Food is often a source of comfort, pleasure, and cultural identity. But for a growing number of adults, eating has become a perplexing challenge. Imagine enjoying a favorite meal, only to experience discomfort, bloating, hives, or even difficulty breathing shortly after. This is the reality for many facing what appears to be a sudden food intolerance in adults. These emerging dietary sensitivities can strike without warning, leading to confusion, distress, and a need for new dietary habits. As research into food sensitivities and intolerances advances, we are beginning to understand the complex interplay between the immune system, the gut, and environmental factors that influence our body’s reaction to food. For adults, particularly those without a history of childhood allergies, the experience can feel both surprising and isolating.
While food allergies are more widely discussed, the nuances of food intolerance remain less understood. Yet the effects can be just as disruptive to everyday life. Differentiating between a food allergy and a food intolerance is crucial for receiving proper diagnosis and treatment. In this article, we will explore what defines a food intolerance in simple terms, the difference between food allergies and intolerances, signs of food intolerance and food sensitivity symptoms, and what causes these conditions to develop later in life. We will also examine the common food intolerances that impact adults and offer insights into how to manage symptoms and rebuild a healthy relationship with food.
You may also like: Macronutrients vs Micronutrients: What the Simple Definition of Macronutrients Reveals About Your Diet and Health
What Is Food Intolerance? A Simple, Yet Important Definition
To begin understanding this topic, it helps to establish a clear and medically sound food intolerance definition. In foods, a food intolerance is typically a non-immunological reaction that occurs when the body has difficulty digesting certain components, such as lactose, gluten, or food additives. Unlike an allergic reaction to food, which involves the immune system and can trigger potentially life-threatening symptoms, a food intolerance does not involve an immune response. Instead, it results from enzyme deficiencies, chemical sensitivities, or malabsorption problems within the gastrointestinal tract. This is the core difference that distinguishes food intolerance from a food allergy.
In the simplest terms, the short definition of food intolerance could be described as the body’s inability to properly process or metabolize specific food ingredients, leading to unpleasant symptoms. This food intolerance simple term is crucial because it helps remove the confusion between an allergic reaction and intolerance. Many individuals mistakenly use the terms interchangeably, which can delay appropriate care. Clarifying this difference early on can help adults better identify the signs of food intolerance and avoid unnecessary panic when symptoms arise.

Recognizing Food Intolerance Symptoms and Food Sensitivity Signs
The symptoms of a food intolerance can vary widely and often depend on the type of food involved. Commonly reported food intolerance symptoms include abdominal pain, bloating, gas, diarrhea, and nausea. These reactions are usually delayed and may occur several hours after consuming the offending food. Because of the nonspecific nature of these symptoms, many people mistake them for unrelated digestive problems or attribute them to stress. This leads to a cycle of continued exposure and symptom persistence until the connection is finally recognized.
Food sensitivity symptoms, although similar, are sometimes broader in scope. They may also include headaches, brain fog, fatigue, and joint pain. These systemic responses suggest that food sensitivities, though not classically allergic, still influence multiple systems within the body. For example, certain food additives like sulfites or monosodium glutamate (MSG) can trigger neurological and cardiovascular responses in sensitive individuals. By recognizing the early signs of food intolerance and food sensitivity symptoms, adults can start to track their reactions and seek appropriate testing and guidance.
Understanding Food Allergy Symptoms and Their Distinct Nature
To distinguish a food intolerance from an allergy, it’s critical to understand the mechanisms and symptoms of allergic reactions. A true food allergy involves an immune system response, typically mediated by immunoglobulin E (IgE) antibodies. When a person with a food allergy consumes the allergen, the immune system launches a defensive attack, releasing histamines and other chemicals that can cause a rapid and severe reaction.
