Understanding Stable Angina and Coronary Artery Disease
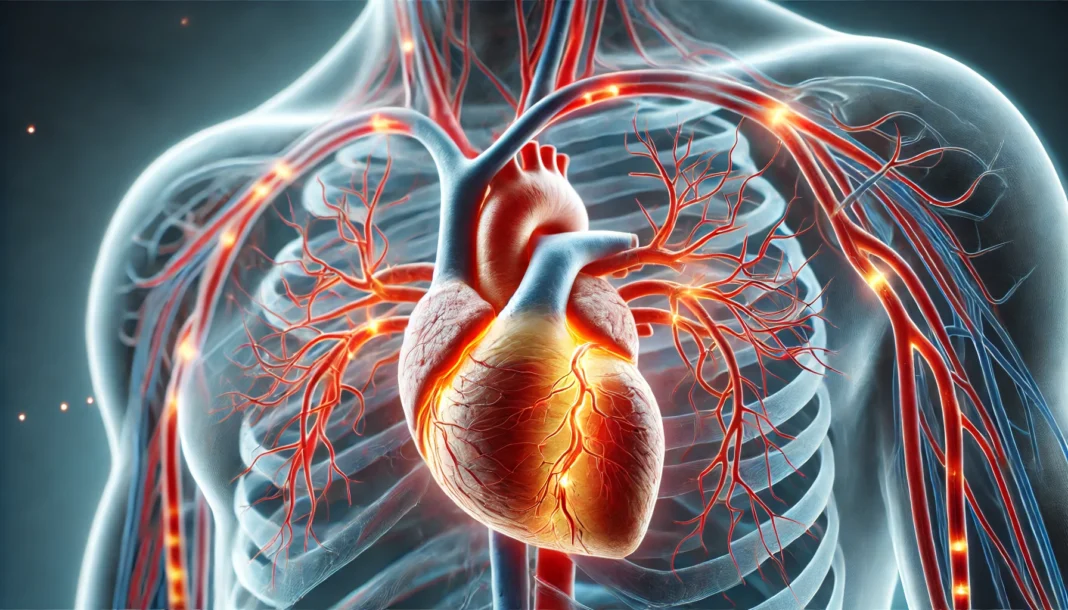
Stable angina and coronary artery disease (CAD) are interconnected cardiovascular conditions that impact millions of individuals worldwide. These conditions often develop silently over time, progressively restricting blood flow to the heart and increasing the risk of severe cardiac events. Understanding the causes, symptoms, and treatment options for stable angina and CAD is essential for individuals at risk, as well as for healthcare professionals aiming to provide optimal care.
You may also like: How to Naturally Reverse 20 Years of Arterial Plaque: Science-Backed Strategies for a Healthier Heart
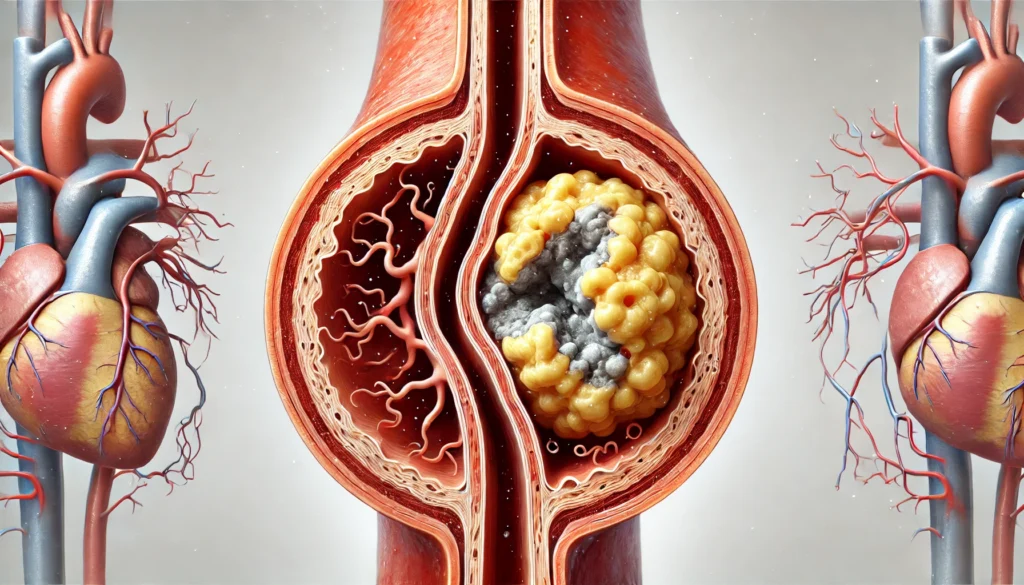
Stable angina is a type of chest pain that occurs due to reduced blood flow to the heart, typically triggered by physical exertion or emotional stress. Unlike unstable angina, which can occur unpredictably and may signal an impending heart attack, stable angina follows a more consistent pattern and is often relieved with rest or medication. Coronary artery disease, the primary underlying cause of stable angina, results from the buildup of atherosclerotic plaques within the coronary arteries, leading to narrowing and reduced oxygen supply to the myocardium. The interplay between these conditions necessitates a comprehensive approach to management, involving lifestyle modifications, pharmacological interventions, and, in some cases, surgical procedures.
