Introduction: The Transformative Promise of Experimental Cancer Treatment
Cancer remains one of the most formidable medical challenges of the 21st century, affecting millions of lives globally and placing an immense burden on individuals, families, and healthcare systems. Despite remarkable advancements in conventional therapies such as surgery, chemotherapy, radiation, and immunotherapy, many cancers persist as difficult to treat, particularly in advanced or drug-resistant stages. In response, researchers around the world have intensified their pursuit of novel therapeutic avenues—ushering in a new era of innovation grounded in experimental treatment. From cutting-edge gene-editing tools to personalized immunotherapies, the domain of experimental cancer treatment is rapidly expanding, offering new hope to patients and clinicians alike. This article explores the most promising advances in experimental cancer treatment, emphasizing the latest research findings and the evolving scientific, ethical, and clinical landscape shaping these developments.
You may also like: Cancer Research Breakthroughs: How Modern Advancements Are Transforming Treatment
Redefining Cancer Therapy: The Role and Scope of Experimental Treatment
Experimental treatment refers to medical therapies that are under investigation and have not yet received full regulatory approval for widespread clinical use. In the context of oncology, these include a range of modalities—targeted therapies, genetic engineering techniques, immunologic interventions, nanotechnology applications, and more—often evaluated through early-phase clinical trials. The objective is to determine their safety, efficacy, and potential superiority to standard care. While experimental treatments are not without risk, they also represent the vanguard of hope, especially for patients with refractory or metastatic cancers who have exhausted conventional options. Understanding how these interventions are developed, tested, and regulated is critical to appreciating their significance and limitations.
The Evolution of Experimental Cancer Treatment in Modern Oncology
The evolution of cancer therapy reflects a trajectory of deepening biological understanding and increasingly precise intervention. Early efforts focused on indiscriminate cell killing, as seen in the era of cytotoxic chemotherapy. Today, the trend is toward targeting molecular drivers of malignancy with ever-increasing specificity. Experimental treatments now encompass modalities capable of modulating immune responses, editing defective genes, and delivering drugs directly to tumor sites with unprecedented accuracy. This shift is not merely technological—it is philosophical. It acknowledges the heterogeneity of cancer and the need for individualized, adaptive approaches. Research institutions, biotech firms, and academic centers are forming global alliances to accelerate innovation, share data, and minimize duplication. This cooperative momentum has dramatically expanded the pipeline of experimental cancer treatment options currently in development or under clinical evaluation.
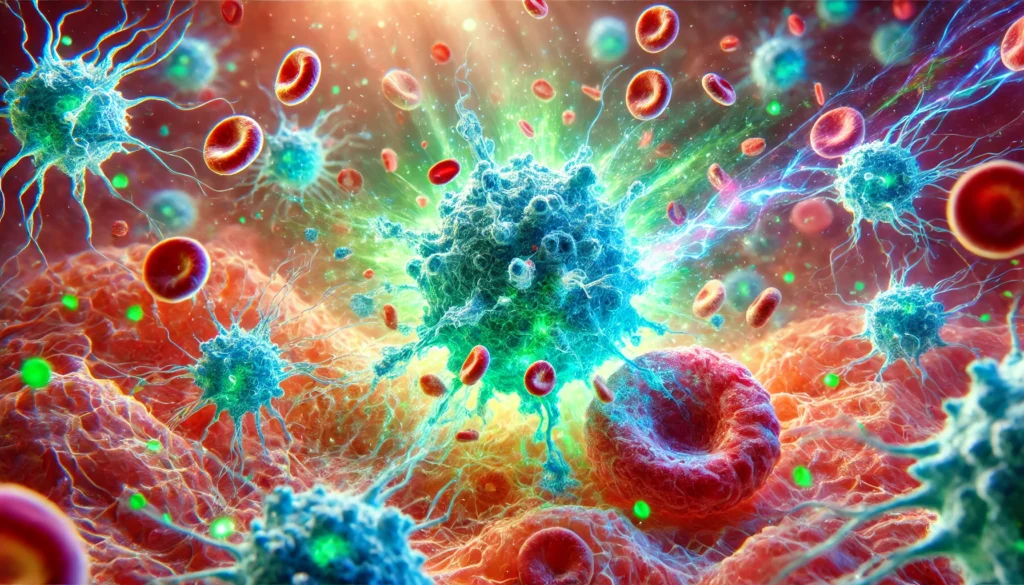
Advances in Immunotherapy: Pushing the Frontiers of Immune-Based Experimental Treatment
Among the most transformative breakthroughs in cancer research has been the rise of immunotherapy—a modality that leverages the body’s immune system to target and destroy cancer cells. While several immunotherapies, such as checkpoint inhibitors and CAR T-cell therapy, have achieved regulatory approval for specific indications, many others remain in the realm of experimental treatment. Current research is expanding this frontier by investigating next-generation CAR T-cell constructs, bispecific T-cell engagers (BiTEs), tumor-infiltrating lymphocyte (TIL) therapies, and dendritic cell vaccines. These approaches aim to enhance antigen specificity, reduce off-target effects, and overcome resistance mechanisms. In particular, experimental cancer treatment involving engineered T cells that recognize neoantigens—unique tumor-specific mutations—holds promise for enhancing efficacy while minimizing collateral damage to healthy tissue. Preliminary trial results have demonstrated durable responses in hematologic malignancies and are now being tested in solid tumors.