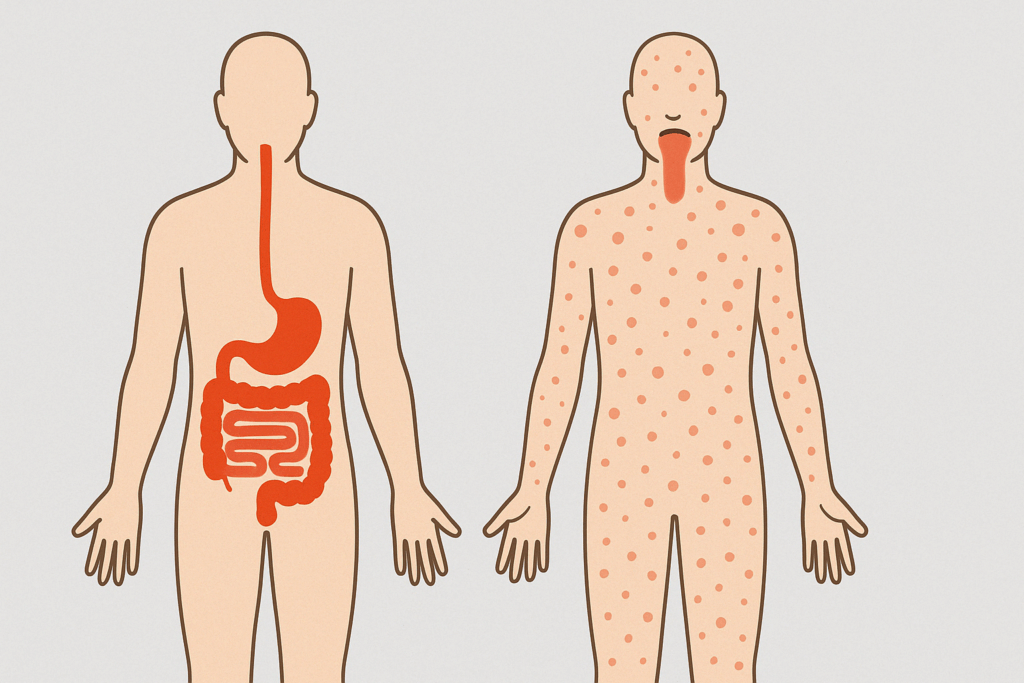
Common food allergy symptoms include hives, swelling of the lips or tongue, difficulty breathing, vomiting, and in some cases, anaphylaxis—a life-threatening condition that requires immediate medical intervention. Anaphylaxis definition in food and nutrition contexts refers to a sudden, systemic allergic reaction that can lead to airway obstruction, a dangerous drop in blood pressure, and shock. In contrast to food intolerance, where symptoms are often delayed and primarily digestive, food allergy effects can appear within minutes and affect the skin, respiratory system, gastrointestinal tract, and cardiovascular function.
Three symptoms of food allergy that commonly present in an emergency setting include swelling (particularly in the face or throat), rash from food allergy (often appearing as raised welts or food allergy hives), and respiratory distress. Knowing these classic signs of allergic reaction to food is essential, especially for individuals at risk or those who have never experienced such symptoms before.
Is It Rare to Not Be Allergic to Any Food?
This question often emerges when discussing food reactions: is it rare to not be allergic to any food? Statistically speaking, food allergies affect a significant but minority portion of the population. According to current estimates, about 5–8% of children and roughly 4% of adults in the United States have a diagnosed food allergy. Therefore, it is not particularly rare to live without any food allergies. In fact, the majority of adults are not allergic to any food, although this does not preclude them from developing food sensitivities or intolerances.
However, just because someone has never had an allergic reaction to food does not mean they are immune to future reactions. Allergies and intolerances can develop at any age due to a variety of genetic, environmental, and lifestyle factors. Adults may develop food sensitivities or allergic reactions later in life, even without a prior history. This phenomenon is part of what makes sudden food intolerance in adults so confusing. For those who have eaten a particular food their whole lives without issue, the abrupt onset of symptoms can feel inexplicable and unsettling.
What Are Three Systems of a Food Allergy?
When a person experiences an allergic reaction to food, the body’s immune response can involve several systems simultaneously. Understanding what are three systems of a food allergy can help clarify how widespread the effects of a reaction can be. First, the integumentary system, or the skin, often reacts with symptoms such as food allergy hives, redness, or rash from food allergy. These are typically among the first visible signs.
Second, the respiratory system may be affected. Individuals can experience nasal congestion, wheezing, throat tightness, or full-blown anaphylaxis. Third, the gastrointestinal system may also respond with nausea, vomiting, abdominal cramping, or diarrhea. Recognizing the impact across these three systems is vital in understanding the urgency and seriousness of allergic reactions. Even mild food allergy symptoms can escalate quickly if the immune system is severely triggered.

The Growing Reality of Sudden Food Intolerance in Adults
It used to be widely assumed that if a person wasn’t allergic to something as a child, they were unlikely to develop problems later in life. However, research and clinical practice now show that sudden food intolerance in adults is increasingly common. There are several possible explanations for this shift. One major factor is changes in the gut microbiome, which can alter how the digestive system processes food. Antibiotic use, chronic stress, and changes in diet can disrupt microbial balance, leading to inflammation and food-related sensitivities.
