Red spots on neck can be unsettling, particularly when they appear suddenly or without a clear cause. For many individuals, these spots may be accompanied by itching, burning, swelling, or even emotional distress due to their visibility. Though they can stem from a variety of causes, ranging from harmless to more concerning medical conditions, understanding the underlying reasons for these spots is crucial. Whether the red spots are flat or raised, itchy or painless, isolated or widespread, deciphering their nature requires an informed approach. This guide delves deep into potential causes, relevant symptoms, and treatment options, and highlights when it becomes necessary to consult a medical professional.
You may also like: Breakthrough Approaches to Eczema Alternative Healing: What Works and Why It Matters
Understanding the Nature of Skin Inflammation and Irritations
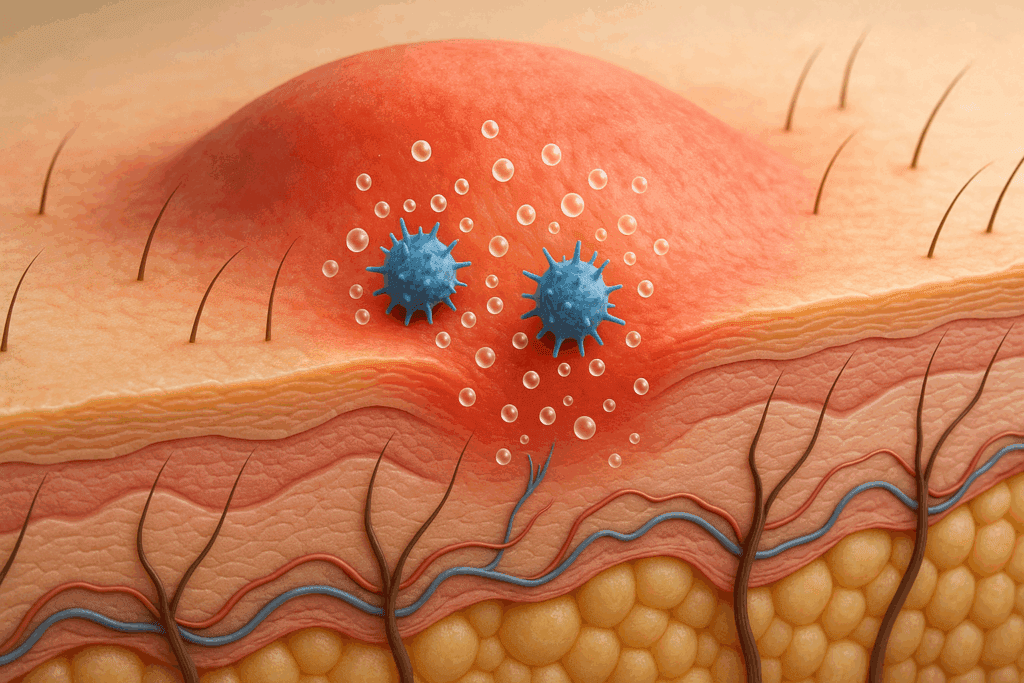
At the heart of many skin eruptions, including red spots on the neck, lies the biological process of skin inflammation. Inflammation serves as the body’s natural defense against irritants, infections, and injuries. When the immune system identifies a threat, it sends inflammatory cells to the affected site, leading to swelling, redness, heat, and sometimes pain. While this process protects the body, it can also manifest as various dermatological symptoms, such as red dots on skin, red splotches on face, or even flat red spots on skin.
One common trigger of such inflammation is contact with allergens or irritants. Substances like certain metals in jewelry, fragrances in lotions, or even laundry detergents can provoke contact dermatitis on neck and other exposed areas. This form of dermatitis often appears as a rash with red spots that itch and may form small red bumps on skin. It is important to recognize these symptoms early and identify potential culprits to prevent recurring episodes.
In other cases, skin inflammation may be a reaction to internal changes, such as hormonal shifts, autoimmune responses, or systemic infections. For instance, viral infections like rubella or bacterial infections like strep throat can produce red spots or rashes that extend to the neck and torso. These systemic responses are often accompanied by fever, fatigue, or other signs of illness, requiring prompt medical attention.

Why Do I Have Red Dots on My Skin and Neck?
When patients ask, “Why do I have red dots on my skin?”, the answer is not always straightforward. The skin is the body’s largest organ and serves as a visible indicator of internal health. Red dots may signal a benign issue like heat rash or a more significant problem such as vasculitis or petechiae, small red spots that do not blanch when pressed and may indicate blood vessel abnormalities or clotting issues.