Harnessing the Microbiome: The Unexpected Ally in Experimental Oncology
The human microbiome has emerged as an unexpected yet powerful modulator of cancer therapy response. Recent studies suggest that specific gut bacteria can influence the efficacy of immunotherapy, enhance drug metabolism, and even produce anticancer metabolites. Experimental treatment strategies now include microbiome modulation through probiotics, fecal microbiota transplantation, and engineered bacterial therapeutics. For example, trials are underway to determine whether microbiome-enhancing interventions can convert non-responders into responders to immune checkpoint inhibitors. The mechanisms remain under investigation, but the integration of microbiome science into experimental cancer treatment offers a novel and potentially synergistic avenue of intervention. This area exemplifies how seemingly peripheral biological systems can play a central role in therapeutic innovation.
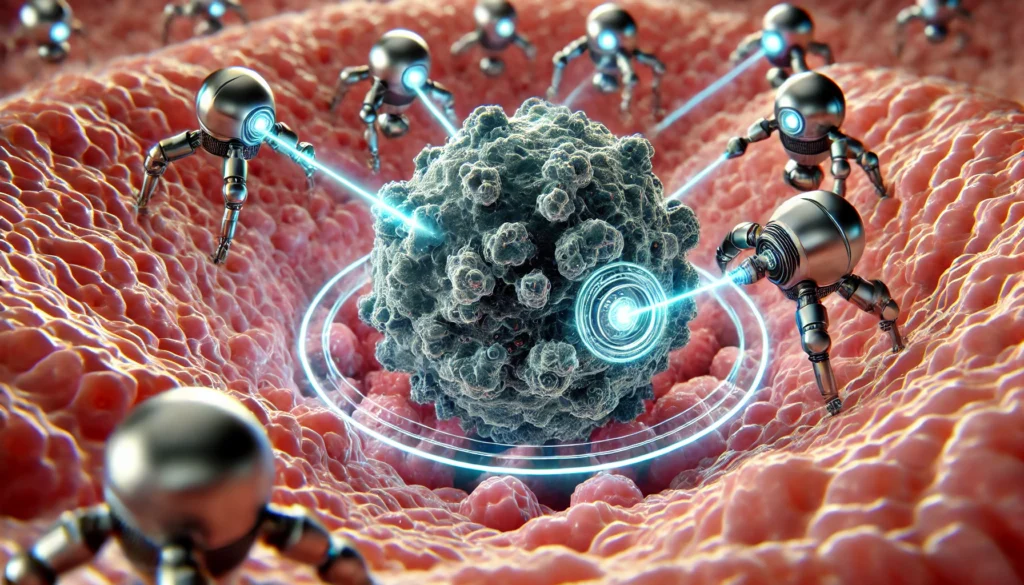
Nanomedicine in Oncology: Precision Delivery Through Engineered Nanoparticles
Nanomedicine represents one of the most exciting developments in experimental cancer treatment. By engineering nanoscale drug carriers, researchers can improve pharmacokinetics, enhance tumor specificity, and reduce systemic toxicity. Liposomes, dendrimers, polymeric micelles, and exosomes are among the many platforms under investigation. These nanoparticles can be functionalized with targeting ligands, imaging agents, or stimuli-responsive components to optimize delivery and track treatment in real time. Several early-phase trials have shown encouraging results in solid tumors, particularly when delivering chemotherapy, siRNA, or immunomodulatory agents. One of the most promising applications is the delivery of CRISPR-Cas9 systems using lipid nanoparticles, potentially enabling gene editing directly at tumor sites. While regulatory hurdles remain, the convergence of material science and oncology could profoundly alter therapeutic strategies.
