Living with digestive discomfort is a reality for millions of people worldwide, but not all reflux is created equal. While occasional heartburn may seem like a minor inconvenience, chronic and advanced forms of gastroesophageal reflux disease (GERD) can result in serious, long-term complications. One of the most severe manifestations of GERD is stage 4 acid reflux, a condition marked by substantial esophageal damage, often accompanied by complications such as strictures, Barrett’s esophagus, or even early signs of esophageal cancer. Recognizing the seriousness of this stage is crucial, as it not only affects digestive health but can also influence systemic well-being and quality of life. This article explores the critical facts surrounding stage 4 acid reflux, its causes, symptoms, and potential treatment options, offering insights that can help patients and healthcare providers navigate this challenging condition more effectively.
You may also like: How Long Does GERD Last in Adults? Expert Insights on This Common Yet Persistent Digestive Condition
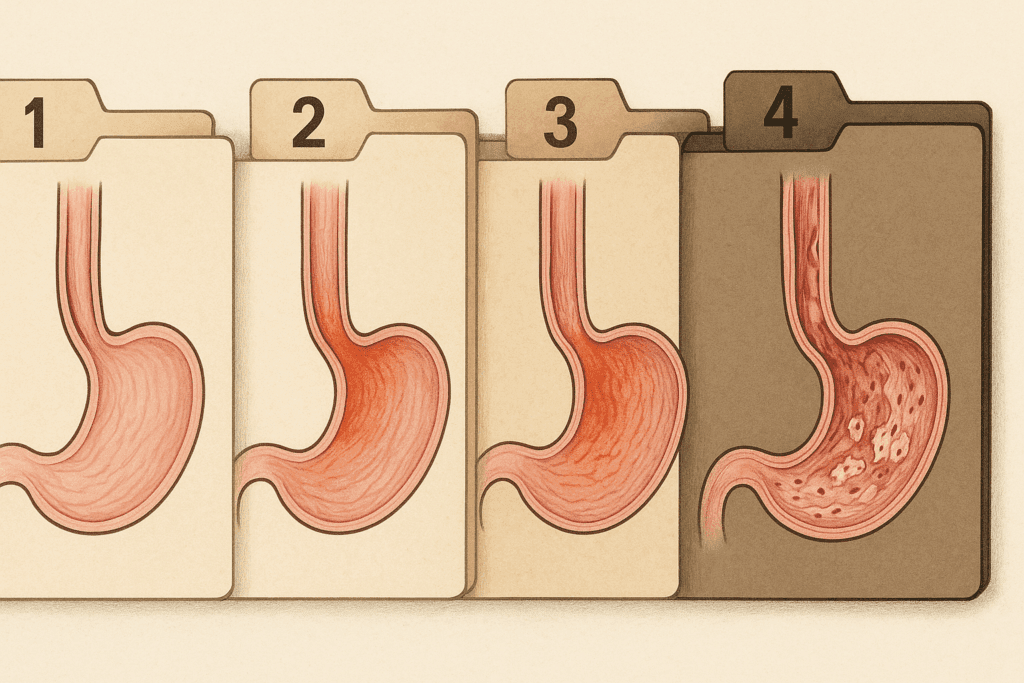
Understanding the Progression: The Four Stages of Acid Reflux
Acid reflux is not a monolithic condition; it exists on a spectrum, progressing through identifiable stages. The stages of acid reflux begin with mild and intermittent symptoms that many people experience occasionally, often triggered by dietary habits or lifestyle factors. In this earliest phase, symptoms such as heartburn or regurgitation occur infrequently and usually resolve without medication. However, without intervention or lifestyle adjustments, these episodes can become more frequent, leading to stage 2, where the condition becomes more chronic and may require medical management with over-the-counter antacids or H2 blockers.
Stage 3 marks a more concerning progression, where inflammation and damage to the esophageal lining become more pronounced. Individuals may experience persistent symptoms despite lifestyle changes and medication. This stage is also when endoscopic evaluations might reveal esophagitis, erosions, or other structural changes in the esophagus. Finally, stage 4 acid reflux represents the most severe end of the spectrum. At this point, the esophagus may show signs of narrowing, scarring, or cellular changes consistent with Barrett’s esophagus—a known risk factor for esophageal cancer. The shift through these stages is not always linear, and some individuals may accelerate through them more rapidly due to genetic predisposition, comorbid conditions, or untreated symptoms. Understanding the stages of GERD is essential for timely diagnosis and effective intervention before irreversible damage occurs.
