Understanding Coronary Artery Calcifications
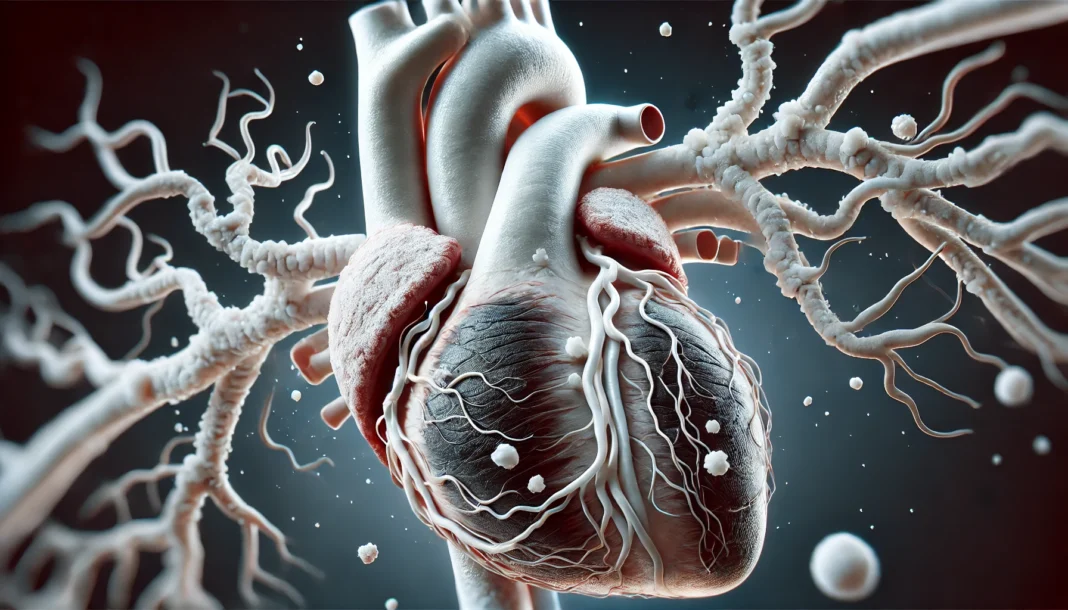
Coronary artery calcifications (CAC) represent a major health concern due to their strong correlation with cardiovascular disease, the leading cause of mortality worldwide. These calcifications, which involve the deposition of calcium in the arterial walls, are a significant marker of atherosclerosis, a condition characterized by the buildup of plaques that can restrict blood flow and lead to severe cardiovascular events such as heart attacks and strokes. CAC is often detected incidentally through imaging techniques, particularly computed tomography (CT) scans, which provide crucial insights into an individual’s cardiovascular risk profile.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
The development of CAC is a complex process influenced by various factors, including genetics, lifestyle choices, metabolic disorders, and chronic inflammation. While some degree of arterial calcification is expected with aging, excessive or premature calcification significantly increases the likelihood of adverse cardiovascular events. Importantly, CAC is not merely a passive consequence of aging but an active pathological process driven by molecular and cellular mechanisms that promote vascular stiffening and impaired arterial function. Understanding the causes, clinical implications, and available treatment options for CAC is essential for optimizing cardiovascular health and preventing severe complications.
What Causes Calcification of Arteries?
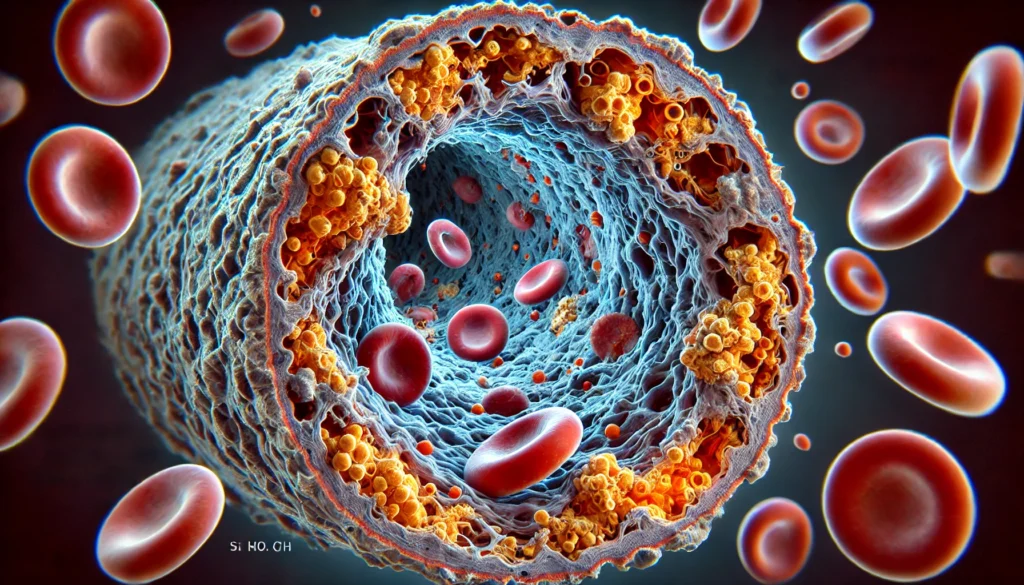
The process of arterial calcification is multifactorial, involving both modifiable and non-modifiable risk factors. One of the primary drivers of CAC is chronic inflammation, which triggers vascular damage and promotes the deposition of calcium within atherosclerotic plaques. Inflammatory markers such as C-reactive protein (CRP) and interleukin-6 have been closely associated with the progression of calcified coronary atherosclerosis.