Overcoming Drug Resistance: Strategies in Experimental Cancer Treatment
Drug resistance remains a central obstacle in oncology. Experimental cancer treatment strategies are increasingly focused on understanding and counteracting resistance mechanisms, whether through combination therapy, epigenetic modulation, or pathway reactivation. For instance, dual blockade of parallel signaling cascades (e.g., PI3K and MEK inhibitors) has shown promise in preclinical models. Additionally, efforts to re-sensitize tumors via histone deacetylase inhibitors or DNA methyltransferase inhibitors are underway. Some experimental treatments aim to target tumor plasticity itself, exploiting vulnerabilities that emerge during phenotypic switching. Adaptive therapy models, which dynamically adjust dosing based on tumor response, are also being explored as a means of forestalling resistance. These innovations reflect a shift from reactive to anticipatory treatment paradigms.
The Future of Experimental Cancer Treatment: Toward a Personalized, Integrated Paradigm
Looking ahead, the future of experimental treatment in oncology lies in convergence: the integration of genomic data, real-time analytics, immunologic profiling, and systems biology to inform therapy design. Multi-omic platforms are enabling a holistic view of tumor biology, guiding not only treatment selection but also timing, dosing, and sequencing. Experimental cancer treatment is increasingly framed not as a last resort but as a proactive strategy—part of a continuous learning loop embedded in clinical care. The advent of decentralized trials, wearable biosensors, and telemedicine is also transforming how experimental treatments are administered and monitored. As innovation accelerates, maintaining rigorous scientific standards while fostering accessibility and transparency will be critical to sustainable progress.
Frequently Asked Questions: Promising Advances in Experimental Cancer Treatment
What distinguishes experimental cancer treatment from off-label drug use? Experimental cancer treatment refers to therapies currently under investigation and not yet approved for general clinical use, while off-label drug use involves approved medications prescribed for conditions outside their original indication. Although both practices are considered when conventional therapies fail, experimental treatment is typically administered within the confines of clinical trials. Off-label use is often based on emerging clinical data or case reports rather than formal trial protocols. Patients participating in experimental cancer treatment trials are monitored under rigorous guidelines, while off-label use is more physician-guided. The distinction matters significantly when assessing risks, legal considerations, and access to supportive care.
Can patients participate in experimental treatment without enrolling in a clinical trial? Yes, in some cases, patients may access experimental treatment through mechanisms such as expanded access or compassionate use programs. These pathways are typically reserved for individuals with life-threatening conditions who cannot participate in clinical trials due to exclusion criteria, geographical limitations, or disease progression. Regulatory bodies like the FDA in the United States evaluate these requests on a case-by-case basis to ensure that patient safety is prioritized. While not as structured as a trial, expanded access still involves oversight and informed consent. Patients and physicians must navigate ethical and logistical challenges when pursuing this route, often relying on advocacy and institutional support to gain access.
How does experimental cancer treatment affect quality of life compared to standard therapies? While conventional therapies have well-documented side effect profiles, the impact of experimental cancer treatment on quality of life can vary widely depending on the treatment type, disease stage, and patient factors. Some experimental treatments, particularly those involving immunotherapy or targeted approaches, may offer better tolerability and fewer systemic effects. However, others, especially those in early-stage testing, may introduce unexpected or severe toxicities. Quality of life assessments are increasingly being integrated into trial design, recognizing that survival alone is not the sole metric of success. In some cases, patients report a sense of empowerment and purpose by contributing to the future of cancer care through experimental treatment participation.
What are the psychological impacts of participating in an experimental treatment trial? The psychological landscape of clinical trial participation is complex, often marked by hope, anxiety, and uncertainty. Many patients pursue experimental treatment as a last resort, which can amplify emotional vulnerability. Yet, studies show that a structured trial environment and close monitoring can offer psychological benefits, such as increased support and attention from healthcare teams. Participants often express satisfaction in contributing to scientific advancement, even if personal clinical benefit is limited. However, the burden of decision-making, fear of side effects, and unclear outcomes can generate stress. Mental health support and transparent communication are essential components of ethical trial management.
How do researchers determine who qualifies for an experimental cancer treatment trial? Eligibility for participation in experimental cancer treatment trials is determined by strict inclusion and exclusion criteria designed to ensure patient safety and maximize the integrity of scientific results. These criteria can include cancer type and stage, previous treatment history, organ function metrics, and genetic or molecular biomarkers. While such selectivity can limit access, it is crucial for minimizing confounding variables and predicting treatment response. Increasingly, adaptive trial designs and precision medicine approaches are helping to broaden eligibility. The goal is to strike a balance between scientific rigor and equitable access to promising experimental treatment options.
