A New Era in Pancreatic Cancer Treatment
Pancreatic cancer has long held a grim reputation in oncology, standing as one of the most challenging and deadly forms of cancer. With a five-year survival rate lingering in the single digits for many patients, the urgency to develop more effective, targeted therapies has never been more pressing. Among the emerging solutions gaining traction is proton radiation therapy for pancreatic cancer, a form of advanced radiation that offers a more focused and precise approach than traditional methods. As technology evolves and clinical research deepens, this therapy is giving new hope to patients who previously had limited options.
You may also like: Cancer Research Breakthroughs: How Modern Advancements Are Transforming Treatment
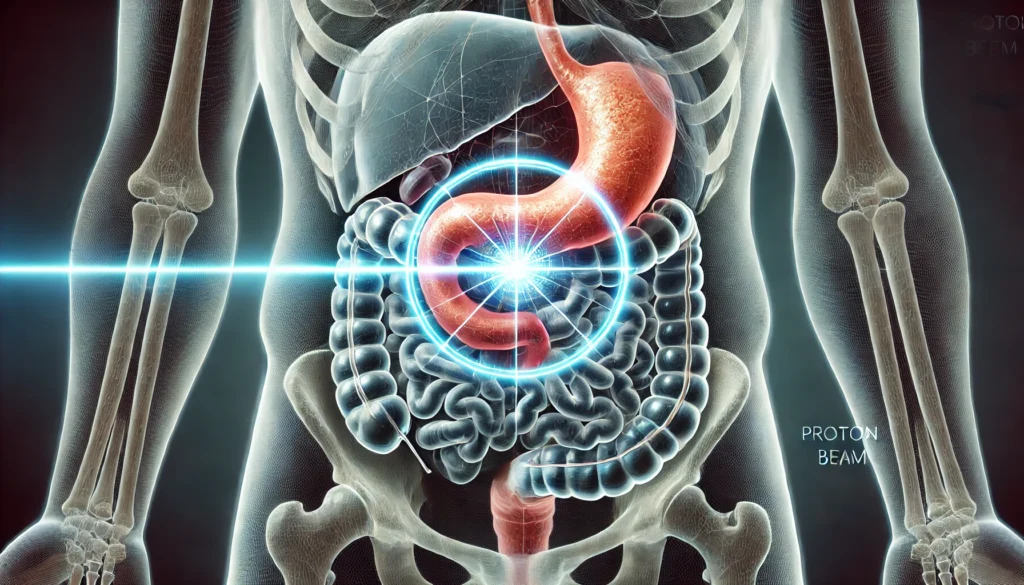
Proton therapy pancreatic cancer treatment differs from conventional photon-based radiation in the way it delivers energy to cancer cells. Instead of spreading energy along the entire path of the radiation beam, proton therapy concentrates the highest dose directly at the tumor site, minimizing exposure to surrounding healthy tissues. This property is particularly important in pancreatic cancer, where the tumor is often nestled among vital organs and blood vessels. For patients and physicians alike, the arrival of such precision technology marks a promising shift in the landscape of cancer care.
Understanding the Science Behind Proton Radiation
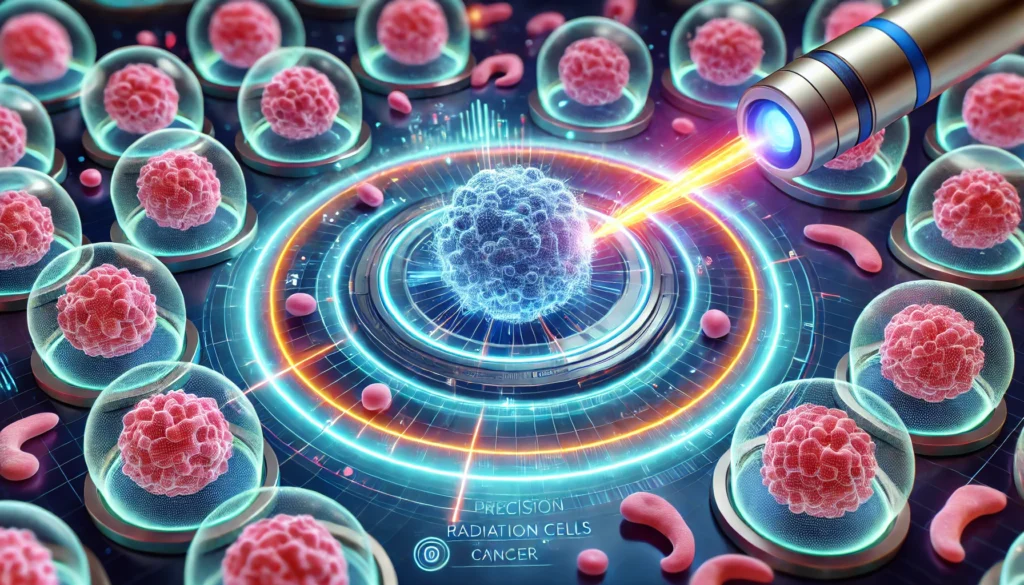
To grasp the full potential of proton therapy pancreatic cancer treatment, one must first understand the mechanics that distinguish it from traditional radiation. Conventional radiation uses X-rays (photons) that deposit energy as they pass through the body, affecting both healthy and cancerous tissues along the way. Proton therapy, on the other hand, utilizes positively charged particles—protons—which behave differently when interacting with matter. These particles deliver the bulk of their energy at a precise point known as the Bragg peak, beyond which the radiation dose drops sharply to zero.