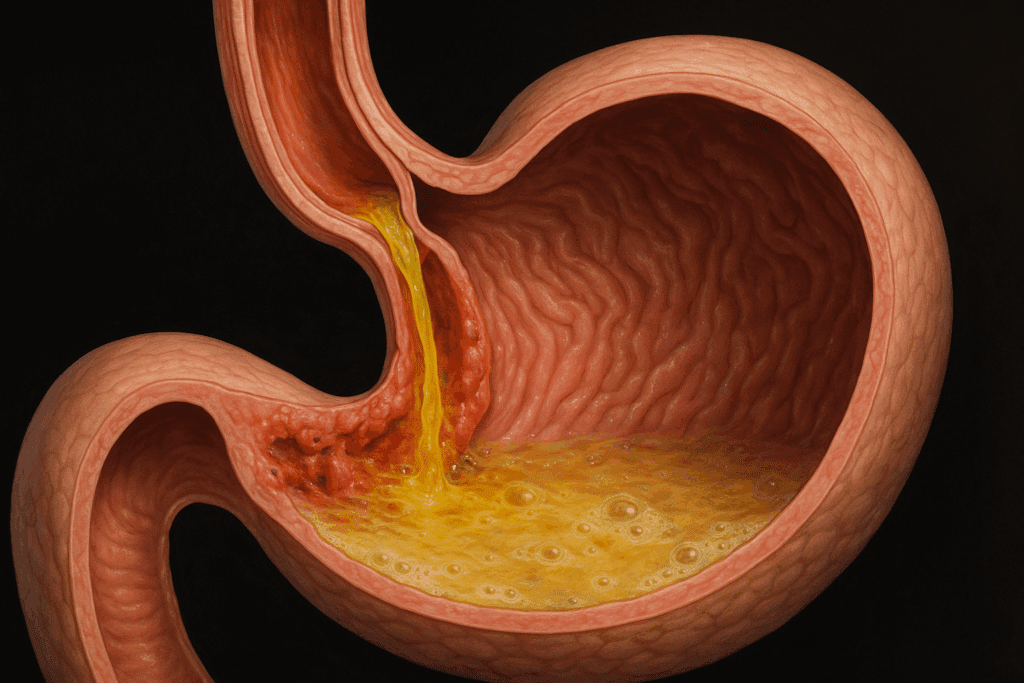
The Pathophysiology Behind Stage 4 Acid Reflux
At the heart of stage 4 acid reflux lies a complex interplay between physiological dysfunction and prolonged exposure to gastric contents in the esophagus. In a healthy digestive system, a ring-like muscle called the lower esophageal sphincter (LES) serves as a valve, opening to allow food into the stomach and closing to prevent its return into the esophagus. In GERD, and particularly in advanced cases, this sphincter becomes weakened or dysfunctional, failing to maintain the necessary barrier. The persistent backflow of acid damages the esophageal lining, triggering chronic inflammation, ulceration, and cellular changes.
Over time, this repeated exposure can lead to fibrosis, where scar tissue replaces healthy tissue, causing strictures or narrowing of the esophagus. Swallowing becomes difficult and painful, and the risk of aspiration into the lungs increases. Another hallmark of stage 4 acid reflux is Barrett’s esophagus, a condition in which the normal squamous cells lining the esophagus are replaced by columnar cells more commonly found in the intestines. This metaplasia is the body’s adaptive—but ultimately dangerous—response to chronic acid exposure, as it significantly raises the risk of developing esophageal adenocarcinoma. Thus, stage 4 acid reflux is not merely an escalation of symptoms but a distinct clinical entity with potentially life-altering consequences.

Warning Signs and Symptoms of Stage 4 Acid Reflux
Although acid reflux symptoms can often mimic other gastrointestinal conditions, stage 4 acid reflux tends to present with persistent and worsening signs that go beyond occasional heartburn. One of the most alarming symptoms is dysphagia, or difficulty swallowing, which may signal the presence of esophageal strictures or inflammation. Patients often describe the sensation of food getting “stuck” in the chest, accompanied by pain during swallowing, or odynophagia. Chronic cough, hoarseness, or a raspy voice—especially in the absence of a respiratory infection—can also point to advanced reflux, as stomach acid irritates the vocal cords and upper respiratory tract.