Causes of Stable Angina and Coronary Artery Disease
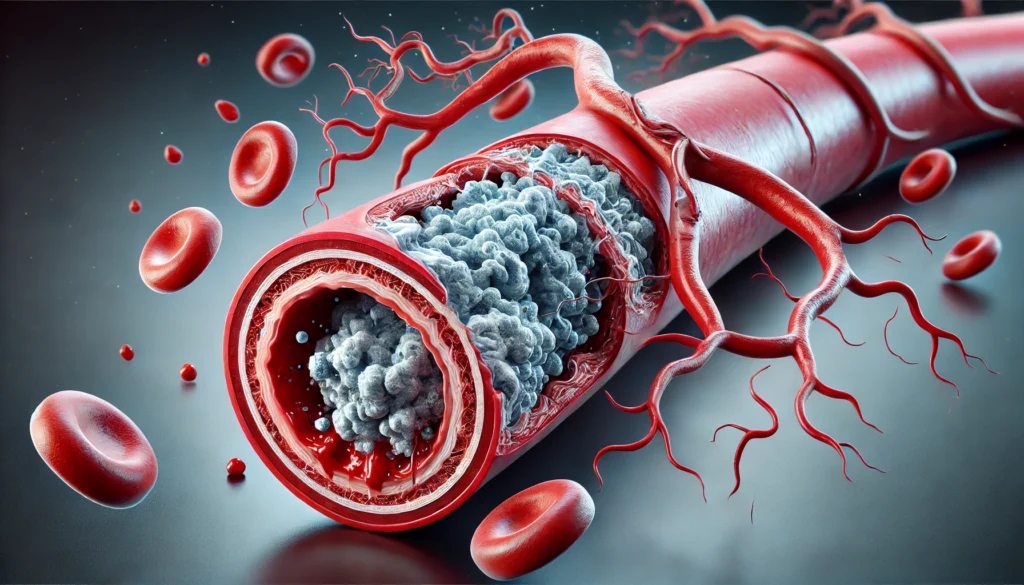
The development of stable angina and CAD is primarily attributed to atherosclerosis, a progressive disease characterized by the accumulation of fatty deposits, cholesterol, and other substances within the arterial walls. This process leads to the formation of plaques that narrow the arteries and restrict blood flow. Several risk factors contribute to the onset and progression of atherosclerosis, each playing a significant role in the pathophysiology of CAD.
Hypertension, or high blood pressure, exerts excessive force on the arterial walls, accelerating the damage that facilitates plaque formation. Elevated cholesterol levels, particularly low-density lipoprotein (LDL) cholesterol, contribute to the buildup of fatty deposits, while high levels of high-density lipoprotein (HDL) cholesterol help protect against arterial narrowing. Diabetes mellitus further exacerbates the risk by promoting inflammation and vascular damage, increasing the likelihood of plaque rupture and thrombosis.
