significant portion of the immune system resides in the gut, maintaining a balanced microbiome contributes to overall immune resilience. While individual responses to supplements vary, consulting with a healthcare provider can help determine appropriate choices based on personal health status and dietary needs.
Understanding How to Prevent Influenza in High-Risk Populations
Certain groups are more vulnerable to complications from influenza and require tailored preventive strategies. These include individuals over 65, young children under the age of five, pregnant women, and those with chronic health conditions such as asthma, diabetes, or heart disease. For these populations, early vaccination is especially important, and additional precautions should be taken during flu season.
Healthcare providers should be vigilant in monitoring high-risk patients for early signs of influenza and be prepared to administer antiviral medications when necessary. These medications are most effective when started within 48 hours of symptom onset and can reduce the severity and duration of illness. In some cases, prophylactic use of antivirals may be considered for high-risk individuals exposed to the flu.
Caregivers and household members of high-risk individuals should also be vaccinated and practice enhanced hygiene to minimize the risk of transmission. In long-term care facilities and hospitals, strict infection control protocols must be followed to prevent outbreaks. Understanding how to prevent influenza in these settings is not only about individual actions but also involves institutional preparedness and policy.
Seasonal Trends and Global Perspectives on Flu Prevention
Influenza exhibits seasonal patterns, with outbreaks commonly occurring in the colder months of the year. This seasonality is driven by factors such as indoor crowding, reduced sunlight, and lower humidity, all of which facilitate viral transmission. Recognizing these trends allows public health officials to time vaccination campaigns and awareness efforts effectively.
Globally, flu prevention strategies vary based on local resources, infrastructure, and healthcare access. In low- and middle-income countries, limited access to vaccines and medical care poses significant challenges. International organizations such as the World Health Organization (WHO) play a crucial role in coordinating global surveillance, vaccine distribution, and public education campaigns.
Emerging research on universal flu vaccines, which aim to provide longer-lasting protection against multiple strains, holds promise for the future. In the meantime, continued investment in research, infrastructure, and equitable healthcare delivery remains critical to improving prevention from flu worldwide.
Integrating Flu Prevention into Everyday Life
Creating a sustainable approach to flu prevention involves embedding healthy behaviors into daily routines. Teaching children proper hygiene from an early age, maintaining regular check-ups with healthcare providers, and staying informed about local flu activity are all part of a proactive health strategy. Schools and community centers can serve as hubs for education and resource distribution, helping to normalize prevention efforts.
Technology also offers new avenues for flu prevention. Mobile apps that track symptoms, notify users of local outbreaks, or provide vaccination reminders can empower individuals to make informed decisions. Digital health platforms enable telemedicine consultations, reducing the need for in-person visits and lowering exposure risk during flu season.
Cultivating a culture that values preventive health requires ongoing education, accessible resources, and supportive policies. By making flu prevention a habitual practice rather than a seasonal response, individuals and communities can build resilience against recurring respiratory threats.
Frequently Asked Questions: Advanced Insights on Flu Prevention and Respiratory Health
How can behavioral psychology be used to support prevention from flu in communities?
Behavioral psychology offers powerful tools for designing interventions that encourage consistent flu prevention behaviors across different populations. One key principle is the use of social norms—when people see others practicing hand hygiene or wearing masks, they are more likely to adopt the same behavior. Visual cues, such as strategically placed reminders in schools, offices, and public transport, can also reinforce daily practices like handwashing or cough etiquette. Additionally, leveraging behavioral nudges through mobile apps or personalized messages can enhance adherence to vaccination schedules and health check-ins. Understanding the psychological barriers to behavior change—such as perceived invincibility among younger adults—allows public health campaigns to frame messages that resonate more effectively and result in sustained behavioral shifts supporting long-term prevention from flu.
What emerging technologies could transform how to prevent influenza in the future?
Several promising technologies are poised to revolutionize how to prevent influenza in both clinical and everyday contexts. Wearable health devices that track early biomarkers—such as elevated body temperature or heart rate variability—may enable real-time flu detection before symptoms fully emerge, prompting early isolation or treatment. AI-driven surveillance systems that analyze trends in social media, pharmacy purchases, and hospital admissions can help forecast outbreaks and direct resources accordingly. Additionally, next-generation flu vaccines that use mRNA platforms—similar to those used for COVID-19—are being developed to offer broader, longer-lasting protection with faster production timelines. These innovations will not only make prevention more efficient but also personalize strategies for those most at risk of severe illness. Integrating such tools into public health systems could redefine the landscape of prevention from flu.
Are there long-term immunity strategies beyond vaccination that support prevention from flu?
Yes, while annual flu vaccination remains essential, there are complementary long-term immunity strategies that contribute to sustained protection. Regular exposure to diverse microbial environments—such as spending time outdoors, gardening, or living with pets—can train the immune system to be more adaptable and less reactive to new pathogens. Intermittent fasting and exercise have also shown promise in modulating immune responses and reducing systemic inflammation, which plays a role in how the body reacts to viral infections. Additionally, mindfulness and stress-reduction practices may decrease cortisol levels, which when chronically elevated, can suppress immune function. These lifestyle-based approaches, when combined with medical prevention from flu, form a holistic strategy for building resilience against respiratory illnesses over time.
How does climate and air quality influence how to prevent influenza in urban populations?
Urban settings often present unique challenges when considering how to prevent influenza, particularly due to factors like poor air quality and population density. Polluted air can damage the mucosal linings of the respiratory tract, making individuals more susceptible to viral invasion. During colder months, increased time spent indoors with limited ventilation facilitates the transmission of airborne viruses. Green infrastructure, such as planting urban trees and promoting clean energy, can help reduce pollution and support respiratory health. Cities can also invest in advanced HVAC systems with HEPA filtration in public buildings to mitigate airborne pathogen spread. Addressing environmental factors in tandem with personal behaviors and vaccination programs is a critical step in creating an ecosystem that supports prevention from flu in high-density regions.