Unintended weight loss is another red flag, often due to reduced appetite, food avoidance, or impaired nutrient absorption caused by esophageal damage. Recurrent chest pain that mimics angina but occurs after eating or when lying down is frequently reported, and though it may be mistaken for cardiac issues, this pain is usually of gastrointestinal origin in GERD patients. Additionally, vomiting or regurgitation of undigested food or bile, particularly during sleep, can increase the risk of aspiration pneumonia and requires immediate medical attention. Recognizing these symptoms is vital not only for symptom control but also for preventing the further progression of tissue damage and cancer risk.
Diagnostic Strategies for Stage 4 GERD and Advanced Acid Reflux
Accurate diagnosis of stage 4 acid reflux requires a combination of clinical evaluation, symptom history, and specialized diagnostic tools. Endoscopy remains the gold standard in assessing esophageal damage. During this procedure, a flexible tube with a camera is inserted through the mouth to visualize the esophagus, allowing physicians to detect inflammation, ulcers, strictures, or evidence of Barrett’s esophagus. In some cases, biopsies are taken to confirm metaplastic changes or to rule out malignancy.
Another valuable diagnostic tool is ambulatory pH monitoring, which measures the frequency and duration of acid reflux episodes over a 24 to 48-hour period. This test is especially useful when symptoms are present, but endoscopic findings are inconclusive. Esophageal manometry is also used to evaluate the function of the LES and the peristaltic activity of the esophageal muscles, which can help guide treatment decisions. Barium swallow studies, where the patient ingests a contrast liquid visible on X-rays, can identify structural abnormalities, such as hiatal hernias or strictures. These comprehensive diagnostic techniques ensure that treatment plans for stage 4 GERD are based on objective findings rather than subjective symptoms alone, leading to more targeted and effective interventions.
Stage 4 Acid Reflux and Its Relationship with Barrett’s Esophagus
A particularly concerning complication of stage 4 acid reflux is the development of Barrett’s esophagus. This condition is characterized by a transformation of the esophageal lining from its normal squamous epithelial cells to columnar cells, which are more resistant to acid but have a higher risk of becoming cancerous. Barrett’s esophagus is considered a precancerous condition, and its detection significantly alters the management of GERD. Although not every patient with stage 4 acid reflux develops Barrett’s, the risk increases with the severity and duration of acid exposure.
Routine surveillance is essential for individuals diagnosed with Barrett’s esophagus. Regular endoscopic evaluations are recommended to monitor for dysplasia, or abnormal cell growth, which may indicate progression toward esophageal cancer. The presence of Barrett’s does not guarantee cancer development, but it does necessitate a more aggressive and proactive approach to treatment. In some cases, patients may undergo radiofrequency ablation or endoscopic mucosal resection to remove precancerous cells and reduce malignancy risk. The link between stage 4 acid reflux and Barrett’s underscores the importance of early detection and highlights the need for long-term follow-up in patients with advanced GERD.
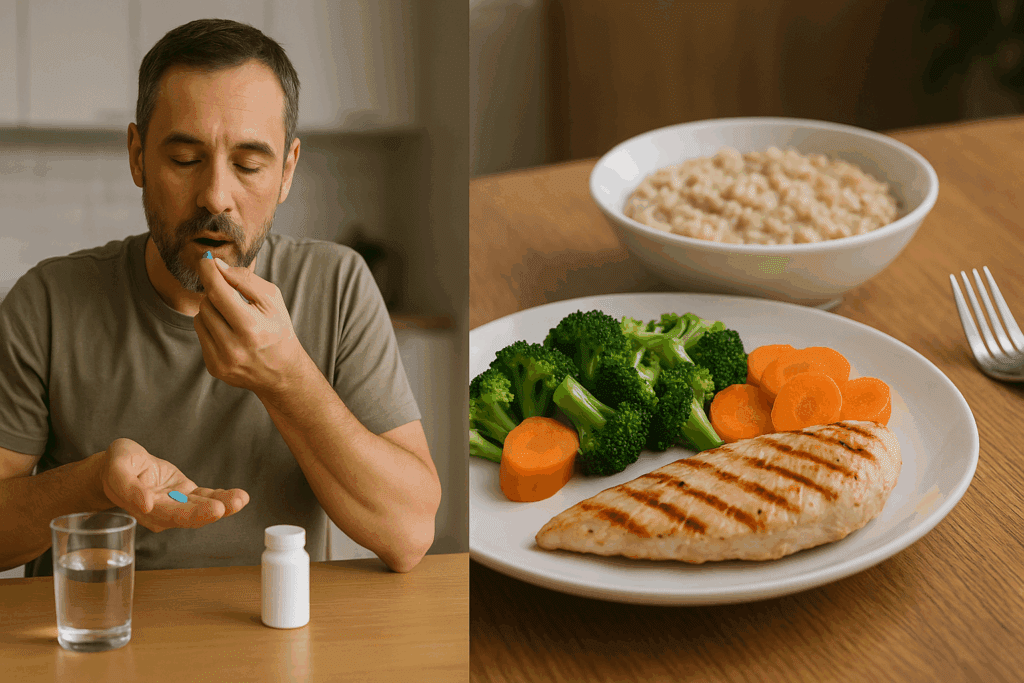
Treatment Approaches for Stage 4 GERD: Medical and Lifestyle Strategies
Managing stage 4 GERD requires a comprehensive approach that combines pharmacological intervention with significant lifestyle changes. The cornerstone of medical treatment is the use of proton pump inhibitors (PPIs), which reduce gastric acid production and promote healing of the esophageal lining. However, in stage 4 cases, the effectiveness of PPIs may be limited, and long-term use raises concerns about nutrient malabsorption, kidney function, and bone density. As such, physicians often tailor medication regimens, combining PPIs with prokinetics to improve gastric motility and reduce reflux episodes.