Additionally, cumulative exposure to certain foods over a lifetime may eventually overwhelm the body’s tolerance. For instance, many people who develop lactose intolerance do so in adulthood as the body naturally produces less lactase enzyme with age. Other cases may arise from heightened immune reactivity due to autoimmune conditions or chronic inflammation. The prevalence of additives and preservatives in modern diets also plays a role in triggering non-allergic food reactions.
Food Sensitivities and Intolerances: A Diagnostic Challenge
Diagnosing food sensitivities and intolerances can be a complex endeavor. Unlike food allergies, which can be detected with blood tests or skin prick tests, intolerances often require elimination diets and careful symptom tracking. This is partly because food intolerance symptoms are delayed and less predictable, making it hard to identify a single culprit. Functional medicine practitioners often employ comprehensive food panels and gut health assessments to explore underlying causes.
Another layer of complexity is that food sensitivities and intolerances are often intertwined. For example, someone may be intolerant to gluten due to celiac disease, an autoimmune disorder, or they may have non-celiac gluten sensitivity, which presents similarly but lacks a clear biomarker. The lack of definitive tests for many intolerances means that clinical judgment and patient history play a large role in diagnosis. This emphasizes the importance of working with a knowledgeable healthcare provider who understands the full spectrum of dietary intolerance.

Common Food Intolerances and Their Impact on Wellness
Among the most common food intolerances in adults are lactose, gluten, and FODMAPs—a group of fermentable carbohydrates that include fructose, lactose, and polyols. Lactose intolerance results from a deficiency of the enzyme lactase, which breaks down milk sugar. Symptoms often include bloating, gas, and diarrhea after consuming dairy. Gluten intolerance, while distinct from celiac disease, can still cause symptoms such as fatigue, brain fog, and abdominal discomfort.
FODMAP intolerance has gained recognition in recent years, particularly among individuals with irritable bowel syndrome (IBS). By following a low-FODMAP diet, many people experience relief from chronic digestive distress. Understanding and identifying these common food intolerances allows adults to make informed dietary choices and avoid unnecessary suffering. It also helps prevent nutrient deficiencies, as many who eliminate entire food groups without guidance may lack essential vitamins and minerals.
Signs of Food Allergies and the Importance of Medical Supervision
The signs of food allergies are often more immediate and dramatic than those of intolerances. Because they involve an immune response, they can be detected with standardized testing and require vigilant avoidance strategies. Signs of allergic reaction to food should never be ignored. Even mild reactions can escalate with repeated exposure. It is important for individuals to carry emergency medications like epinephrine if they have known food allergies.
Medical supervision is essential not only for diagnosis but also for long-term management. Many adults confuse food intolerance symptoms with allergic reactions, leading them to either overreact or underestimate their condition. By distinguishing between food allergies and food sensitivities, adults can adopt the right treatment protocols and avoid unnecessary dietary restrictions. Working with an allergist or dietitian can provide the clarity needed to navigate these complex conditions.

Understanding the Psychology of Dietary Intolerance
Experiencing a sudden dietary intolerance can trigger emotional and psychological distress. The fear of unknown reactions, the social implications of avoiding common foods, and the disruption of long-standing eating habits can significantly affect quality of life. Some individuals may develop food-related anxiety or even disordered eating patterns as a result of trying to control their symptoms. It is not uncommon for adults facing sudden food intolerance to feel isolated or frustrated when their condition is misunderstood.
A supportive environment that includes empathetic healthcare providers and informed family and friends can make a substantial difference. Counseling or support groups may also help individuals adjust emotionally to their new dietary landscape. Education plays a key role in empowering individuals to make confident food choices without succumbing to fear or misinformation. Understanding that food intolerance is a manageable condition can restore a sense of control and normalcy.
Empowering Adults to Navigate Their Dietary Needs
Empowerment begins with awareness. Recognizing the signs of food intolerance, identifying common triggers, and seeking appropriate medical guidance are critical steps toward reclaiming health. Keeping a food and symptom journal, reading ingredient labels, and experimenting with elimination diets under professional supervision can help identify problematic foods. Additionally, integrating gut-supportive practices like probiotic supplementation, stress reduction, and anti-inflammatory diets may improve tolerance over time.
