Introduction
The pulmonary artery plays a crucial role in the human circulatory system, serving as the primary conduit for deoxygenated blood from the heart to the lungs. As one of the most vital arteries in the body, any dysfunction or disorder affecting the pulmonary artery can have profound implications for overall cardiovascular health. Despite its importance, many people are unaware of the specific functions of the pulmonary artery, the common conditions that may affect it, and the potential treatment options available. Understanding the anatomy, physiology, and pathology of the pulmonary artery is essential for medical professionals and patients alike, as it allows for early detection and appropriate intervention in various pulmonary and cardiovascular disorders.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
In this article, we will explore the pulmonary artery’s fundamental role in circulation, discuss common disorders that can compromise its function, and highlight the latest advancements in medical research and treatment options. Additionally, we will emphasize the importance of maintaining pulmonary artery health through lifestyle modifications, early diagnosis, and medical management. By integrating the latest scientific findings and expert opinions, this article aims to provide a comprehensive overview of pulmonary artery health while maintaining readability and practical application for a broad audience.

The Role of the Pulmonary Artery in Circulation
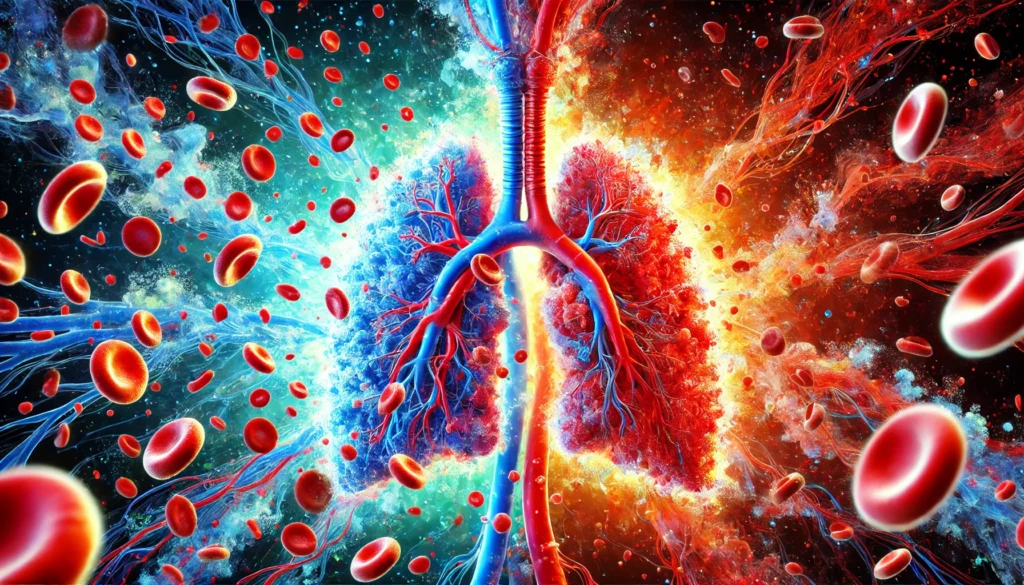
The pulmonary artery is a key component of the pulmonary circulation system, which is responsible for transporting deoxygenated blood from the right ventricle of the heart to the lungs. Unlike other arteries in the body that carry oxygen-rich blood, the pulmonary artery is unique in that it carries oxygen-depleted blood to the lungs for gas exchange. This distinction highlights the pulmonary artery’s fundamental role in sustaining life by ensuring that blood is properly oxygenated before it is pumped to the rest of the body.
The pulmonary artery originates from the right ventricle of the heart and quickly bifurcates into the left and right pulmonary arteries, which supply blood to each lung. Once in the lungs, the pulmonary arteries further branch into smaller arterioles and capillaries, facilitating the exchange of carbon dioxide and oxygen within the alveoli. This process is critical for maintaining proper blood gas levels, which influence cellular respiration, metabolic function, and overall systemic health.
Without the efficient function of the pulmonary artery, the body would be unable to receive the oxygen it needs to sustain vital processes. Any obstruction, narrowing, or damage to the pulmonary artery can result in severe cardiovascular complications, including pulmonary hypertension and right-sided heart failure. Given its essential role in circulation, maintaining pulmonary artery health is of paramount importance in preventing potentially life-threatening conditions.
Common Disorders Affecting the Pulmonary Artery
Numerous conditions can affect the pulmonary artery, each presenting unique challenges in diagnosis and treatment. Understanding these disorders allows for better management and preventive care, ultimately reducing morbidity and mortality associated with pulmonary vascular diseases.