Moreover, advances in imaging and planning software have enabled clinicians to map tumors in three dimensions with extraordinary accuracy. These tools support the delivery of proton radiation therapy for pancreatic cancer in ways that are adaptive and responsive to changes in tumor size or patient positioning. As a result, treatment can be optimized on an ongoing basis, offering both efficacy and flexibility.
The Clinical Advantages of Precision Radiation
Clinical trials and retrospective studies have increasingly demonstrated the tangible benefits of proton therapy for pancreatic cancer. Among the most significant findings is the reduction in gastrointestinal toxicity, a common and often debilitating side effect of abdominal radiation. Traditional therapies can inadvertently damage the small bowel, stomach, and colon, leading to complications such as nausea, vomiting, diarrhea, and in severe cases, bowel perforation or obstruction. By sparing these organs, proton therapy improves not just the tolerability of treatment but also the patient’s ability to complete the full course without interruptions.
Another important clinical advantage lies in the potential for dose escalation. Pancreatic tumors are notoriously radioresistant, meaning they often require higher doses of radiation to achieve meaningful control. However, delivering such doses has traditionally been constrained by the risk of damaging surrounding tissues. Proton therapy helps overcome this limitation, making it possible to administer stronger treatments with a lower risk profile.
Patient-Centered Outcomes and Quality of Life
While tumor control remains the central goal in oncology, modern cancer care increasingly emphasizes patient-centered outcomes such as functional status, symptom burden, and overall quality of life. Proton therapy pancreatic cancer treatment has been associated with favorable profiles in all these domains, especially when compared to photon-based approaches.
Importantly, quality-of-life benefits extend into the post-treatment period. Reduced radiation-induced damage to the gastrointestinal tract may decrease the risk of long-term complications such as strictures, ulceration, or chronic pain. This preservation of digestive function plays a crucial role in supporting recovery and nutritional health, especially for pancreatic cancer patients who often face digestive challenges related to tumor location or surgical resection.
Additionally, the psychological impact of receiving a more advanced, precise, and less damaging treatment cannot be underestimated. Patients frequently describe a sense of empowerment and optimism when offered cutting-edge technologies like proton beam therapy for pancreatic cancer. This mental resilience can influence not only the experience of care but also physiological outcomes such as immune function and treatment adherence.
Addressing Access, Availability, and Cost
Despite its growing reputation and clinical promise, proton radiation therapy for pancreatic cancer remains less accessible than traditional radiation modalities. This disparity stems from the high cost of building and operating proton therapy centers, which require sophisticated infrastructure, cyclotrons or synchrotrons, and substantial physical space. As of now, only a limited number of specialized centers in the United States and globally offer this technology.
Efforts are underway to address these challenges. Advances in compact proton therapy systems are making it more feasible to incorporate this technology into community cancer centers. At the same time, growing data on clinical effectiveness is helping to build the case for broader insurance coverage. Academic and advocacy groups are also playing a role by generating awareness, supporting policy change, and helping patients navigate the complexities of access.
Ultimately, achieving broader access to proton therapy pancreatic cancer treatment will require collaboration among stakeholders—clinicians, policymakers, payers, and patients. It will also demand continued investment in research, infrastructure, and patient education to ensure that this promising therapy can fulfill its potential in transforming pancreatic cancer care.
Ongoing Research and Future Directions
The story of proton beam therapy for pancreatic cancer is still unfolding, with new studies and clinical trials shedding light on its full capabilities. Several major academic centers are conducting randomized controlled trials comparing proton therapy to intensity-modulated radiation therapy (IMRT), with endpoints including local tumor control, toxicity profiles, quality of life, and overall survival. These studies aim to provide the high-level evidence needed to shift guidelines and influence payer policies.
Finally, survivorship research is beginning to focus on long-term outcomes, such as organ function, metabolic health, and psychosocial well-being. These studies are essential for understanding the full spectrum of benefits and risks associated with proton therapy and for guiding follow-up care in patients who achieve remission.