In the context of the neck, red dots often develop due to friction, sweat retention, or allergic reactions. Clothing materials, perfumes, or exposure to heat can all contribute to outbreaks. Even minor irritation from shaving or jewelry can result in visible red spots. Additionally, stress-induced hives can manifest as small red dots on skin that are itchy and migratory.
Another common but overlooked cause is seborrheic dermatitis, which typically affects areas with oil-producing glands, such as the scalp, behind the ears, and the neck. This condition results in red dry patches on skin that may flake or peel. Though not contagious, seborrheic dermatitis can persist without proper treatment and often requires medicated shampoos or creams.

Red Spots on Neck from Dermatitis and Allergic Reactions
One of the primary dermatological conditions linked to red spots on the neck is dermatitis, an umbrella term encompassing several types of skin inflammation. Allergic contact dermatitis, for example, arises when the immune system reacts to a substance it deems harmful, even if it’s not inherently dangerous. Common allergens include nickel, latex, preservatives, and plant oils.
This type of dermatitis typically results in red bumps on face or neck and can progress to oozing blisters if scratched or left untreated. A closely related form is irritant contact dermatitis, which occurs when the skin is repeatedly exposed to a harsh substance, such as soap, detergent, or chlorine. Unlike allergic dermatitis, irritant dermatitis does not require prior sensitization, and anyone can develop it after enough exposure.
Atopic dermatitis (eczema) is another condition that may cause random red spots on skin, particularly in individuals with a family history of allergies or asthma. In children and adults alike, atopic dermatitis may affect the folds of the neck, arms, and knees. Chronic scratching leads to thickened, leathery skin and may predispose individuals to bacterial infections. Recognizing these patterns and seeking early dermatological intervention can prevent flare-ups and minimize long-term skin damage.
Exploring the Connection Between Hives, Dry Skin, and Red Spots
It is not uncommon to wonder whether you can get hives from dry skin, especially during colder months when moisture levels drop significantly. The answer is nuanced. While dry skin itself doesn’t cause hives, it compromises the skin barrier and makes it more susceptible to allergens and irritants. This vulnerability can lead to the formation of red bumps that itch on legs, arms, or the neck.
Hives, or urticaria, are welts that appear suddenly and can disappear within hours or linger for days. They result from the release of histamine in the skin, which increases blood vessel permeability and leads to fluid leakage into surrounding tissues. Triggers for hives vary widely and include foods, medications, stress, temperature changes, and physical stimuli like pressure or vibration.
Individuals with a history of eczema or allergic rhinitis are more prone to hives, especially when their skin is already dry or irritated. Applying fragrance-free moisturizers and avoiding known allergens can significantly reduce the frequency and intensity of outbreaks. However, if hives become chronic or interfere with daily life, antihistamines or prescription medications may be required.

Can Contact Dermatitis Spread and Worsen Without Treatment?
A frequent concern among those experiencing itchy rashes is whether contact dermatitis can spread. The short answer is that allergic contact dermatitis does not spread from person to person, but it can expand on the same individual if exposure to the allergen continues. Irritant contact dermatitis can also worsen and involve larger areas of skin, particularly when the barrier function is repeatedly compromised.
For instance, someone using a new lotion on their neck might develop red spots on neck after repeated applications. If the offending product isn’t discontinued, these spots may evolve into more extensive areas of inflammation, even spreading to nearby regions such as the shoulders or chest. Persistent scratching can also create new breaks in the skin, inviting secondary bacterial infections.
Moreover, chronic contact dermatitis may trigger a phenomenon known as autoeczematization, where a localized rash leads to widespread eczema-like symptoms throughout the body. This highlights the importance of early diagnosis and the avoidance of irritants or allergens. Patch testing by a dermatologist can help identify specific triggers, allowing patients to make informed choices about skincare and hygiene products.
The Role of Environmental and Occupational Factors in Red Spot Formation
Beyond direct skin contact with irritants, environmental and occupational exposures play a significant role in the development of skin rashes, especially red spots on arms, neck, and face. Individuals working in construction, healthcare, agriculture, or the food industry often handle substances that can irritate or sensitize the skin. Prolonged exposure to gloves, solvents, or disinfectants can lead to dermatitis on hands and neck.
Similarly, climates with high humidity or frequent temperature fluctuations can create conditions that foster skin inflammation. Sweat accumulation and friction in these environments can cause pink spots on skin or a red dot rash, especially in skin folds or under clothing. These factors highlight the need for protective gear, appropriate skin care routines, and environmental controls in workplaces to reduce dermatological complaints.
