Introduction: A New Frontier in Diabetes Research
In recent years, the global medical community has intensified its focus on the gut microbiome as a significant factor in metabolic health. Diabetes, a condition long associated with insulin resistance and blood glucose control, is now being reevaluated through a new lens—that of microbial ecology. Among the most intriguing developments in this evolving landscape is the discovery of how nocturnal bacteria may influence diabetes, especially through species like Prevotella that dominate the microbial terrain during nighttime metabolic processes. As science digs deeper into this nocturnal microbial world, emerging evidence suggests that the gut microbiota does not merely passively coexist within us but plays an active role in shaping metabolic pathways, particularly those associated with type 2 diabetes. The rise in interest surrounding terms like “nocturnal bacteria diabetes,” “diabetic gut,” and “Prevotella and diabetes” is a testament to this paradigm shift.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
Understanding the Diabetic Gut and Its Unique Microbial Environment
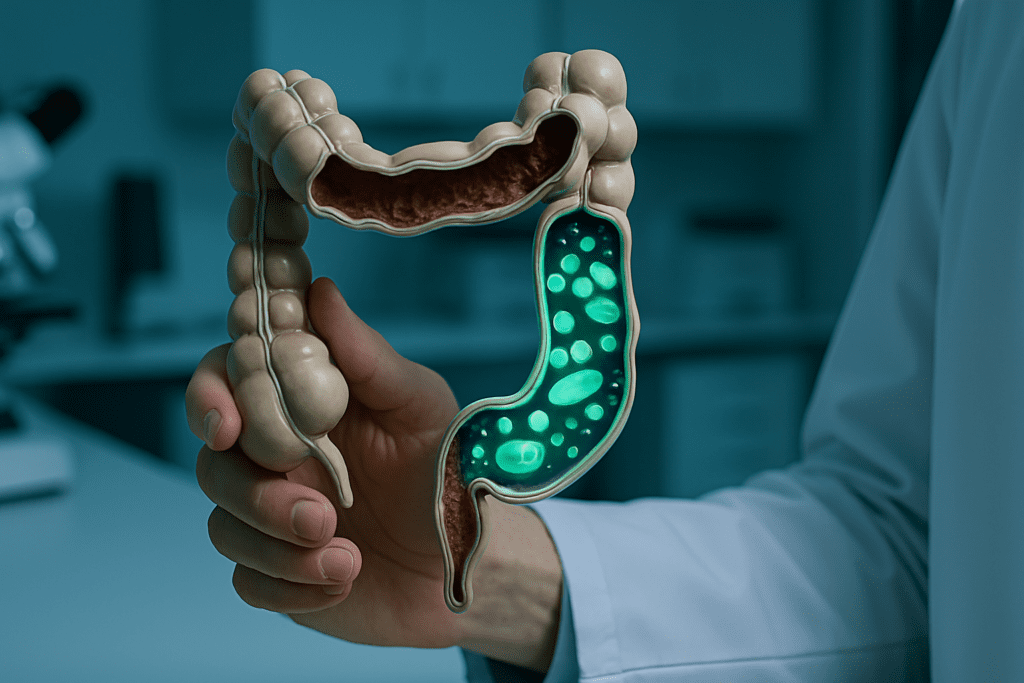
The human gut harbors trillions of microorganisms that form a complex ecosystem known as the gut microbiota. In individuals with diabetes, this ecosystem exhibits distinctive characteristics that separate it from that of non-diabetic individuals. Often referred to as the “diabetic gut,” this altered microbiome is marked by reduced microbial diversity and an imbalance between beneficial and pathogenic bacterial strains. One of the most significant changes observed is a shift in the Firmicutes-to-Bacteroidetes ratio, which plays a vital role in metabolic homeostasis. This dysbiosis—an imbalance in the microbial community—is not merely a byproduct of diabetes but a potential contributor to its onset and progression.