Lifestyle modifications are equally critical in managing stage 4 acid reflux. Patients are advised to adopt an anti-reflux diet, avoiding foods that relax the LES, such as caffeine, chocolate, peppermint, and high-fat meals. Eating smaller, more frequent meals and avoiding food intake close to bedtime can significantly reduce nighttime reflux. Elevating the head of the bed, wearing loose-fitting clothing, and maintaining a healthy body weight also contribute to symptom relief. These non-pharmacologic strategies are not merely adjuncts to medication but essential pillars of long-term management, particularly in preventing further esophageal damage.

Surgical Interventions and Advanced Therapies for Stage 4 Acid Reflux
When lifestyle changes and medications fail to adequately control symptoms or halt disease progression, surgical intervention may become necessary. One of the most widely performed surgical procedures for severe GERD is the Nissen fundoplication. In this operation, the upper part of the stomach is wrapped around the lower esophagus to reinforce the LES and prevent reflux. This procedure can be performed laparoscopically and has demonstrated long-term efficacy in reducing acid exposure, improving symptoms, and enhancing quality of life. However, as with any surgery, it carries risks such as difficulty swallowing, gas-bloat syndrome, or slippage of the wrap, which may require further correction.
Another emerging option is the LINX device, a ring of magnetic beads implanted around the LES to augment its barrier function. The magnetic attraction between the beads keeps the sphincter closed but allows it to open for swallowing. Unlike fundoplication, the LINX system preserves the ability to belch or vomit and can be removed if necessary. For patients with Barrett’s esophagus and signs of dysplasia, endoscopic ablative therapies such as radiofrequency ablation or cryotherapy may be employed to eradicate abnormal cells and prevent malignant transformation. These therapies represent a shift toward organ-sparing, minimally invasive interventions that address both the functional and oncological aspects of stage 4 acid reflux.
Stage 4 GERD Treatment Considerations in Older Adults and High-Risk Patients
The management of stage 4 GERD must be tailored to individual patient profiles, particularly in older adults or those with comorbidities that may complicate standard treatments. Age-related changes in gastrointestinal motility, decreased salivary production, and polypharmacy can all influence how symptoms manifest and how patients respond to therapy. Older patients may also be more susceptible to the adverse effects of long-term PPI use, including increased risk of fractures, Clostridium difficile infection, and renal impairment.
In this population, treatment goals often shift toward maximizing comfort, preserving nutritional status, and minimizing invasive interventions unless absolutely necessary. Non-pharmacologic strategies gain particular importance here, as they can be employed with fewer risks. When surgical intervention is indicated, careful preoperative evaluation is essential to assess cardiopulmonary fitness and anesthesia risk. Shared decision-making between the patient, family, and healthcare providers plays a crucial role in ensuring that the selected treatment aligns with the patient’s overall health status, values, and goals of care.
Psychological and Quality of Life Impact of Living with Stage 4 Acid Reflux
Living with stage 4 acid reflux goes far beyond the physical symptoms—it also deeply impacts emotional well-being, social functioning, and overall quality of life. The chronic nature of the condition, combined with dietary restrictions and anxiety about disease progression or cancer risk, can lead to emotional distress. Many individuals report feelings of frustration, isolation, or even depression, especially when their symptoms are not adequately managed despite significant effort. The unpredictability of symptom flare-ups may interfere with professional obligations, travel, or social engagements, compounding the psychological burden.