Can workplace culture play a critical role in effective flu prevention strategies?
Absolutely. Workplace culture profoundly impacts the effectiveness of flu prevention strategies, particularly through policies, communication, and peer behavior. When employers actively promote sick leave without penalizing employees, it reduces the likelihood of contagious individuals remaining at work. Encouraging flexible work-from-home policies during peak flu seasons or providing on-site flu vaccination clinics are other effective measures. Moreover, leadership behavior sets the tone—when managers model preventive behaviors like mask-wearing or hand sanitizing, employees are more likely to follow suit. Incorporating flu awareness into wellness initiatives, reward programs, or internal communication channels fosters an environment where prevention from flu is seen as a shared responsibility rather than an individual burden.
What role does travel play in global influenza dynamics, and how can travelers reduce their risk?
Travel significantly contributes to the global spread of influenza, especially during peak holiday seasons or international events where people from various regions converge. Air travel, in particular, increases exposure due to close contact in enclosed spaces and the recirculation of cabin air. To reduce risk, travelers should get vaccinated at least two weeks before departure, especially if heading to regions with known outbreaks. Wearing masks, using hand sanitizer, and avoiding unnecessary contact with surfaces in high-traffic areas like airports and train stations can also help. Monitoring local health advisories and carrying a small travel health kit that includes antiviral medication (when prescribed), masks, and disinfecting wipes offers an added layer of protection. Recognizing the interconnected nature of flu transmission, conscientious travel habits are essential components of modern strategies for how to prevent influenza globally.
How do flu prevention strategies differ in immunocompromised individuals?
Immunocompromised individuals require more tailored flu prevention approaches due to their heightened vulnerability to complications. Standard vaccination may yield a weaker immune response in these populations, prompting the use of high-dose or adjuvanted vaccines designed to elicit stronger immunity. Antiviral prophylaxis, taken under medical supervision during peak flu season or after exposure, is sometimes recommended. Beyond pharmacological interventions, immunocompromised individuals benefit from limiting exposure by avoiding crowded spaces, practicing rigorous hand hygiene, and ensuring household members are vaccinated. Caregivers and family members should also adopt enhanced prevention from flu protocols to create a safer living environment. Coordinated care involving specialists can ensure that preventive strategies align with the individual\u2019s broader health management plan.
Why is public trust essential in broad adoption of prevention from flu initiatives?
Public trust is foundational to the success of any large-scale flu prevention initiative. When people trust health authorities, they are more likely to get vaccinated, follow public guidance, and engage in proactive behaviors like staying home when sick. Conversely, misinformation and inconsistent messaging can lead to skepticism, reduced compliance, and increased risk of outbreaks. Transparent communication, clear explanations of the science behind recommendations, and culturally sensitive outreach are critical in building and maintaining trust. Engaging community leaders, educators, and even social influencers to disseminate accurate information can help bridge the gap between public health agencies and everyday citizens. Trust not only facilitates individual behavior change but also cultivates a social contract that makes community-wide prevention from flu more achievable.
What are some underutilized but effective strategies for how to prevent influenza?
While vaccination and hand hygiene are well known, several underutilized strategies can enhance efforts in how to prevent influenza. One such approach is the strategic use of antiviral medications as a preventive measure, particularly in outbreak settings like long-term care facilities. Ultraviolet germicidal irradiation (UVGI) is another underrecognized method; it uses UV light to sterilize air and surfaces in high-risk environments like hospitals or schools. Incorporating adaptive ventilation systems that respond to occupancy levels can optimize air quality in shared spaces. Another promising strategy is cross-training staff in critical sectors (like healthcare and emergency services) to ensure operational continuity even during outbreaks. By embracing these complementary strategies, communities can achieve a more layered and resilient form of prevention from flu.
How can schools and educational institutions serve as hubs for flu prevention education?
Schools are ideal environments for instilling lifelong health behaviors that support flu prevention. By integrating modules on personal hygiene, disease transmission, and community health into curricula, educators can empower students with actionable knowledge. Hosting annual vaccination drives in partnership with local health departments increases access while normalizing the practice among families. Interactive programs—such as gamified hygiene challenges or classroom-based peer teaching—can make flu prevention more engaging and memorable. Additionally, schools can serve as information bridges to parents by distributing flu season updates, guidelines, and resources through newsletters and digital platforms. When children bring home flu prevention knowledge, it creates a ripple effect that strengthens entire households and communities. This holistic model of education-centered health promotion enhances long-term strategies for how to prevent influenza.
Conclusion: Building a Resilient Future Through Proactive Prevention from Flu
The path to a healthier future hinges on a collective commitment to disease prevention, particularly in the realm of respiratory infections. Prevention from flu is not simply a matter of avoiding seasonal illness; it is a comprehensive strategy that encompasses vaccination, daily hygiene, environmental controls, and personal health optimization. Each action, no matter how small, contributes to a larger web of protection that shields not only the individual but also the broader community.
Understanding how to prevent influenza involves a dynamic interplay of science, behavior, and policy. As new viruses emerge and old ones evolve, our preventive tactics must also adapt. The lessons learned from past flu seasons, and from global health crises like the COVID-19 pandemic, reinforce the importance of proactive, evidence-based approaches.
Ultimately, the key to lasting flu prevention lies in an integrated strategy that brings together medical advancements, public awareness, and personal responsibility. When these elements align, the burden of respiratory infections can be significantly reduced, paving the way for healthier communities and a more resilient global health landscape.