Interestingly, even indoor environments can contribute to skin issues. For example, prolonged exposure to indoor heating during winter can dry the skin and exacerbate red dry patches. Airborne allergens like dust mites, mold spores, and pet dander can also lead to skin inflammation and trigger existing conditions such as atopic dermatitis.

Recognizing Red Spots on Neck as Part of Systemic Conditions
While many causes of red spots are localized and benign, it is essential to remain vigilant for signs that these skin changes might be part of a broader systemic condition. Autoimmune diseases, such as lupus or dermatomyositis, may present with distinctive rashes that affect the face and neck. In lupus, the classic malar rash or “butterfly rash” often precedes more serious systemic symptoms, such as joint pain or kidney involvement.
Another condition to consider is vasculitis, which involves inflammation of blood vessels and may cause red dots on skin that are palpable and sometimes painful. These dots may not blanch under pressure and are frequently accompanied by symptoms such as fever, fatigue, or muscle pain. Petechiae and purpura are also concerning findings that suggest a need for further evaluation, particularly in patients taking anticoagulants or with platelet disorders.
Infections such as mononucleosis, measles, or scarlet fever can also manifest with red spots on neck and torso. These cases often include systemic signs like sore throat, swollen glands, or high fever. Medical evaluation is crucial in these instances, as timely diagnosis can prevent complications and ensure appropriate treatment.
The Relationship Between Skin Location and Symptom Patterns
When evaluating red spots, the location of the rash provides important diagnostic clues. For example, dermatitis on thighs might suggest chafing, friction, or sensitivity to certain fabrics. Red bumps that itch on leg above knee could point toward folliculitis, insect bites, or even a heat rash. Skin rash on elbows and knees may be indicative of psoriasis, a chronic autoimmune condition characterized by well-demarcated plaques with silvery scales.
Similarly, red splotches on face often raise concerns due to their visibility and potential for lasting discoloration. These could stem from rosacea, lupus, or even allergic reactions to facial products. On the neck, the presence of red dry patches or tiny red spots on skin could reflect a broad spectrum of issues, from fungal infections to systemic allergies.
Patterns of distribution and associated symptoms such as itching, burning, scaling, or systemic illness can guide clinicians toward a more accurate diagnosis. Detailed history-taking, including recent exposures, new products, medications, and travel, further helps narrow the differential.
What Causes Red Spots on Skin? A Broad Differential Diagnosis
The question “what causes red spots on skin” can only be answered by considering a broad range of possibilities. These include infectious agents (bacterial, viral, fungal), allergic reactions, inflammatory conditions, autoimmune diseases, vascular abnormalities, and even malignancies. Each category encompasses multiple diagnoses with varying degrees of severity.
For instance, a red dot rash from a viral exanthem may resolve on its own, whereas purpura associated with thrombocytopenia might indicate a serious hematologic disorder. Likewise, small red dots on skin itchy from bedbug bites may be treated with topical steroids and antihistamines, but petechiae from leukemia require urgent oncologic evaluation.
The process of elimination begins with a careful examination of lesion characteristics—color, shape, size, texture, distribution, and evolution over time. Supporting tests like skin biopsies, blood panels, and allergy testing can offer definitive answers when clinical diagnosis remains uncertain.
Red Spots on Neck: When to Seek Medical Advice
While many instances of red spots on neck are self-limited and respond well to over-the-counter treatments, certain signs warrant professional evaluation. These include persistent or worsening symptoms, involvement of mucous membranes, signs of infection (such as pus or fever), and systemic symptoms like joint pain or fatigue.
Additionally, if red spots recur frequently or spread despite home treatment, a visit to a dermatologist is advisable. Conditions like psoriasis, eczema, and lupus require long-term management strategies, including lifestyle modifications and prescription therapies. Early intervention can improve outcomes and reduce the risk of complications such as scarring or secondary infections.
Another scenario to consider is medication-induced rashes, especially when starting a new drug. Drug eruptions can range from mild red dots to severe reactions like Stevens-Johnson Syndrome, which requires emergency care. Documenting new medications and promptly reporting any skin changes to a healthcare provider is essential.
Effective Prevention and Skincare Strategies
Prevention remains a cornerstone of managing red spots, especially for individuals with sensitive or reactive skin. Simple measures like choosing fragrance-free, hypoallergenic skincare products, wearing loose-fitting clothing, and avoiding known triggers can go a long way in minimizing flare-ups. Regular moisturizing helps restore the skin barrier and prevent conditions like dermatitis on face or red dry patches on skin.