Lifestyle factors also play a crucial role in the development of CAD and stable angina. A diet high in saturated fats, trans fats, and processed foods can accelerate atherosclerosis, while physical inactivity contributes to obesity and metabolic syndrome, both of which heighten cardiovascular risk. Smoking introduces harmful chemicals that damage the endothelium and promote arterial stiffness, while excessive alcohol consumption can lead to hypertension and cardiomyopathy. Genetic predisposition also influences susceptibility to CAD, with a family history of heart disease serving as a significant risk factor.
Recognizing Symptoms of Stable Angina
Stable angina presents with a characteristic pattern of symptoms, most notably chest pain or discomfort that occurs predictably with exertion and subsides with rest. This pain is often described as a pressure, tightness, or burning sensation in the chest, sometimes radiating to the arms, neck, jaw, or back. The duration of discomfort typically lasts a few minutes and is relieved by ceasing physical activity or taking nitroglycerin.
Beyond chest pain, individuals with stable angina may experience additional symptoms, including shortness of breath, fatigue, nausea, and dizziness. These symptoms arise due to the heart’s inability to receive adequate oxygen during periods of increased demand. While stable angina does not indicate an immediate heart attack, it signifies underlying CAD that requires careful monitoring and management.
Distinguishing stable angina from other forms of chest pain is crucial for accurate diagnosis. Conditions such as gastroesophageal reflux disease (GERD), musculoskeletal pain, and anxiety-related chest discomfort can mimic angina, leading to diagnostic challenges. However, the predictable nature of stable angina, along with its relief upon resting, provides key clinical clues.

Diagnosing Stable Angina and Coronary Artery Disease
Diagnosing stable angina and CAD involves a combination of clinical evaluation, laboratory tests, and imaging studies. A detailed medical history and physical examination help identify risk factors and symptom patterns. Physicians assess the frequency, duration, and triggers of chest pain, as well as associated symptoms that may suggest myocardial ischemia.
Electrocardiography (ECG) is a fundamental diagnostic tool that records the heart’s electrical activity and detects ischemic changes. However, a resting ECG may appear normal in individuals with stable angina, necessitating further testing. Stress testing, which involves exercising on a treadmill or stationary bicycle while monitoring heart function, can reveal ischemic abnormalities under exertion.
Coronary angiography, often performed using cardiac catheterization, provides a definitive assessment of coronary artery blockages. This procedure involves injecting contrast dye into the coronary arteries and capturing X-ray images to visualize the extent of atherosclerosis. Additionally, non-invasive imaging techniques such as coronary computed tomography angiography (CTA) and magnetic resonance imaging (MRI) offer valuable insights into arterial health and myocardial perfusion.
Treatment Options for Stable Angina and Coronary Artery Disease
Effective management of stable angina and CAD requires a multifaceted approach aimed at alleviating symptoms, preventing disease progression, and reducing the risk of heart attacks. Treatment strategies encompass lifestyle modifications, pharmacological therapies, and interventional procedures.
Lifestyle Modifications: Adopting heart-healthy lifestyle changes is a cornerstone of CAD management. Dietary interventions, including the Mediterranean diet, emphasize fruits, vegetables, whole grains, and healthy fats while limiting processed foods and refined sugars. Regular physical activity, such as brisk walking or cycling, enhances cardiovascular fitness and helps maintain a healthy weight. Smoking cessation is imperative, as tobacco use accelerates atherosclerosis and increases the likelihood of cardiovascular events.
Pharmacological Therapies: Medications play a crucial role in stabilizing angina and managing CAD. Nitrates, such as nitroglycerin, provide rapid symptom relief by dilating coronary arteries and improving blood flow. Beta-blockers reduce heart rate and oxygen demand, while calcium channel blockers enhance arterial dilation and decrease myocardial workload. Antiplatelet agents, including aspirin, prevent clot formation, and statins lower cholesterol levels to slow atherosclerosis progression.
Interventional Procedures: For individuals with severe arterial blockages, revascularization procedures may be necessary. Percutaneous coronary intervention (PCI), commonly known as angioplasty, involves inserting a catheter with a balloon to widen narrowed arteries. Stent placement helps maintain arterial patency and prevent restenosis. Coronary artery bypass grafting (CABG) is reserved for extensive CAD cases, where bypassing blocked arteries with grafts restores blood flow to the heart.