While there is no universal cure for food sensitivities and intolerances, many people find relief through tailored nutrition plans. The key lies in understanding the difference between intolerance and allergy, responding to symptoms appropriately, and taking a holistic approach to healing. Personalized nutrition is rapidly becoming a cornerstone of preventive health, and for adults with food intolerance, this represents a promising path forward.
Rebuilding Your Relationship with Food After an Intolerance Diagnosis
Receiving a diagnosis of food intolerance can feel like a loss. Foods that once brought joy may now bring discomfort or fear. However, many individuals find that with time and guidance, they can rebuild their relationship with food. This process begins with knowledge. Understanding the food intolerance definition in foods, the mechanisms behind reactions, and the ways to manage symptoms restores a sense of agency.
Replacing problematic foods with nutrient-dense alternatives, discovering new recipes, and exploring diverse cuisines can turn what feels like a limitation into an opportunity for culinary discovery. Food, after all, is not only fuel but also culture, connection, and pleasure. With proper management, food can once again become a source of nourishment rather than distress.
Frequently Asked Questions: Understanding Sudden Food Intolerance in Adults and Related Food Sensitivities
1. Can emotional stress trigger sudden food intolerance in adults?
Yes, emotional stress can be a surprising yet significant factor in the onset of sudden food intolerance in adults. While food intolerance symptoms typically originate from digestive inefficiencies or chemical sensitivities, psychological stress has been shown to alter gut permeability and immune system function. This disruption may make the gastrointestinal system more sensitive to certain foods that were previously well-tolerated. In some individuals, chronic anxiety or trauma can also contribute to altered neuroimmune responses, which may amplify food sensitivity symptoms and create new food-related triggers. Therefore, managing stress through techniques like mindfulness, therapy, or relaxation exercises may reduce or prevent episodes of dietary intolerance.
2. What makes diagnosing food sensitivities and intolerances more difficult than diagnosing food allergies?
Unlike allergies that present acute food allergy symptoms such as hives or anaphylaxis, food sensitivity symptoms tend to be delayed and inconsistent. This makes it much harder to pinpoint the offending food without thorough tracking. Furthermore, many standard allergy tests do not detect non-IgE-mediated reactions, which are common in food sensitivities and dietary intolerance. The lack of validated biomarkers for many food intolerance types means that practitioners often rely on elimination diets, which can be time-consuming and inconclusive without professional oversight. This complexity highlights the need for personalized nutrition strategies and comprehensive symptom logs.
3. Are there new technologies emerging to detect food intolerance more accurately?
Yes, emerging technologies are gradually improving how we detect food intolerance in adults. Microbiome analysis, metabolomic profiling, and advanced IgG testing are being explored to identify patterns linked to dietary intolerance and chronic inflammation. While not yet universally accepted, these tools may eventually provide a deeper understanding of how food intolerance definition in foods is shaped by individual gut ecosystems. Wearable digestive trackers and digital elimination diet tools are also aiding users in identifying subtle reactions in real-time. However, clinical validation remains critical to differentiate between evidence-based tools and those offering limited scientific merit.
4. How can someone distinguish between common food intolerances and an allergic reaction to food when symptoms overlap?
While symptoms like stomach pain, fatigue, or skin irritation can occur in both conditions, an allergic reaction to food generally produces a faster, more intense response. The three symptoms of food allergy that are most commonly immediate include food allergy hives, respiratory difficulty, and swelling of the face or throat. In contrast, food intolerance symptoms are usually restricted to digestive upset and appear hours after consumption. Understanding what are three systems of a food allergy can help: the skin, respiratory, and gastrointestinal systems are all often affected. Individuals should seek medical evaluation, especially if signs of allergic reaction to food involve breathing difficulty or widespread rash from food allergy.
5. Why do some people experience food intolerance symptoms with healthy foods like fruits or vegetables?
Certain fruits and vegetables contain natural compounds, such as histamines, salicylates, or FODMAPs, that can trigger food sensitivity in susceptible individuals. These reactions fall under the umbrella of food sensitivities and intolerances rather than food allergies. For example, avocados and tomatoes are high in histamines and may cause headaches or skin flushing in people with histamine intolerance. Similarly, onions and apples contain FODMAPs that may aggravate irritable bowel syndrome. Understanding the broader context of food intolerance simple term classifications helps differentiate between nutrient-rich foods and how individual biochemistry responds to them.