Furthermore, sleep disturbances caused by nocturnal reflux contribute to daytime fatigue and impaired concentration. Some patients may also experience food-related anxiety, avoiding meals or entire food groups out of fear of triggering symptoms. This avoidance can contribute to weight loss, nutrient deficiencies, and disordered eating patterns. Multidisciplinary care that includes psychological support, such as counseling or cognitive-behavioral therapy, can be immensely beneficial. Integrating mental health care into GERD treatment plans ensures a more holistic approach, recognizing that digestive health and emotional well-being are deeply intertwined.

The Role of Nutrition in Managing Stage 4 Acid Reflux
A strategic approach to nutrition can be one of the most powerful tools in managing stage 4 acid reflux. While there is no single GERD diet that works for everyone, evidence supports the avoidance of trigger foods known to relax the LES or increase gastric acidity. These include spicy foods, acidic fruits like citrus and tomatoes, caffeine, alcohol, chocolate, and carbonated beverages. A plant-forward, low-acid diet rich in fiber, non-citrus fruits, vegetables, and whole grains has shown promise in reducing reflux symptoms and promoting esophageal healing.
Protein intake is another important consideration. Lean proteins such as poultry, fish, tofu, and legumes are less likely to trigger reflux than high-fat cuts of meat. Cooking methods also matter—grilling, baking, or steaming foods rather than frying them can reduce symptom severity. In some cases, patients may benefit from working with a registered dietitian to create a personalized meal plan that meets their nutritional needs while minimizing discomfort. Small, frequent meals tend to be better tolerated than large portions, and mindful eating practices—such as chewing slowly and avoiding overeating—further aid digestion. A focus on nutrition is not only a symptom-management strategy but also an essential aspect of restoring gastrointestinal function and preventing further esophageal damage.
Long-Term Monitoring and Surveillance in Stage 4 GERD
One of the defining features of stage 4 acid reflux is its chronicity and potential for serious complications, making long-term monitoring an essential component of care. Regular follow-ups with a gastroenterologist allow for assessment of treatment efficacy, adjustment of medications, and monitoring for progression to dysplasia or cancer. Patients with Barrett’s esophagus, in particular, require a structured surveillance program that includes periodic endoscopies, typically every three to five years for non-dysplastic Barrett’s and more frequently if dysplasia is present.
In addition to clinical monitoring, laboratory evaluations may be conducted to assess for complications of long-term medication use. For example, patients on high-dose PPIs may need monitoring of magnesium, calcium, and vitamin B12 levels, as deficiencies can occur over time. Bone density scans might also be considered in postmenopausal women or elderly men with prolonged PPI use. Importantly, patient education is a cornerstone of successful long-term management. Teaching patients to recognize warning signs such as worsening dysphagia, unexplained weight loss, or chest pain ensures that they seek timely evaluation and intervention. Proactive surveillance empowers both patients and providers to act decisively before serious complications develop.
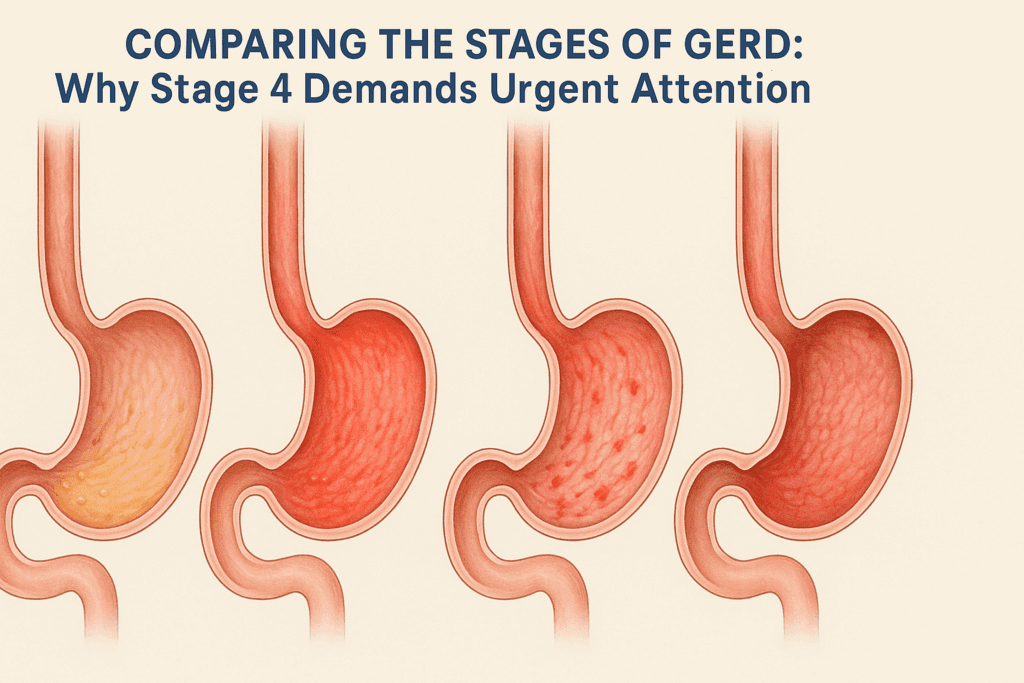
Comparing the Stages of GERD: Why Stage 4 Demands Urgent Attention
The stages of GERD illustrate the progressive nature of acid reflux and reinforce why early intervention is so critical. Stage 1, typically referred to as episodic or mild GERD, involves occasional heartburn or regurgitation, often triggered by dietary choices or stress. Many people in this stage may not seek medical care, instead relying on lifestyle adjustments or over-the-counter remedies. Stage 2 signals the beginning of chronic reflux, with symptoms occurring more than twice a week and starting to interfere with daily life. Medical evaluation and treatment typically become necessary at this stage.