Recent studies have shown that the diabetic gut exhibits heightened levels of inflammatory markers, potentially stemming from the overrepresentation of opportunistic pathogens and underrepresentation of commensal bacteria that produce anti-inflammatory short-chain fatty acids (SCFAs). These SCFAs, particularly butyrate, are crucial for maintaining gut barrier integrity and regulating immune function. The absence or depletion of SCFA-producing bacteria compromises these protective mechanisms, creating a pro-inflammatory environment conducive to insulin resistance. Thus, understanding the composition and function of the diabetic gut is essential for developing microbiome-based therapeutic strategies.
The Circadian Rhythm of the Microbiome: More Than a Day-Night Cycle
While the circadian rhythm is often discussed in the context of sleep-wake cycles and hormonal regulation, it also governs microbial activity within the gastrointestinal tract. The gut microbiota undergoes dynamic fluctuations throughout the day, influenced by feeding patterns, sleep schedules, and hormonal secretions. These diurnal oscillations are not arbitrary but serve a biological function, synchronizing microbial activity with host metabolism. Within this context, the concept of “nocturnal bacteria” has garnered scientific attention, referring to bacterial populations that become more active or predominant during nighttime hours.
In healthy individuals, these fluctuations are balanced and support metabolic homeostasis. However, in those with diabetes or disrupted circadian rhythms, this microbial rhythmicity becomes distorted. Such disturbances can alter microbial composition and function, contributing to metabolic dysregulation. The term “nocturnal bacteria diabetes” encapsulates this phenomenon, pointing to the role of nighttime-active bacteria in exacerbating or potentially mediating diabetic symptoms. As such, the microbiome’s circadian rhythm is not merely a background process but an integral component of metabolic regulation.
Prevotella and Diabetes: A Double-Edged Sword?
Among the many bacterial genera implicated in metabolic health, Prevotella stands out for its complex and sometimes contradictory role. Some studies have associated Prevotella with beneficial outcomes, including improved glucose metabolism and increased SCFA production, particularly in individuals consuming high-fiber diets. However, other research indicates that certain Prevotella strains may exacerbate inflammatory responses, contributing to insulin resistance and metabolic syndrome.
This dual nature makes Prevotella a focal point in the study of diabetes and gut microbiota. In the context of nocturnal bacterium diabetes, researchers are exploring how specific strains of Prevotella behave during the night and how these behaviors correlate with glucose homeostasis. Initial findings suggest that nighttime Prevotella activity may be significantly different from its daytime profile, potentially contributing to nocturnal hyperglycemia in diabetic patients. Moreover, Prevotella’s ability to degrade complex polysaccharides and interact with mucosal immune cells places it at the intersection of diet, immunity, and metabolism.
Understanding the conditions under which Prevotella exerts either beneficial or harmful effects is crucial for leveraging its potential in microbiome-targeted therapies. This nuanced view of Prevotella and diabetes underscores the importance of precision medicine in microbiome research—a one-size-fits-all approach is unlikely to yield sustainable results.
Metabolic Implications of Nighttime Microbiome Activity
The nocturnal activity of gut microbes has far-reaching implications for metabolic health. During the night, the body’s physiological priorities shift toward rest, repair, and fasting-related metabolic processes. The gut microbiome adapts accordingly, with certain bacterial populations becoming more active in fermenting undigested polysaccharides and producing metabolites that influence host physiology. In the context of diabetes, however, this delicate balance is often disrupted.
Individuals with poorly controlled blood glucose levels often experience altered sleep patterns, which in turn affect gut microbial rhythms. Studies on nocturnal bacteria and diabetes have revealed that irregular sleeping schedules and late-night eating can desynchronize microbial activity, exacerbating insulin resistance and impairing glucose tolerance. Additionally, specific nocturnal bacteria have been found to modulate levels of hormones such as ghrelin and leptin, which are intimately involved in appetite regulation and energy balance.
The production of metabolites such as lipopolysaccharides (LPS) by certain nocturnal bacteria also contributes to systemic inflammation, a hallmark of type 2 diabetes. These insights highlight the importance of aligning lifestyle factors like meal timing and sleep hygiene with the natural rhythms of the microbiome to promote metabolic health.