Metabolic conditions such as diabetes mellitus and chronic kidney disease also contribute significantly to arterial calcification. Hyperglycemia in diabetes leads to endothelial dysfunction, oxidative stress, and increased vascular calcification. Similarly, chronic kidney disease disrupts calcium and phosphate metabolism, leading to vascular calcification through the dysregulation of mineral homeostasis and secondary hyperparathyroidism. These conditions highlight the intricate interplay between metabolic disorders and cardiovascular health.
Additionally, lifestyle factors play a pivotal role in the development of CAC. A diet high in saturated fats, trans fats, and processed foods contributes to the accumulation of arterial plaques, increasing the likelihood of calcification. Smoking further exacerbates the risk by inducing oxidative stress and inflammation, accelerating the progression of atherosclerosis. Conversely, regular physical activity and a diet rich in antioxidants, omega-3 fatty acids, and fiber have been shown to mitigate arterial calcification by improving endothelial function and reducing systemic inflammation.
Genetics also influence an individual’s susceptibility to CAC. A family history of cardiovascular disease often indicates an inherited predisposition to arterial calcification, emphasizing the importance of early screening and preventive measures in high-risk individuals. While genetic factors cannot be modified, lifestyle interventions and medical therapies can significantly reduce the overall burden of cardiovascular risk.
The Significance of Coronary Artery Calcification on CT Scan
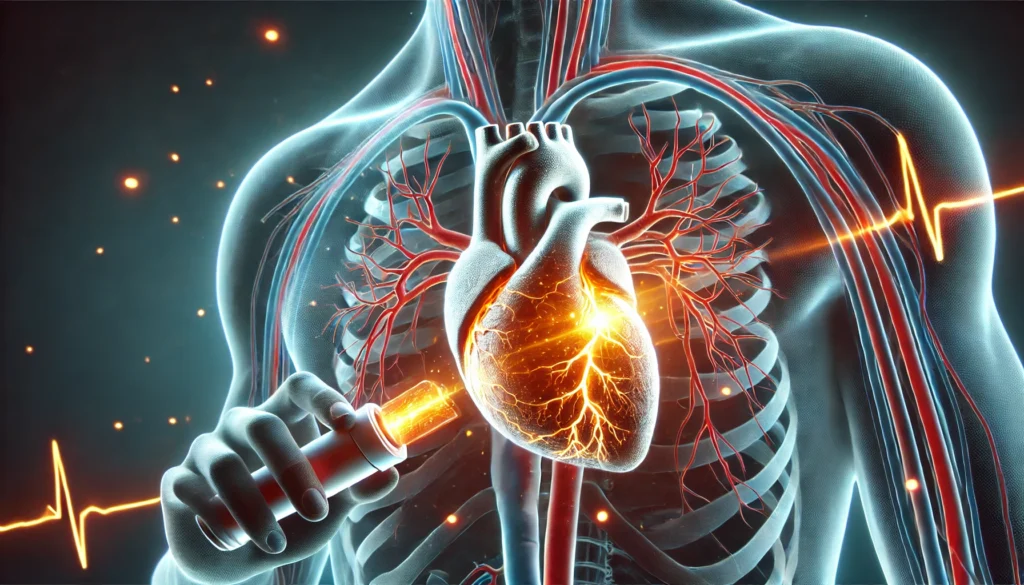
CT imaging has revolutionized the assessment of coronary artery disease by providing a non-invasive and highly accurate method for detecting and quantifying CAC. The coronary artery calcium score (CACS), derived from CT scans, serves as a powerful prognostic tool that helps stratify cardiovascular risk and guide clinical decision-making. This score quantifies the extent of calcification in the coronary arteries, with higher scores correlating with a greater risk of future cardiac events.