Pulmonary Hypertension
Pulmonary hypertension (PH) is a condition characterized by elevated blood pressure within the pulmonary arteries. It occurs when the blood vessels in the lungs become narrowed, stiffened, or blocked, increasing resistance to blood flow. This increased pressure forces the right side of the heart to work harder to pump blood into the lungs, which can lead to right ventricular hypertrophy and, eventually, heart failure.
There are several types of pulmonary hypertension, including pulmonary arterial hypertension (PAH), which is a specific form of the disease that affects the pulmonary arteries directly. PAH can be idiopathic (without a known cause) or secondary to other conditions such as connective tissue diseases, congenital heart defects, or chronic lung diseases. Symptoms of pulmonary hypertension include shortness of breath, chest pain, fatigue, and fainting, particularly during physical exertion. Early detection and treatment with medications such as vasodilators, endothelin receptor antagonists, and anticoagulants can help manage the disease and improve quality of life.
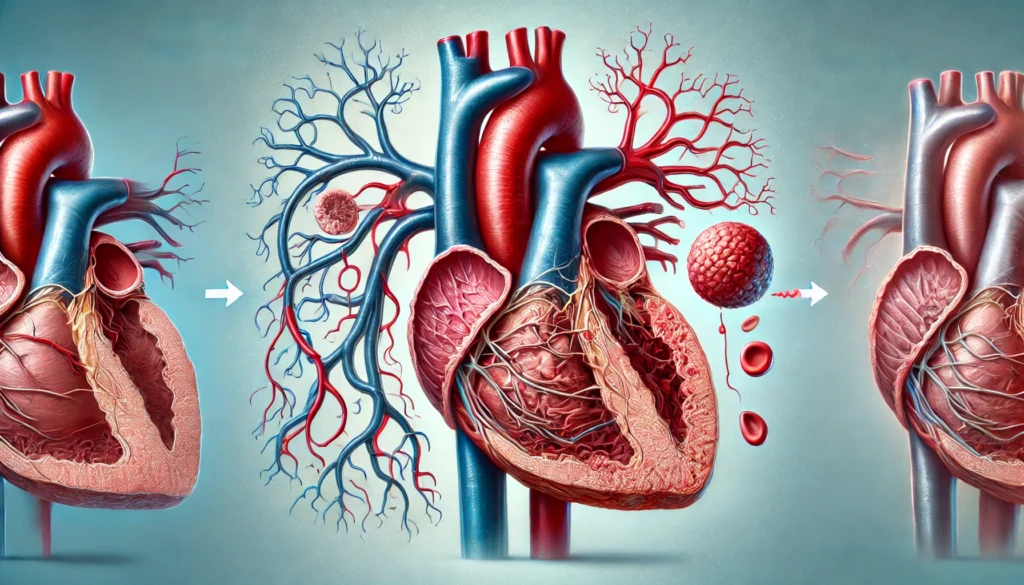
Pulmonary Embolism
A pulmonary embolism (PE) occurs when a blood clot, typically originating from the deep veins of the legs (deep vein thrombosis or DVT), travels to the lungs and obstructs a pulmonary artery. This blockage can impede blood flow to the lungs, leading to decreased oxygen levels in the blood and potential life-threatening complications.
Symptoms of a pulmonary embolism include sudden shortness of breath, sharp chest pain, rapid heart rate, and coughing up blood. Risk factors for PE include prolonged immobility, surgery, pregnancy, and conditions that increase blood clotting, such as cancer or thrombophilia. Immediate medical intervention is necessary to prevent severe complications, and treatment often involves anticoagulant therapy, thrombolytic agents, or surgical interventions such as thrombectomy or placement of a vena cava filter.
Pulmonary Artery Stenosis
Pulmonary artery stenosis is a condition in which the pulmonary artery becomes narrowed, restricting blood flow from the heart to the lungs. This condition can be congenital or acquired due to inflammatory diseases, infections, or surgical complications.
In congenital cases, pulmonary artery stenosis is often associated with congenital heart defects, such as Tetralogy of Fallot or Williams syndrome. Symptoms may vary depending on the severity of the narrowing but often include difficulty breathing, cyanosis (bluish discoloration of the skin), and fatigue. Treatment options range from balloon angioplasty and stent placement to surgical reconstruction in severe cases.
Maintaining Pulmonary Artery Health
Maintaining the health of the pulmonary artery is crucial for overall cardiovascular well-being. Several strategies can help reduce the risk of developing pulmonary artery disorders, including lifestyle modifications, regular medical check-ups, and appropriate medical interventions.