Frequently Asked Questions (FAQ) About Stable Angina and Coronary Artery Disease
What lifestyle changes can help manage stable angina effectively?
Managing stable angina effectively requires a combination of heart-healthy habits tailored to improve cardiovascular function. One of the most impactful changes is adopting a diet rich in fruits, vegetables, whole grains, and lean proteins while reducing saturated fats, trans fats, and processed foods that contribute to atherosclerosis. Regular physical activity, such as brisk walking, swimming, or cycling, enhances circulation and helps maintain optimal heart function. Stress management techniques, including mindfulness meditation, deep breathing exercises, and adequate sleep, can prevent angina episodes triggered by emotional strain. Additionally, avoiding tobacco products and limiting alcohol intake can significantly lower the risk of progression from stable angina to more severe cardiac conditions.
Can stable angina turn into a heart attack?
Although stable angina itself is not a heart attack, it signals underlying coronary artery disease and angina-related concerns that may increase the risk of a future cardiac event. Over time, if the coronary arteries continue to narrow due to plaque buildup, the restricted blood flow can result in unstable angina or myocardial infarction. Warning signs that stable angina may be worsening include an increase in frequency, intensity, or duration of chest discomfort, as well as symptoms occurring at rest. It is crucial for individuals with stable angina to undergo regular medical evaluations to assess their heart health and adjust treatment plans accordingly. By closely monitoring symptoms and adhering to prescribed therapies, patients can mitigate the likelihood of their condition progressing into a life-threatening emergency.
How does stress contribute to coronary artery disease and angina?
Chronic stress has a profound impact on cardiovascular health, often exacerbating conditions such as coronary artery disease and angina. When an individual experiences stress, the body releases adrenaline and cortisol, which can temporarily elevate heart rate and blood pressure. Over time, prolonged exposure to these stress hormones promotes inflammation and endothelial dysfunction, accelerating the progression of atherosclerosis. Furthermore, stress often leads to unhealthy coping mechanisms, such as overeating, smoking, or a sedentary lifestyle, all of which contribute to worsening cardiovascular health. Implementing relaxation techniques, engaging in regular physical activity, and seeking psychological support can help reduce stress-related cardiac risks.
Are there early warning signs of coronary artery disease before angina develops?
Many individuals with coronary artery disease experience subtle warning signs before angina becomes noticeable. Symptoms such as unusual fatigue, shortness of breath, dizziness, and discomfort in the jaw, neck, or back can indicate reduced blood flow to the heart. Some people may also experience indigestion-like sensations, particularly after exertion or heavy meals. These early signs should not be dismissed, especially for those with risk factors such as hypertension, diabetes, or a family history of cardiovascular disease. Detecting coronary artery disease early through medical screenings and lifestyle modifications can help prevent the onset of angina and more severe complications.
How do medications for stable angina work?
Medications for stable angina function by improving blood flow to the heart and reducing the heart’s workload. Nitrates, such as nitroglycerin, rapidly relax and widen blood vessels, easing the strain on the heart and alleviating chest discomfort. Beta-blockers slow the heart rate and lower blood pressure, decreasing oxygen demand during physical activity or stress. Calcium channel blockers prevent arterial constriction, enhancing blood supply to the myocardium while reducing chest pain episodes. Antiplatelet drugs like aspirin help prevent blood clots from forming, reducing the risk of heart attacks in individuals with coronary artery disease and angina. Cholesterol-lowering medications, particularly statins, help manage atherosclerosis progression by reducing plaque buildup within the arteries.
Can alternative therapies help in managing stable angina?
While conventional treatments remain the primary approach to managing stable angina, alternative therapies can complement medical interventions. Acupuncture has been studied for its potential in reducing angina-related discomfort by promoting circulation and alleviating muscle tension. Herbal supplements such as hawthorn extract have been explored for their cardiovascular benefits, though they should be used cautiously under medical supervision. Yoga and Tai Chi can improve heart rate variability, lower stress, and enhance overall cardiovascular fitness, providing holistic support alongside traditional therapies. However, it is essential for patients to consult their healthcare providers before incorporating alternative treatments to ensure they do not interfere with prescribed medications or existing health conditions.
What role does sleep quality play in coronary artery disease and angina?