Stage 3 represents a turning point, where visible esophageal damage becomes more common, and symptoms may persist despite medications. At this stage, complications such as erosive esophagitis may arise, and patients often undergo more intensive treatment or evaluation. Stage 4 acid reflux, however, is a distinct clinical entity with significant anatomical changes and increased oncological risk. It often involves complications such as strictures, Barrett’s esophagus, and even early cancer in some cases. Unlike the earlier stages, where the focus may be symptom relief, stage 4 management centers on preventing irreversible damage and life-threatening complications. Recognizing the escalation between these stages helps underscore the importance of early diagnosis, ongoing management, and vigilant monitoring.
Understanding the Nuances of Stage 4 GERD Treatment
When exploring stage 4 GERD treatment, it’s essential to acknowledge that this stage cannot be approached with a one-size-fits-all model. Instead, a nuanced, personalized strategy must be developed in collaboration with a multidisciplinary team that may include gastroenterologists, surgeons, dietitians, and behavioral health professionals. Treatment decisions must take into account not only symptom severity but also the presence of structural complications, the risk of malignant transformation, patient comorbidities, and personal preferences.
A patient with Barrett’s esophagus and high-grade dysplasia may be a candidate for endoscopic mucosal resection or even esophagectomy in rare cases, whereas another patient with the same diagnosis but low-grade dysplasia might be managed with careful surveillance and acid suppression therapy. Similarly, a person with multiple failed medication trials may opt for surgical intervention, while others may respond to a revised lifestyle and dietary protocol. The importance of shared decision-making cannot be overstated here. Patients who understand their diagnosis, the rationale behind each treatment recommendation, and the long-term implications are more likely to adhere to treatment plans and achieve better outcomes.
Emerging Research and Innovations in GERD Management
The landscape of GERD treatment is continually evolving, with emerging research offering hope for more precise, effective, and less invasive interventions. Advances in endoscopic technologies have enabled earlier detection of precancerous lesions and more targeted therapies. Techniques such as transoral incisionless fundoplication (TIF) and Stretta radiofrequency therapy offer promising alternatives for patients who are not ideal candidates for traditional surgery. These interventions are less invasive and associated with quicker recovery times and fewer side effects.
Biological therapies are also being explored, particularly in cases where inflammation plays a prominent role in symptom exacerbation. Researchers are investigating whether modifying the esophageal microbiome might influence disease progression or symptom severity, given the growing recognition of the gut microbiota’s role in overall health. In addition, artificial intelligence and machine learning tools are being incorporated into endoscopic diagnostics to enhance the detection of subtle mucosal changes that may indicate early Barrett’s or dysplasia. These innovations signal a future in which GERD treatment is more personalized, precise, and preventive.
Frequently Asked Questions About Managing and Understanding Stage 4 Acid Reflux
What lifestyle changes make the biggest impact in managing stage 4 acid reflux?