A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can help prevent conditions such as high blood pressure and atherosclerosis, which can indirectly impact the pulmonary artery. Regular physical activity promotes cardiovascular fitness and improves lung function, reducing the risk of pulmonary hypertension and other related conditions. Additionally, avoiding smoking and exposure to environmental pollutants can protect the pulmonary artery from damage caused by inflammation and oxidative stress.
For individuals with predisposing risk factors, regular monitoring of blood pressure, cholesterol levels, and lung function can aid in early detection and management of potential issues. Medications such as anticoagulants and vasodilators can be used in individuals diagnosed with pulmonary vascular diseases to prevent complications and improve outcomes. Furthermore, advances in medical research continue to provide innovative treatment options, including targeted therapies and surgical interventions for severe pulmonary artery disorders.
Frequently Asked Questions (FAQ) About Pulmonary Artery Health
1. What makes the pulmonary artery unique compared to other arteries?
The pulmonary artery is unique because, unlike most arteries that carry oxygen-rich blood, it transports oxygen-depleted blood from the heart to the lungs for oxygenation. This distinction plays a crucial role in maintaining the body’s oxygen balance. The artery in the lung branches into smaller vessels that facilitate efficient gas exchange in the alveoli, ensuring that blood is reoxygenated before circulating to the rest of the body. The pulmonary artery also has lower pressure compared to systemic arteries, allowing for more efficient blood flow through the lungs. Any dysfunction in this artery can significantly impact oxygen delivery and overall cardiovascular health.
2. How does pulmonary hypertension affect the artery in the lung?
Pulmonary hypertension causes increased pressure within the pulmonary artery, making it harder for blood to travel from the heart to the lungs. Over time, this condition can lead to thickening and stiffening of the arterial walls, reducing their ability to expand and accommodate normal blood flow. As a result, the right side of the heart has to work harder, which may eventually lead to right ventricular failure. The effects of pulmonary hypertension can lead to significant symptoms such as shortness of breath, dizziness, and fatigue. Early diagnosis and targeted treatments can help slow the progression of the disease and preserve pulmonary artery function.
3. Can lifestyle choices impact pulmonary artery health?
Yes, lifestyle choices play a significant role in maintaining pulmonary artery health. Smoking, for example, can lead to chronic inflammation and increased pressure in the pulmonary artery, raising the risk of pulmonary hypertension and other vascular diseases. Regular physical activity improves overall cardiovascular fitness and can help keep the pulmonary artery functioning efficiently. A diet rich in antioxidants and heart-healthy fats can reduce oxidative stress and inflammation, which may contribute to arterial stiffness. Additionally, managing stress and ensuring adequate sleep are essential for preventing vascular dysfunction. Taking proactive steps in daily life can significantly reduce the risk of developing pulmonary artery-related conditions.
4. What are the potential complications of a blocked pulmonary artery?
A blocked pulmonary artery, often caused by a pulmonary embolism, can lead to severe complications, including sudden respiratory distress and decreased oxygen supply to vital organs. If left untreated, a large embolism can cause pulmonary infarction, where part of the lung tissue dies due to a lack of blood flow. Severe cases can lead to life-threatening conditions such as right-sided heart failure or sudden cardiac arrest. Treatment typically involves anticoagulants to prevent further clot formation, but in critical cases, clot-dissolving medications or surgical interventions may be required. Recognizing symptoms such as sharp chest pain, rapid breathing, and lightheadedness can be lifesaving in the early stages of a pulmonary embolism.
5. How do congenital conditions affect the pulmonary artery?
Congenital heart defects, such as Tetralogy of Fallot or pulmonary artery stenosis, can significantly alter the structure and function of the pulmonary artery. Some congenital abnormalities result in narrowed or malformed arteries that restrict blood flow to the lungs, leading to reduced oxygenation of blood. These conditions often require early medical intervention, including surgical procedures or catheter-based treatments to restore normal circulation. In some cases, lifelong monitoring and medication are necessary to manage associated complications. Advances in pediatric cardiology have significantly improved outcomes for individuals born with pulmonary artery defects, allowing them to lead active and healthy lives.