The Role of Diet in Shaping Nocturnal Microbial Profiles
Diet is one of the most powerful modulators of the gut microbiome, capable of altering microbial composition within days. The timing, composition, and quality of food intake significantly influence which bacteria thrive, particularly during nighttime fasting and digestion. In the case of nocturnal bacterium diabetes, researchers have begun to investigate how specific dietary interventions can reshape nocturnal microbial activity to improve metabolic outcomes.
Diets high in fiber, polyphenols, and prebiotics have been shown to enhance the abundance of beneficial bacteria, including certain strains of Prevotella that are active at night. Conversely, high-fat, low-fiber diets tend to favor the proliferation of pro-inflammatory nocturnal bacteria that may worsen insulin resistance. Time-restricted feeding (TRF), a dietary pattern that confines food intake to specific windows of the day, has also emerged as a promising intervention. TRF appears to restore microbial rhythmicity and improve glycemic control, supporting the hypothesis that synchronizing food intake with circadian rhythms can mitigate the adverse effects of a diabetic gut.
Furthermore, personalized nutrition strategies that consider an individual’s existing microbial profile, metabolic status, and lifestyle habits may offer more effective solutions than generalized dietary advice. Such approaches emphasize the need for microbiome-informed dietary planning, particularly in managing diabetes.
Sleep, Stress, and the Gut-Brain-Microbiome Axis
The intricate relationship between the gut and brain is well-documented, with the gut-brain axis playing a pivotal role in regulating mood, cognition, and overall health. This bidirectional communication network also involves the microbiome, forming what is now known as the gut-brain-microbiome axis. Disruptions in sleep and elevated stress levels—both common in individuals with diabetes—can significantly impact this axis, with consequences for nocturnal microbial activity.
Poor sleep quality alters the release of hormones such as cortisol and melatonin, which in turn affect gut motility and microbial composition. Elevated stress levels can lead to increased intestinal permeability, commonly referred to as “leaky gut,” allowing bacterial metabolites like LPS to enter the bloodstream and trigger systemic inflammation. These changes are particularly relevant in the context of nocturnal bacteria diabetes, as they may amplify the pro-inflammatory potential of nighttime microbial activity.
Moreover, the psychological burden of managing a chronic condition like diabetes can create a feedback loop in which stress worsens glycemic control, further disrupting sleep and gut health. Addressing these interconnected factors requires a holistic approach that incorporates stress management, sleep hygiene, and targeted microbiome support.
Clinical Applications and Future Therapeutic Directions
The insights gained from studying nocturnal microbiome activity are beginning to translate into clinical practice. Probiotic and prebiotic formulations tailored to support beneficial nocturnal bacteria are currently under investigation, with early trials showing promise in improving insulin sensitivity and reducing inflammation. Similarly, microbiome transplants and synbiotics—combinations of prebiotics and probiotics—are being explored as potential interventions for the diabetic gut.
Another exciting avenue of research is the development of chronobiotic therapies—treatments that align with the body’s natural biological rhythms. By timing medication or nutritional interventions to coincide with microbial activity peaks, clinicians may be able to enhance therapeutic efficacy and minimize side effects. This approach aligns with the broader trend toward personalized and precision medicine, in which treatments are customized based on an individual’s unique physiological and microbial profile.
While much work remains to be done, the potential to harness nocturnal microbial activity for therapeutic benefit represents a frontier in diabetes care. Future research will likely focus on identifying key microbial signatures associated with metabolic resilience and susceptibility, enabling early intervention and improved disease management.

Frequently Asked Questions: Nocturnal Bacteria, Diabetes, and the Gut Microbiome
1. How does nighttime activity of gut bacteria differ between healthy individuals and those with diabetes?
In healthy individuals, the circadian rhythm of gut bacteria follows predictable, beneficial patterns that support digestion, metabolism, and immune regulation. These fluctuations help maintain glycemic balance overnight by producing anti-inflammatory metabolites and supporting hormonal signaling. In contrast, people with diabetes often show disrupted microbial rhythms. This disruption can lead to a rise in nocturnal bacteria that drive low-grade inflammation or impair insulin sensitivity. Studies exploring the connection between nocturnal bacteria and diabetes suggest that these nighttime microbial shifts may not just mirror the disease but actively contribute to its metabolic consequences.