While dietary shifts are foundational in treating acid reflux, those at stage 4 often require more nuanced lifestyle modifications to see meaningful improvement. One of the most impactful strategies is adjusting sleep position—not simply sleeping with the head elevated, but using a wedge pillow or adjusting the entire bed frame to maintain a 30- to 45-degree incline. This significantly reduces nocturnal reflux events and the risk of aspiration. Beyond dietary triggers, managing chronic stress plays a critical role, as cortisol and adrenaline can disrupt gastric emptying and exacerbate reflux symptoms. Mind-body interventions such as mindfulness meditation, diaphragmatic breathing, or even paced yoga tailored to gastrointestinal health have demonstrated improvements in symptom frequency and severity in advanced cases. For individuals with stage 4 acid reflux, the goal is not just to avoid flare-ups but to consistently support the entire digestive process across sleep, stress, and movement patterns.
How is stage 4 GERD treatment different for individuals with a history of autoimmune disease?
Patients with autoimmune conditions like scleroderma, lupus, or Sjögren’s syndrome often experience GERD differently, and stage 4 gerd treatment must reflect those unique physiological challenges. For instance, scleroderma can severely weaken esophageal motility and further impair the function of the lower esophageal sphincter, accelerating progression through the stages of GERD. In these individuals, surgical options may carry higher risks, so conservative management—including compounded medications tailored for esophageal transit—may be prioritized. Nutritional strategies are also adjusted to address malabsorption or inflammatory triggers, often involving coordination with a rheumatologist. Because many autoimmune patients are immunosuppressed, surveillance protocols for Barrett’s esophagus or esophageal strictures may occur at shorter intervals to mitigate their elevated cancer risk.
Can stage 4 acid reflux affect areas beyond the esophagus?
Yes, the complications of stage 4 acid reflux can extend well beyond the esophagus and involve multiple systems. One overlooked effect is chronic laryngeal and pharyngeal inflammation, which can result in persistent hoarseness, throat clearing, or a sensation of a lump in the throat—often mistaken for anxiety-related symptoms. Additionally, microaspiration of gastric contents during sleep can lead to recurrent respiratory infections, asthma exacerbations, or even chronic sinusitis. Over time, poor nutrient absorption caused by inflammation and dietary limitations can impact metabolic and immune function, leading to fatigue or anemia. Cardiovascular health may also be indirectly affected, as the systemic inflammation and poor sleep associated with stage 4 acid reflux are both known contributors to heart disease. Understanding this broader scope is essential for comprehensive care and interdisciplinary management.
How do clinicians determine the best surgical approach for stage 4 GERD?
Selecting a surgical intervention for advanced GERD isn’t based solely on symptom severity but involves a multidimensional assessment. Clinicians consider esophageal motility tests, imaging studies, and overall patient resilience before recommending options like Nissen fundoplication or magnetic sphincter augmentation. If the esophagus exhibits severely impaired peristalsis, a partial wrap or a LINX device may be preferable to reduce postoperative dysphagia. For patients with Barrett’s esophagus, surgeons weigh the benefits of fundoplication against the need for concurrent or staged endoscopic interventions. Additionally, patient preferences play a larger role at this stage, with shared decision-making models helping determine whether a minimally invasive or more definitive anatomical correction is appropriate. Each procedure has different profiles regarding symptom control, side effects, and reversibility, making individualized planning essential in stage 4 GERD treatment.
What are the cognitive and emotional side effects of long-term untreated stage 4 acid reflux?
Living with untreated stage 4 acid reflux can exert a considerable toll on cognitive and emotional well-being, especially when sleep is consistently disrupted. Individuals may experience brain fog, irritability, and slowed cognitive processing due to the effects of nocturnal reflux on sleep quality. There’s also a higher incidence of anxiety and depressive symptoms among GERD patients, particularly when symptoms are unpredictable or socially limiting. Moreover, the dietary restrictions and fear of eating can lead to disordered eating patterns or social withdrawal, reducing life satisfaction. These effects are often compounded by the stigma or lack of public understanding of how serious advanced reflux can be. Addressing these symptoms may require collaboration with a mental health professional familiar with chronic illness, emphasizing that emotional support is not ancillary but integral to managing advanced stages of GERD.
Why does stage 4 acid reflux often require a multidisciplinary care team?
Due to its complexity and systemic implications, stage 4 acid reflux typically requires a team-based approach involving several specialties. Gastroenterologists handle diagnostics, medication management, and surveillance for Barrett’s esophagus or dysplasia. Surgeons step in when anatomical correction is necessary. Dietitians play a critical role in maintaining nutritional adequacy amidst food restrictions, especially when weight loss or nutrient deficiencies arise. Mental health professionals help address the psychological burden of chronic illness, which is often underestimated. Some patients may also require pulmonologists or otolaryngologists if complications like aspiration pneumonia or vocal cord damage develop. The coordinated effort of these professionals ensures that care is not only reactive but proactively designed to prevent complications and support long-term quality of life.