Sun protection is also crucial. UV exposure not only exacerbates existing rashes but can also trigger new lesions in conditions like lupus or photosensitive eczema. Broad-spectrum sunscreens with SPF 30 or higher, along with protective clothing, can significantly reduce UV-induced skin damage.
For those prone to contact dermatitis, patch testing can provide definitive answers about specific allergens to avoid. Educating oneself about ingredients in skincare and cleaning products, coupled with environmental control measures like air purifiers, can further enhance skin resilience.
Understanding Small Red Spots on Skin: Clues and Clinical Insights
Small red spots on skin, particularly when itchy or clustered, often signify an allergic, infectious, or inflammatory process. In some cases, such as in cherry angiomas or petechiae, they are painless and may not itch. Identifying the context in which they appear—such as after exercise, sun exposure, or dietary changes—can yield valuable diagnostic clues.
In children, conditions like viral exanthems, scarlet fever, or fifth disease can present with widespread small red dots on skin. Adults may develop similar presentations due to shingles, allergic drug reactions, or stress-related hives. Skin examination under good lighting, sometimes aided by dermatoscopy, helps differentiate benign from concerning lesions.
Ultimately, integrating clinical findings with patient history and, when needed, laboratory tests ensures that these spots are evaluated correctly and treated appropriately. Ignoring persistent or unexplained skin changes can delay the diagnosis of underlying conditions that might require more than just topical care.
Frequently Asked Questions: Understanding Red Spots on Neck and Related Skin Conditions
What are some unexpected environmental factors that can trigger red spots on neck?
Beyond the typical irritants such as perfumes or metal jewelry, environmental factors like rapid shifts in temperature, low indoor humidity, and air pollution can significantly contribute to skin inflammation. Urban dwellers often face high levels of particulate matter that can settle on the skin and cause red spots on neck, especially when the skin barrier is compromised. Additionally, chlorinated water from pools or even hard tap water can act as irritants over time, especially in individuals prone to dermatitis on neck. Seasonal allergies can also affect the skin indirectly—airborne pollen doesn’t just cause sneezing; it can land on the skin and lead to contact dermatitis or random red spots on skin. Those living in dry or polluted areas might benefit from using humidifiers, air purifiers, and gentle cleansers to reduce skin stress.
Can emotional stress directly cause or worsen red spots on skin?
Absolutely. Emotional stress has a direct link to skin health due to its impact on the immune and endocrine systems. When you’re under stress, your body increases cortisol production, which can suppress immune function and impair the skin’s natural barrier. This makes the skin more vulnerable to conditions like hives, red bumps on face, or red dry patches on skin. Stress also exacerbates existing skin inflammation, making flare-ups of dermatitis on face, neck, and thighs more frequent and severe. Practicing relaxation techniques such as meditation, yoga, or biofeedback may not only help mental health but also minimize outbreaks of small red dots on skin itchy from psychosomatic triggers.
Is it possible for red bumps that itch on leg above knee to be related to systemic conditions?
Yes, while many red bumps that itch on leg above knee may appear due to local issues like shaving irritation or insect bites, they can sometimes indicate systemic conditions. For example, autoimmune diseases such as lupus or dermatomyositis can cause skin manifestations across various parts of the body, not just isolated areas. Similarly, vasculitis may start with small red spots on skin but progress into widespread rashes that affect multiple limbs. If these bumps persist or are accompanied by fatigue, joint pain, or fever, it’s crucial to look beyond dermatologic causes. Medical providers may order blood tests, biopsies, or imaging to assess for underlying disease when the skin rash on elbows and knees or thighs appears suspiciously widespread or recurrent.
What differentiates a red dot rash from petechiae or purpura?
A red dot rash generally refers to flat red spots on skin that may or may not itch and often accompany allergic reactions, viral infections, or irritants. In contrast, petechiae are pinpoint red dots on body caused by minor bleeding under the skin and do not blanch under pressure. Purpura is similar but larger and often signals issues with clotting or platelet disorders. Unlike red splotches on face due to rosacea or dermatitis, petechiae and purpura are not inflammatory in origin and may indicate a serious systemic condition. If red spots appear suddenly without any identifiable trigger and are accompanied by bruising or systemic symptoms, immediate medical evaluation is warranted.
Can you get hives from dry skin, or is that a myth?