The Promise and Responsibility of Innovation in Cancer Care
As with any advanced medical technology, the introduction of proton therapy into pancreatic cancer treatment brings with it both great promise and significant responsibility. While the potential benefits are considerable—ranging from reduced toxicity to enhanced tumor control—these must be weighed against practical concerns such as cost, availability, and equitable access. Innovation must not only push the boundaries of what is medically possible but also remain grounded in the real-world experiences of patients navigating a complex healthcare system.
One of the central ethical considerations is ensuring that the promise of proton radiation therapy for pancreatic cancer does not exacerbate existing disparities in care. Socioeconomic status, geographic location, and insurance coverage should not determine who can access potentially life-extending treatments. Institutions must therefore commit to transparency, advocacy, and patient-centered decision-making that aligns advanced therapies with the needs and values of diverse populations.
Furthermore, patients themselves must be empowered as active participants in their care. Through clear communication, shared decision-making, and access to trustworthy information, individuals can make informed choices about whether proton therapy aligns with their treatment priorities. This empowerment is especially important in the context of pancreatic cancer, where decisions often carry profound implications for quality of life and survival.
Frequently Asked Questions: Proton Therapy Pancreatic Cancer Treatment
1. How does proton therapy support recovery after pancreatic cancer surgery?
Proton therapy plays a valuable role in enhancing post-surgical recovery for pancreatic cancer patients. Because proton radiation therapy for pancreatic cancer minimizes radiation exposure to adjacent organs, patients are less likely to experience complications that could hinder healing. This is particularly important when surgery involves procedures like the Whipple, where preserving nearby tissues is crucial. With fewer side effects, patients can return to eating and digesting sooner, which supports immune strength and overall recovery. Moreover, the gentler impact of proton therapy allows clinicians to coordinate post-operative chemotherapy with less delay, potentially improving long-term outcomes.
2. Can proton therapy be used alongside clinical trials for pancreatic cancer?
Absolutely. Many cutting-edge clinical trials now incorporate proton therapy pancreatic cancer treatment as part of innovative research protocols. These trials often explore combinations with immunotherapies or targeted drugs, offering participants access to investigational regimens not available through standard care. Proton beam therapy for pancreatic cancer is increasingly recognized for its compatibility with these advanced approaches due to its precision and reduced toxicity. Patients enrolled in such studies may benefit from both the therapeutic effects of proton therapy and the potential advantages of novel systemic agents. As clinical trials become more personalized, proton therapy often complements the strategic delivery of treatment.
3. How does insurance coverage vary for proton therapy in pancreatic cancer care?
Insurance approval for proton therapy pancreatic cancer treatment can vary widely depending on the provider and geographic region. While more insurers are beginning to recognize the clinical value of proton beam therapy for pancreatic cancer, many still consider it investigational for this indication. Patients often need strong supporting documentation from their care teams, including data on anticipated toxicities and comparisons with photon-based therapy. Some centers employ dedicated insurance specialists to help patients navigate preauthorization processes and appeals. Fortunately, as more outcomes data accumulate, coverage is expanding—especially for cases where conventional radiation poses heightened risks.
4. Are there differences in recovery experiences between proton and conventional radiation?
Yes, the recovery experience can be significantly more favorable with proton radiation therapy for pancreatic cancer. Conventional radiation often leads to fatigue, appetite loss, and digestive issues that persist for weeks after treatment. In contrast, proton therapy’s tissue-sparing precision reduces the inflammatory burden on the gastrointestinal tract and surrounding organs. As a result, many patients report faster return to normal activities, fewer dietary restrictions, and less reliance on supportive medications. While individual experiences vary, the overall trajectory of recovery is often smoother and more manageable with proton therapy.
5. How do patients emotionally respond to receiving proton beam therapy?
Psychological responses to proton therapy pancreatic cancer treatment are overwhelmingly positive, especially when patients understand the rationale behind the precision approach. Many report a sense of empowerment from receiving a technologically advanced therapy that aligns with their values of preserving function and minimizing harm. In a disease as emotionally taxing as pancreatic cancer, this psychological boost can translate into greater resilience and treatment adherence. Patients also appreciate the more tolerable side effect profile, which helps them stay engaged with daily life and maintain important relationships. The visible investment in innovation at proton centers further reassures patients that they are receiving cutting-edge care.