What role does artificial intelligence play in advancing experimental cancer treatment? Artificial intelligence (AI) is becoming a transformative force in the design and delivery of experimental cancer treatment. AI algorithms can identify patterns in genomic data, predict drug response, and simulate clinical trial outcomes—dramatically accelerating the pace of discovery. Machine learning models also aid in patient stratification, allowing for more personalized and effective experimental treatment assignments. In radiology and pathology, AI enhances diagnostic accuracy, enabling earlier and more targeted interventions. These technologies also facilitate real-time monitoring of treatment efficacy and adverse events, creating a feedback loop that informs ongoing innovation. The integration of AI holds immense promise for improving both clinical outcomes and operational efficiency in experimental oncology.
Are there long-term health risks associated with receiving experimental treatment? Due to their investigational nature, the long-term health risks of experimental cancer treatments are often unknown at the time of administration. Some therapies may carry risks of late-onset toxicity, secondary malignancies, or immune dysregulation, particularly those involving genetic modification or immune system activation. Long-term follow-up is a standard component of most trial protocols and may continue for years after initial treatment. Patients are often enrolled in observational registries to track outcomes and adverse effects over time. While these risks must be weighed carefully, the potential benefits of experimental treatment for patients with limited options may justify these uncertainties, especially when supported by thorough informed consent and monitoring.
What financial considerations should patients be aware of when pursuing experimental treatment? Participation in experimental cancer treatment trials can entail various financial implications, though many study-related costs are typically covered by the sponsoring institution or pharmaceutical company. However, patients may still incur expenses related to travel, accommodation, and supportive care not included in the trial. Health insurance may or may not cover ancillary services associated with trial participation, depending on the policy and local regulations. Some nonprofit organizations offer grants or logistical support for patients seeking experimental treatment. Understanding the full spectrum of financial obligations is crucial, and patients are encouraged to consult financial counselors and clinical trial navigators before enrolling.
How are cultural and social factors influencing access to experimental cancer treatment? Access to experimental cancer treatment is shaped by a range of sociocultural dynamics, including race, ethnicity, language, geographic location, and socioeconomic status. Underserved populations are often underrepresented in clinical trials due to systemic barriers such as lack of transportation, limited health literacy, and mistrust of the medical system. Cultural beliefs may also influence willingness to participate in experimental treatment, particularly when communication is not tailored to the patient’s background. Efforts are underway to diversify trial recruitment and ensure inclusivity through community engagement, multilingual resources, and policy reform. Addressing these disparities is essential for ensuring that the benefits of innovation are equitably distributed.
What is the future outlook for experimental cancer treatment in mainstream medicine? The future of experimental cancer treatment is increasingly intertwined with the broader evolution of precision medicine, real-time analytics, and biologically adaptive care. As data sharing platforms, AI-driven tools, and decentralized trial models become more prevalent, the transition from experimental to standard practice will likely accelerate. Emerging fields such as synthetic biology, epitranscriptomics, and in situ vaccine development are poised to redefine the boundaries of cancer care. Moreover, regulatory innovations, such as adaptive licensing and conditional approvals, are streamlining the path from laboratory to clinic. In this rapidly changing landscape, experimental treatment is evolving from a niche option to a cornerstone of personalized oncology.

Conclusion: Embracing the Promise and Complexity of Experimental Cancer Treatment
The landscape of cancer care is undergoing a profound transformation, driven by relentless innovation and a deepening understanding of disease biology. Experimental cancer treatment occupies a pivotal role in this evolution, offering novel strategies for diagnosis, intervention, and long-term disease management. From immunotherapy to gene editing, nanotechnology to microbiome manipulation, each advance reflects the convergence of science, technology, and clinical insight. While challenges remain—from ethical concerns to logistical barriers—the overarching trajectory is one of promise and possibility. For patients facing limited options, these experimental treatments represent more than hope; they represent a tangible pathway to extended survival and improved quality of life. As research continues to unveil the intricate tapestry of cancer pathogenesis, the integration of experimental treatment into mainstream oncology will likely become not just a possibility, but a necessity. It is a future that demands both caution and courage, but above all, a steadfast commitment to science in service of humanity.
novel cancer therapies, breakthrough oncology research, cancer immunotherapy innovations, targeted cancer drugs, gene editing in oncology, CRISPR cancer research, precision oncology advances, nanotechnology in medicine, tumor microenvironment studies, cancer microbiome connection, clinical trial developments, personalized cancer medicine, future of oncology care, adaptive cancer therapies, AI in cancer diagnostics, emerging cancer treatments, immune system and cancer, oncology research pipeline, cancer therapy resistance, molecular oncology breakthroughs
Further Reading:
Experts Forecast Cancer Research and Treatment Advances in 2025
11 new research advances from the past year
Top Cancer Treatment Advances at MSK in 2024
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