While dry skin doesn’t directly cause hives, it significantly increases your susceptibility to them. A compromised skin barrier allows allergens and irritants to penetrate more easily, triggering immune responses like hives. In winter months, individuals often experience red spots on arms or tiny red spots on skin due to a combination of dryness and environmental allergens. Moisturizing frequently with ceramide-rich lotions can help restore the skin’s barrier and prevent hives. If your skin is chronically dry and you frequently develop red spots on skin, especially when under stress or exposed to irritants, maintaining optimal hydration levels both internally and externally becomes critical.
How does dermatitis on thighs differ from other types of dermatitis?
Dermatitis on thighs is often influenced by factors like friction, sweating, and fabric irritation. Unlike dermatitis on face or neck, which may be linked more to cosmetics or environmental triggers, thigh dermatitis is frequently mechanical or fungal in nature. People who wear tight clothing or exercise frequently are at higher risk of developing small red bumps on skin in this area. It’s also worth noting that obesity can increase the risk of intertrigo, a type of skin inflammation found in skin folds, which may manifest as red dry patches on skin. Preventative strategies include wearing breathable fabrics, using anti-chafing powders, and keeping the area clean and dry.
What should I do if I keep noticing recurring pink spots on skin?
Recurring pink spots on skin may be indicative of chronic allergic reactions, rosacea, or even early signs of autoimmune conditions. Unlike temporary red dots on skin caused by heat or friction, pink spots often fade and return, suggesting a deeper underlying issue. It’s important to track triggers—such as specific foods, environmental changes, or skincare products—to identify patterns. In some cases, these spots may progress into red bumps or evolve into small red dots on skin that persist or spread. A dermatologist may perform patch testing or recommend a biopsy if the etiology remains unclear after initial assessment.
Can contact dermatitis spread even after removing the irritant?
Contact dermatitis typically improves once the offending agent is removed, but in certain situations, it may appear to spread. This can happen if the skin becomes hypersensitive and starts reacting to other, previously tolerated substances—a process called secondary sensitization. Additionally, scratching the initial rash can transfer allergens to adjacent skin areas, giving the impression that the dermatitis is spreading. For example, an allergic reaction to a necklace might initially cause red spots on neck but extend to red spots on arms if the allergen is transferred via touch. To prevent this, avoid scratching, wash the area thoroughly, and apply topical corticosteroids as directed.
Why do I have red dots on my skin even though I’ve made no lifestyle changes?
Sometimes, red dots on skin emerge without any obvious change in routine, but this doesn’t mean no change has occurred. Immune responses can be delayed, and something as subtle as a new detergent, seasonal pollen shift, or mild dietary adjustment may provoke skin inflammation. Additionally, internal factors such as hormonal fluctuations, minor infections, or vitamin deficiencies can lead to red spots or even small red dots on skin itchy in nature. It’s also possible for tiny red spots on skin to appear from pressure or trauma, especially in individuals on anticoagulants. Keeping a health journal can help track less apparent influences over time and uncover hidden patterns.
Are red spots on neck ever a sign of something contagious?
Yes, in certain cases, red spots on neck may result from contagious conditions like viral exanthems, fungal infections, or bacterial skin conditions. For example, impetigo can cause red bumps on face or neck that become crusty and are highly transmissible, particularly among children. Fungal infections like tinea corporis (ringworm) may start as red dry patches on skin and spread to areas like the neck or arms. While not all rashes are contagious, the presence of weeping lesions, fever, or close contact with an infected individual raises the likelihood. If red spots appear alongside flu-like symptoms or spread rapidly in a household or school setting, it is best to consult a healthcare provider promptly.
Reflecting on Red Spots, Skin Health, and the Importance of Medical Insight
Red spots on the neck are more than just a cosmetic concern; they serve as visible markers of the body’s intricate immune and dermatological processes. From benign causes like friction and dry skin to more serious concerns such as autoimmune diseases or vascular disorders, the potential explanations are diverse and multifaceted. Recognizing whether red dots on skin are harmless or indicative of a deeper issue requires a combination of observation, knowledge, and when necessary, professional assessment.
Equally important is understanding how related conditions such as dermatitis on thighs, rash on elbows and knees, or red splotches on face may interconnect to form a comprehensive picture of skin health. Knowing when to ask, “Can contact dermatitis spread?” or “Why do I have red dots on my skin?” empowers individuals to advocate for their well-being with informed urgency.
Investing in proactive skincare, avoiding known irritants, and seeking early medical evaluation for persistent or unexplained symptoms can significantly improve outcomes. As with any aspect of health, awareness, prevention, and expert guidance are vital tools in navigating the complexities of dermatological care. Whether managing small red bumps on skin or evaluating systemic symptoms, timely and evidence-based action leads to better skin and overall health outcomes.