6. What are some lesser-known side effects specific to proton therapy for pancreatic cancer?
While proton beam therapy for pancreatic cancer is generally well-tolerated, there are nuanced side effects that merit attention. For instance, subtle shifts in gastrointestinal motility may occur due to low-dose exposure to peripheral organs, potentially leading to temporary bloating or irregular bowel patterns. Additionally, if proton therapy is administered near spinal structures, patients may experience transient nerve-related sensations. Rarely, proton therapy may trigger local skin irritation or fatigue localized to the treated region. Importantly, these effects are typically mild and self-limiting when compared to the broader toxicity associated with conventional modalities. Tailored symptom management strategies can help patients maintain comfort and quality of life throughout treatment.
7. How are treatment plans personalized with proton therapy for pancreatic cancer?
Proton radiation therapy for pancreatic cancer is uniquely suited to highly individualized treatment planning. Advanced imaging, including PET-MRI fusion scans, allows clinicians to delineate tumors with exceptional accuracy and adapt to changes in real time. Treatment plans can be modified mid-course to account for weight fluctuations, anatomical shifts, or tumor shrinkage. Additionally, motion management techniques such as respiratory gating help ensure that the radiation dose remains tightly focused even as patients breathe. These personalized adjustments maximize tumor control while minimizing toxicity, making proton therapy an ideal candidate for precision-based medicine. Such dynamic planning is less feasible with conventional radiation platforms.
8. Can older patients safely undergo proton therapy for pancreatic cancer?
Yes, older adults often tolerate proton therapy pancreatic cancer treatment very well, particularly when compared to standard radiation approaches. Age alone is not a limiting factor; rather, overall fitness and comorbidities guide treatment decisions. Because proton therapy causes fewer systemic side effects, elderly patients are less likely to suffer from dehydration, weight loss, or medication interactions during radiation. This is especially important for those with pre-existing digestive or renal issues that could be aggravated by conventional treatment. Proton therapy’s safety profile allows older patients to maintain independence and continue concurrent treatments when necessary.
9. How does the physical setup of proton therapy differ from standard radiation centers?
The physical environment of a proton therapy center is distinctly high-tech, often featuring large gantries, cyclotrons, and custom-designed treatment rooms. The patient experience typically includes specialized immobilization devices to maintain consistent positioning throughout sessions. While the sessions themselves are not necessarily longer, the setup time may be slightly extended due to the need for meticulous alignment. Many centers also integrate visual or audio aids to help patients remain calm and still during treatment. This enhanced infrastructure reflects the precision of proton beam therapy for pancreatic cancer and contributes to its superior accuracy.
10. What innovations are on the horizon for proton therapy in pancreatic cancer treatment?
Several innovations are poised to expand the utility of proton radiation therapy for pancreatic cancer. One promising area is FLASH proton therapy, which delivers ultra-high dose rates in milliseconds, potentially reducing side effects even further. Researchers are also exploring radiomics and machine learning to refine dose predictions and improve patient selection. Furthermore, integration with wearable devices and real-time biomarker monitoring could soon allow for adaptive responses to biological changes during treatment. As the cost of proton therapy decreases with compact system development, more regional centers may begin to offer this option. These advancements suggest that proton therapy pancreatic cancer treatment will continue to evolve in both scope and precision.
Proton Therapy and Pancreatic Cancer: A Future Worth Fighting For
The journey of proton beam therapy for pancreatic cancer is emblematic of the broader evolution of cancer treatment—from blunt-force approaches to precision-targeted strategies that prioritize both effectiveness and quality of life. While challenges remain in terms of access, cost, and definitive evidence, the clinical and patient-reported benefits emerging from proton therapy are undeniable. This technology is not a panacea, but it represents a meaningful advance for one of the most difficult-to-treat malignancies in modern medicine.
As research progresses and technology becomes more accessible, the potential to change outcomes for pancreatic cancer patients grows ever stronger. Proton radiation therapy for pancreatic cancer is more than just a technological innovation; it is a testament to the power of human ingenuity, scientific perseverance, and the enduring hope that better treatments are always on the horizon. In a field often marked by sobering statistics and limited options, this precision radiation therapy offers a rare but tangible promise: a future in which even the hardest tumors can be met with strength, accuracy, and renewed possibility.
advanced radiation therapy, gastrointestinal cancer treatment, pancreatic tumor radiation, high-precision oncology, non-invasive cancer therapy, cutting-edge cancer treatment, radiation therapy side effects, pancreatic cancer survival strategies, radiation oncology innovations, cancer care personalization, pancreas-focused radiation, soft tissue sparing radiation, emerging cancer treatments, immunotherapy and radiation synergy, multidisciplinary cancer care, cancer treatment planning, clinical trials in oncology, adaptive radiation therapy, geriatric oncology care, quality of life in cancer treatment
Further Reading:
Proton Therapy in the Management of Pancreatic Cancer
Proton Therapy: The Future Of Precision Cancer Treatment
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.