2. Why is Prevotella gaining attention in research on nocturnal bacterium diabetes?
Prevotella is a genus that demonstrates versatile metabolic functions, including the breakdown of complex carbohydrates. In the context of nocturnal bacterium diabetes, Prevotella species have shown activity peaks during the night, particularly in response to late-evening food intake or disrupted sleep patterns. While some strains may support metabolic health in fiber-rich diets, others are linked to mucosal inflammation, especially in individuals with dysregulated glucose metabolism. This dual nature makes Prevotella a central player in understanding how the diabetic gut behaves at night. Ongoing research into Prevotella and diabetes seeks to differentiate beneficial from harmful strains to guide more targeted interventions.
3. Can behavioral changes like sleep improvement reduce the impact of nocturnal bacteria on diabetes progression?
Yes, improving sleep hygiene can positively influence gut microbial rhythms, potentially offsetting the adverse metabolic effects of nocturnal bacteria in diabetes. Irregular sleep reduces melatonin and increases cortisol, which in turn affects microbial composition and activity. Aligning sleep and wake times with the body’s natural clock can help stabilize microbial oscillations, allowing beneficial bacteria to flourish during the night. This intervention is particularly relevant in managing nocturnal bacterium diabetes, where disrupted circadian cycles exacerbate inflammation and glucose intolerance. Behavioral consistency acts as a non-pharmaceutical tool to improve gut and metabolic health synergistically.
4. Are there specific diets that can shift nocturnal bacteria toward a more beneficial profile in people with diabetes?
Dietary interventions, especially those rich in fiber and polyphenols, are powerful tools in reshaping the microbiome toward a healthier state. Foods like legumes, oats, and leafy greens nourish bacteria that help counteract the pro-inflammatory environment of the diabetic gut. When consumed in the right timing—avoiding heavy late-night meals—these diets can suppress pathogenic nocturnal bacteria while promoting protective strains. Research into nocturnal bacteria diabetes highlights how evening food choices can influence overnight microbial activity. A Mediterranean-style or plant-based diet aligned with time-restricted feeding protocols has shown particular promise in clinical trials.
5. Could the diabetic gut’s microbial response to nighttime fasting inform future therapies?
Absolutely. Overnight fasting triggers a shift in microbial metabolism, and in the diabetic gut, this response may be muted or abnormal. Normally, fasting prompts nocturnal bacteria to produce beneficial compounds like short-chain fatty acids, but in diabetes, these outputs may be impaired. Therapeutic strategies could involve enhancing these fasting-induced microbial pathways through targeted prebiotics or engineered probiotics. As research deepens into nocturnal bacterium diabetes, fasting-mimicking interventions may provide a drug-free route to metabolic stability. These strategies could be especially impactful when integrated with personalized microbiome assessments.
6. What role does mental health play in regulating nocturnal microbiome activity in people with diabetes?
Psychological stress can significantly alter the composition and behavior of the gut microbiome, particularly during nighttime hours. Individuals with diabetes who also suffer from anxiety or depression often exhibit more pronounced dysbiosis in their nocturnal bacterial populations. Stress hormones can disrupt intestinal permeability and promote the expansion of bacteria that trigger inflammatory responses. The diabetic gut is uniquely sensitive to these psychological and microbial interactions, which may explain why mental health comorbidities often worsen glycemic control. Incorporating stress-reduction techniques into diabetes management may help regulate both the gut microbiome and nighttime metabolic function.
7. How might future wearables or digital health tools help monitor nocturnal bacteria in diabetes?
Emerging technologies like gut microbiome sensors and continuous glucose monitors could be synchronized to detect microbial activity patterns overnight. With machine learning algorithms, it may become possible to identify real-time shifts in the diabetic gut related to nocturnal bacterium diabetes. This could lead to just-in-time interventions such as dietary adjustments or probiotic supplementation tailored to a person’s microbial profile. In the near future, digital tools could bridge the gap between microbiome science and everyday diabetes care. These innovations represent a promising frontier in personalized health monitoring.