6. Is it rare to not be allergic to any food, and what might that imply about the immune system?
Statistically, it is not rare to not be allergic to any food; in fact, the majority of the population does not experience food allergy effects. However, a lack of allergic reactions doesn’t necessarily mean the immune system is stronger or weaker. Instead, it may reflect a unique interplay of genetics, gut microbiota composition, and environmental exposures. While some people never develop what is a food allergy, they may still experience dietary intolerance or mild signs of food intolerance that don’t rise to the level of a full allergic response. Thus, immunity is nuanced and cannot be measured solely by the presence or absence of food-related reactions.
7. Can food sensitivities develop as a result of gut infections or antibiotic use?
Yes, both acute gastrointestinal infections and prolonged antibiotic use can disrupt the microbiome and gut lining integrity, leading to new food sensitivities or sudden food intolerance in adults. This microbial imbalance can impair digestion and increase gut permeability, allowing undigested food particles to provoke low-grade immune responses. Such reactions may manifest as food intolerance symptoms like bloating, fatigue, or joint pain. The connection between gut dysbiosis and food sensitivity underscores the importance of post-antibiotic recovery protocols, including the use of prebiotics, probiotics, and anti-inflammatory foods. A resilient gut often serves as a frontline defense against the emergence of food sensitivities and intolerances.
8. How might the social and emotional impact of food intolerance affect mental health?
Coping with food intolerance often extends beyond physical symptoms and affects social life, emotional well-being, and mental health. Individuals may experience food-related anxiety or depression due to the fear of accidental exposure or social isolation during meals. These emotional burdens can be compounded when food sensitivity symptoms are dismissed or misunderstood by others. Over time, this may lead to disordered eating patterns or hypervigilance around food. Integrating mental health support with dietary management can make a profound difference for those living with dietary intolerance, creating space for emotional recovery alongside physical healing.
9. Can you grow out of food sensitivities, or are they usually permanent?
Unlike classic allergies, which often persist for life, some food sensitivities can resolve over time, especially if the underlying cause is addressed. For instance, if food sensitivity was triggered by stress, gut inflammation, or nutrient deficiencies, healing those factors may reduce or eliminate symptoms. Rotational diets, gut-healing protocols, and microbiome diversity strategies have been effective in reducing sensitivity in many adults. However, permanent avoidance may still be necessary for more severe or persistent intolerances. Ongoing re-evaluation with a qualified professional ensures that dietary intolerance is managed dynamically rather than through overly restrictive approaches.
10. How can travelers manage food intolerance and reduce the risk of an allergic reaction food allergy while abroad?
Managing food intolerance or signs of food allergies while traveling requires advanced planning. Travelers should research local ingredients, prepare translations for dietary restrictions, and consider packing safe snacks or enzyme supplements when possible. For those with a history of allergic reaction to food, carrying antihistamines and an epinephrine auto-injector is essential. Identifying the signs of allergic reaction to food quickly—such as swelling, rash from food allergy, or difficulty breathing—can make a critical difference in accessing prompt care. Whether dealing with food intolerance symptoms or food allergy effects, maintaining awareness and preparation allows travelers to explore the world with greater safety and confidence.
Closing Reflections: Embracing Awareness and Action in Food Intolerance Management
Understanding sudden food intolerance in adults requires a nuanced appreciation of both biology and behavior. By learning the food intolerance simple definition, recognizing food sensitivity symptoms, and distinguishing them from food allergy symptoms, individuals can navigate their health more confidently. Identifying signs of food intolerance and allergic reaction to food is not just about symptom control; it’s about enhancing overall well-being and preventing long-term complications.
Food intolerance symptoms may be inconvenient, but they offer an important message about the body’s internal state. Just as food has the power to heal, it can also harm when mismatched with our unique physiology. Recognizing the signs of food allergies, differentiating food intolerance from allergic reaction food allergy events, and knowing what are three systems of a food allergy empowers adults to respond appropriately and seek the help they need. Whether you experience food allergy hives or the bloating of a common food intolerance, your body’s signals deserve to be heard.
By embracing both medical insight and personal experience, individuals can reclaim a healthier relationship with food. It is through this awareness that people can move from confusion and frustration to clarity and empowerment. With expert guidance and self-awareness, even the most sudden and perplexing food reactions can become manageable, and the journey back to wellness can begin with confidence and compassion.
Further Reading:
The 8 Most Common Food Intolerances
Food Sensitivity, Intolerance, or Allergy: What’s the Difference?