6. Can pulmonary artery conditions be detected early?
Early detection of pulmonary artery conditions is possible through various diagnostic tests, including echocardiography, CT angiography, and right heart catheterization. These imaging techniques help assess blood flow, artery structure, and potential blockages that could indicate underlying issues. Symptoms such as unexplained shortness of breath, persistent fatigue, or chest discomfort should prompt further medical evaluation. Blood tests measuring biomarkers related to heart strain can also provide early indications of pulmonary artery dysfunction. Regular check-ups, particularly for individuals with risk factors like smoking or a family history of cardiovascular disease, can aid in early diagnosis and timely intervention.
7. How does chronic lung disease impact the pulmonary artery?
Chronic lung diseases such as chronic obstructive pulmonary disease (COPD) or pulmonary fibrosis can place excessive strain on the pulmonary artery. When lung function declines, the arteries in the lung must work harder to facilitate oxygen exchange, often leading to increased pulmonary blood pressure. This added strain can contribute to pulmonary hypertension, further complicating respiratory conditions. Oxygen therapy and pulmonary rehabilitation programs can help alleviate pressure on the pulmonary artery by improving oxygenation and reducing overall vascular stress. Addressing lung diseases early can prevent secondary complications involving the pulmonary artery and improve long-term health outcomes.
8. Are there surgical treatments available for pulmonary artery disorders?
Yes, several surgical treatments are available for managing severe pulmonary artery disorders. Pulmonary thromboendarterectomy (PTE) is a procedure used to remove chronic blood clots obstructing the pulmonary artery, restoring normal blood flow. For cases of severe pulmonary hypertension, lung transplantation may be considered when other treatments fail. Congenital defects affecting the pulmonary artery often require corrective surgery to ensure adequate blood circulation from the heart to the lungs. Minimally invasive procedures, such as balloon angioplasty or stent placement, are also available to address narrowed arteries and improve blood flow. Surgical interventions are typically reserved for severe cases where medical therapies alone are insufficient.
9. What role do medications play in maintaining pulmonary artery health?
Medications play a critical role in managing pulmonary artery disorders by improving blood flow, reducing inflammation, and preventing clot formation. Vasodilators help widen the pulmonary artery, reducing resistance and allowing blood to flow more freely. Anticoagulants and antiplatelet drugs are commonly prescribed to prevent or treat clots that could lead to pulmonary embolism. In cases of pulmonary hypertension, endothelin receptor antagonists and phosphodiesterase inhibitors can help regulate vascular pressure. Proper medication management, often in combination with lifestyle changes and oxygen therapy, significantly improves the quality of life for individuals with pulmonary artery diseases.
10. What advancements are being made in pulmonary artery research?
Medical research on pulmonary artery health continues to advance, with new treatment strategies emerging to improve patient outcomes. Gene therapy is being explored as a potential approach to correcting genetic mutations that contribute to pulmonary hypertension. Scientists are also investigating the use of stem cells to repair damaged blood vessels and restore pulmonary artery function. Novel drug therapies targeting specific pathways involved in vascular remodeling are showing promise in clinical trials. Additionally, wearable technology and artificial intelligence are being integrated into patient monitoring, allowing for early detection of pulmonary artery-related complications. These advancements hold great promise for the future of pulmonary medicine, offering hope for improved treatments and potential cures for pulmonary artery diseases.
Conclusion
The pulmonary artery plays an indispensable role in the circulatory system, ensuring that oxygen-depleted blood is efficiently transported to the lungs for gas exchange. Disorders affecting the pulmonary artery, such as pulmonary hypertension, pulmonary embolism, and pulmonary artery stenosis, can have significant health implications if left untreated. Understanding these conditions, their causes, symptoms, and treatment options is essential for both medical professionals and individuals at risk.
By adopting a proactive approach to cardiovascular health through lifestyle modifications, regular medical check-ups, and adherence to prescribed treatments, individuals can significantly reduce their risk of developing pulmonary artery-related conditions. As medical research continues to evolve, new treatment modalities and preventive strategies offer hope for improved outcomes and enhanced quality of life for those affected by pulmonary artery disorders. With greater awareness and education, pulmonary artery health can be prioritized, ultimately leading to better overall cardiovascular and pulmonary function.
cardiovascular health, lung circulation, pulmonary vascular disease, heart and lung connection, respiratory circulation, arterial blood flow, pulmonary hypertension treatment, blood clot in lungs, chronic lung disease effects, vascular function, cardiopulmonary system, oxygen transport in blood, right heart failure, pulmonary embolism risk, lung disease and heart health, circulation disorders, vascular health tips, arterial pressure regulation, heart-lung interaction, pulmonary disease management
Further Reading:
Pathophysiology and new advances in pulmonary hypertension
Evaluation and management of pulmonary arterial hypertension
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