8. Can changes in gut bacteria during travel or shift work worsen nocturnal bacterium diabetes?
Yes, frequent travel or irregular work hours can seriously disrupt the circadian rhythm of gut microbes. People with diabetes who experience constant jet lag or nighttime work shifts are especially vulnerable to microbial imbalances that occur during the night. These environmental stressors can encourage the proliferation of pathogenic nocturnal bacteria while suppressing beneficial strains. Such changes may exacerbate insulin resistance and further destabilize blood glucose levels. Understanding how lifestyle-induced dysregulation impacts the diabetic gut could inform targeted solutions for high-risk populations.
9. Are children with type 2 diabetes affected by nocturnal bacteria in similar ways as adults?
Preliminary studies suggest that children with type 2 diabetes also exhibit distinctive nocturnal microbial signatures, though their gut microbiota is still developing and may respond differently to interventions. The diabetic gut in children often shows less microbial diversity, making it more sensitive to dietary and environmental changes. Researchers are beginning to explore how early exposure to artificial light, irregular sleep, and ultra-processed foods might shape nocturnal bacterium diabetes in pediatric populations. Childhood presents a critical window for microbiome modulation, offering a chance to prevent long-term metabolic complications. With age-specific strategies, it may be possible to mitigate the impact of nighttime dysbiosis early on.
10. How close are we to developing microbial therapies that specifically target nocturnal bacteria in diabetes?
Though still in early stages, research into microbial therapies tailored to circadian timing is advancing rapidly. Scientists are now identifying bacterial strains that show peak activity during night hours and evaluating their role in diabetes progression. Some biotech firms are exploring how encapsulated probiotics could release selectively during nighttime digestion. These efforts aim to directly address the challenges posed by nocturnal bacteria diabetes, focusing on timing as well as bacterial strain specificity. If successful, these therapies could redefine how we approach microbiome-based interventions for metabolic diseases.
Conclusion: Rethinking Diabetes Through the Lens of the Nocturnal Microbiome
The growing body of research on nocturnal bacteria and diabetes challenges traditional views of metabolic disease as a solely hormone-driven condition. Instead, it positions the gut microbiome—and more specifically, its nighttime behavior—as a dynamic participant in the regulation of glucose metabolism, inflammation, and overall metabolic health. The emerging evidence surrounding Prevotella and diabetes underscores the complexity of microbial interactions, particularly within the context of a diabetic gut.
As we continue to unravel the layers of this microbial-metabolic interface, new avenues for diagnosis, prevention, and treatment are beginning to emerge. By aligning lifestyle interventions with microbial circadian rhythms, and by developing targeted therapies that consider the nocturnal behavior of key bacterial strains, we can move closer to a more nuanced and effective model of diabetes care. The integration of diet, sleep, stress management, and microbial science offers a holistic framework for addressing this complex condition. Ultimately, embracing the insights offered by nocturnal microbiome activity holds the potential to transform not only how we treat diabetes but how we understand the fundamental biology of metabolic health.
gut microbiome and diabetes, circadian rhythm and metabolism, insulin resistance and gut health, microbial inflammation in diabetes, SCFA-producing bacteria, gut-brain axis in metabolic health, sleep and glucose regulation, diet and microbiome balance, microbial diversity and disease, time-restricted eating and gut health, prebiotics for metabolic health, probiotics and insulin sensitivity, microbial chronotherapy, gut dysbiosis and chronic disease, fiber-rich diets and gut bacteria, inflammation and metabolic disorders, blood sugar and gut health, personalized microbiome therapy, gut barrier function and diabetes, lifestyle and metabolic syndrome prevention
Further Reading:
Changes to Gut Microbiome May Increase Type 2 Diabetes Risk
Arrhythmic Gut Microbiome Signatures Predict Risk of Type 2 Diabetes
Certain gut bacteria, viruses may increase type 2 diabetes risk, study finds
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