Sleep quality has a direct impact on heart health, particularly for individuals with coronary artery disease and angina. Poor sleep, especially in those with sleep apnea, contributes to increased blood pressure, inflammation, and reduced oxygen levels, all of which aggravate cardiovascular strain. Studies have shown that people who consistently get less than six hours of sleep per night have a higher risk of developing heart disease. Additionally, disrupted sleep patterns can lead to hormonal imbalances that affect cholesterol levels, insulin resistance, and arterial health. Prioritizing good sleep hygiene, maintaining a regular sleep schedule, and seeking treatment for sleep disorders can significantly reduce angina episodes and improve overall cardiac function.
How does climate and seasonal change affect stable angina?
Weather fluctuations, particularly extreme cold or heat, can impact individuals with stable angina. Cold temperatures cause blood vessels to constrict, increasing blood pressure and making it harder for the heart to pump efficiently, potentially triggering angina episodes. Conversely, extreme heat can lead to dehydration, lowering blood pressure and causing an imbalance in electrolyte levels, which may result in heart strain. Seasonal changes can also influence physical activity levels, with colder months leading to reduced outdoor exercise and higher risks of weight gain. To mitigate these effects, individuals with coronary artery disease and angina should dress appropriately for the weather, stay hydrated, and modify physical activities to suit environmental conditions.
Can coronary artery disease and angina be reversed?
While coronary artery disease is a chronic condition, its progression can often be slowed or even partially reversed through aggressive lifestyle interventions. A heart-healthy diet low in saturated fats and high in fiber can help reduce arterial plaque buildup. Regular aerobic exercise improves endothelial function and promotes the development of collateral blood vessels, which can enhance circulation in the heart. Comprehensive lifestyle programs, such as the Ornish or Mediterranean diet, have demonstrated potential in reducing arterial narrowing and improving cardiovascular outcomes. Additionally, medical advancements, including new cholesterol-lowering therapies and regenerative medicine approaches, offer promising avenues for managing and potentially reversing certain aspects of coronary artery disease and angina.
What advancements in medical research are shaping the future of angina treatment?
Medical research is continuously evolving to improve the treatment of stable angina and coronary artery disease. Emerging therapies include gene-based treatments aimed at enhancing vascular repair and reducing atherosclerosis. Novel cholesterol-lowering medications, such as PCSK9 inhibitors, provide an alternative for individuals who do not respond to traditional statins. Developments in bioengineered tissues and stem cell therapy are being explored as potential solutions for regenerating damaged heart muscle. Personalized medicine, utilizing genetic profiling, is also gaining traction to optimize treatment plans based on an individual’s unique cardiovascular risk factors. These innovations, along with advances in minimally invasive cardiac procedures, hold great promise for improving the long-term outcomes of individuals with stable angina and CAD.
Conclusion: Enhancing Heart Health and Preventing Complications
Stable angina and coronary artery disease represent significant cardiovascular challenges that require proactive management. By understanding the causes, symptoms, and treatment options, individuals can take informed steps toward reducing their risk and improving heart health. Lifestyle modifications, combined with medical therapies and, when necessary, interventional procedures, form the foundation of effective disease management.
Early detection and regular monitoring are essential in preventing complications such as heart attacks and heart failure. Patients should work closely with healthcare providers to optimize their treatment plans and make sustainable lifestyle changes. As research continues to advance, novel therapeutic approaches, including personalized medicine and regenerative therapies, hold promise for improving outcomes in individuals with stable angina and CAD. Through awareness, prevention, and adherence to medical recommendations, individuals can achieve better cardiovascular health and enhance their overall quality of life.
heart disease prevention, cardiac health tips, myocardial ischemia management, symptoms of chest pain, blood circulation improvement, cardiovascular risk factors, managing high cholesterol, hypertension and heart disease, lifestyle changes for heart health, heart attack prevention strategies, plaque buildup in arteries, best diet for heart patients, exercise for heart health, reducing heart disease risk, stress management for heart patients, cardiac rehabilitation programs, chronic angina relief, improving vascular health, heart-friendly medications, early signs of heart disease
Further Reading:
Stable Angina Pectoris: 1. Clinical Patterns
Angina: contemporary diagnosis and management
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.