What emerging technologies may redefine how we treat stage 4 GERD in the future?
Several cutting-edge technologies are poised to revolutionize how we approach advanced GERD. One such innovation is AI-assisted endoscopy, which uses machine learning algorithms to detect microscopic changes in esophageal tissue, enabling earlier and more accurate identification of Barrett’s esophagus or dysplasia. Additionally, robotic-assisted surgical techniques are enhancing precision and reducing recovery times for procedures like fundoplication. Implantable pH-monitoring capsules and motility sensors now allow for non-invasive, real-time tracking of reflux events over extended periods, offering better diagnostic accuracy without disrupting daily life. Pharmacogenomics is also emerging as a tool to tailor medication types and dosages based on genetic metabolism profiles, minimizing side effects and maximizing therapeutic efficacy. As these technologies evolve, they promise not only more personalized treatment plans but also earlier intervention—potentially halting progression before reaching stage 4 acid reflux.
Navigating the Psychological Toll of Stage 4 Acid Reflux
The emotional burden of stage 4 acid reflux is often invisible but profound. For many, the experience of chronic symptoms fosters a constant state of hyper-vigilance—worrying about what to eat, how to sleep, or whether a seemingly benign symptom could be a warning sign of cancer. Over time, this can evolve into health anxiety or medical PTSD, especially in those who have undergone multiple invasive procedures. The feeling of losing control over one’s body, particularly in a digestive system that was once taken for granted, can provoke deep frustration or even hopelessness. Counseling and support groups provide invaluable tools to reframe the patient experience, offering coping mechanisms rooted in empowerment rather than fear. Importantly, integrating behavioral therapy with physical treatment enhances compliance and long-term outcomes, reminding patients that addressing the mind is not secondary—it’s essential to healing the body.
How do the stages of acid reflux influence treatment timelines and urgency?
Understanding the stages of acid reflux is critical for designing a timely and effective treatment plan. In the early stages, interventions often focus on lifestyle changes and occasional medication use, with treatment urgency tied to symptom severity rather than structural damage. As patients progress to mid-level stages, where esophageal inflammation becomes visible on endoscopy, regular monitoring and more consistent pharmacologic therapy become essential. By stage 4, the urgency dramatically increases due to the potential for permanent anatomical changes and the elevated cancer risk. At this point, proactive management—including surveillance endoscopy and possibly surgical or ablative therapy—shifts from symptom control to life preservation. Recognizing the progressive nature of GERD helps clinicians and patients act decisively, potentially reversing damage before complications arise.
When does stage 4 gerd treatment require nutritional intervention by a specialist?
Nutritional intervention is often overlooked until stage 4 GERD treatment reaches a point where weight loss, malabsorption, or food aversion becomes evident. At this stage, patients may have adopted restrictive eating patterns that compromise macronutrient and micronutrient intake. Dietitians can identify subtle deficiencies—such as low magnesium or vitamin B12 levels—often linked to long-term PPI use. Specialized meal planning helps patients consume foods that are not only reflux-safe but also nutritionally dense, ensuring sustained energy and immune support. Enteral nutrition may even be considered in extreme cases where swallowing is impaired due to strictures. Collaborating with a nutrition professional ensures that food becomes a source of healing rather than fear, restoring confidence and helping patients maintain their strength through ongoing treatment.
Final Thoughts: Managing Stage 4 Acid Reflux with Vigilance, Compassion, and Strategy
Stage 4 acid reflux is not just an advanced phase of a common digestive condition—it is a complex, potentially life-altering diagnosis that requires comprehensive and proactive care. The journey through the stages of GERD can be gradual or rapid, but when stage 4 is reached, the stakes are significantly higher. It demands not only medical expertise but also a compassionate understanding of the physical and emotional burdens patients carry. Addressing stage 4 GERD means implementing a strategy that spans dietary management, pharmacological precision, surgical interventions when warranted, and vigilant surveillance for complications such as Barrett’s esophagus or malignancy.
Equally important is the recognition that successful treatment goes beyond acid suppression. It involves addressing the psychological toll, ensuring nutritional adequacy, supporting patient education, and incorporating the latest advancements in medical technology. By focusing on these essential facts about stage 4 acid reflux, patients and providers can work together to improve digestive health outcomes, prevent further complications, and ultimately reclaim a better quality of life. In a condition where early warning signs often go ignored, the pathway to healing begins with awareness, courage, and an unwavering commitment to care.