Individuals with a CACS of zero have a very low risk of cardiovascular disease, while those with scores exceeding 1000 are at a significantly elevated risk of heart attacks and other cardiovascular complications. The predictive value of CACS extends beyond traditional risk factors such as cholesterol levels and blood pressure, making it an essential component of comprehensive cardiovascular risk assessment.
Moreover, the detection of CAC on CT scans can prompt early interventions, including lifestyle modifications, pharmacologic therapy, and more intensive cardiovascular monitoring. Statin therapy, for instance, is often initiated in individuals with elevated CACS to lower cholesterol levels and stabilize atherosclerotic plaques. Similarly, aspirin therapy may be considered in select patients to reduce thrombotic risk. Importantly, CT imaging also helps identify individuals who may benefit from more aggressive preventive strategies, ensuring that high-risk patients receive timely and appropriate interventions.
Treatment and Management of Severe Coronary Artery Calcification
The management of severe coronary artery calcification requires a multifaceted approach that encompasses lifestyle modifications, pharmacologic interventions, and, in some cases, invasive procedures. Lifestyle changes remain the cornerstone of CAC management, as they address the underlying risk factors contributing to arterial calcification. A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce inflammation and improve lipid profiles. Regular exercise, including aerobic and resistance training, has been shown to enhance vascular health by improving endothelial function and reducing arterial stiffness.
Pharmacologic therapy plays a crucial role in mitigating the progression of CAC. Statins, the most widely prescribed lipid-lowering agents, have demonstrated significant benefits in reducing cardiovascular risk by lowering LDL cholesterol and stabilizing atherosclerotic plaques. In addition to statins, newer lipid-lowering agents such as PCSK9 inhibitors provide an effective alternative for individuals with high cardiovascular risk who do not achieve adequate lipid control with statins alone.
Antihypertensive medications are also essential in managing CAC, as uncontrolled hypertension accelerates arterial damage and calcification. Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) help protect the vascular endothelium and reduce the burden of arterial calcification. In patients with diabetes, optimizing glycemic control through medications such as metformin and SGLT2 inhibitors can further mitigate vascular complications and slow the progression of CAC.
In cases of severe CAC where medical therapy alone is insufficient, interventional procedures may be necessary. Percutaneous coronary intervention (PCI) with specialized techniques such as rotational atherectomy and intravascular lithotripsy can effectively treat heavily calcified lesions and restore blood flow. Coronary artery bypass grafting (CABG) remains a viable option for patients with extensive calcification and multi-vessel disease, offering long-term benefits in terms of symptom relief and survival.
Frequently Asked Questions (FAQ) on Coronary Artery Calcifications
1. What are the early signs of severe coronary artery calcification, and how can they be detected?
Severe coronary artery calcification often develops silently over time, making early detection challenging without proper screening. However, individuals may experience subtle symptoms such as occasional chest discomfort, shortness of breath during exertion, or fatigue that is not easily explained. These signs may indicate that blood flow to the heart is becoming restricted due to calcified coronary atherosclerosis. One of the most effective ways to detect coronary artery calcifications early is through a coronary artery calcium score obtained via a CT scan. The significance of coronary artery calcification on CT scan results lies in its ability to quantify the extent of calcification and predict future cardiovascular risks, allowing for timely intervention.
2. Can lifestyle changes reverse or reduce coronary artery calcifications?
While coronary artery calcifications are generally considered irreversible, certain lifestyle modifications can slow their progression and reduce the risk of further cardiovascular complications. Adopting a heart-healthy diet rich in omega-3 fatty acids, fiber, and antioxidants can help manage cholesterol levels and inflammation, both of which contribute to calcified coronary atherosclerosis. Regular physical activity improves vascular function and reduces arterial stiffness, mitigating the impact of severe coronary artery calcification. Stress management and adequate sleep also play critical roles in maintaining cardiovascular health by reducing chronic inflammation. Although these lifestyle changes may not dissolve existing calcifications, they can significantly improve overall heart function and prevent additional plaque buildup.
3. What medical treatments are available for managing coronary artery calcifications?
Medical management of coronary artery calcifications focuses on stabilizing plaques, reducing cardiovascular risk factors, and improving blood flow to the heart. Statins are commonly prescribed to lower LDL cholesterol levels, which helps slow the progression of calcified coronary atherosclerosis. In cases of severe coronary artery calcification, blood pressure management through ACE inhibitors or beta-blockers can help reduce strain on the heart and prevent further arterial damage. In patients with diabetes, optimizing glucose control is crucial since high blood sugar levels accelerate vascular calcification. Emerging treatments such as PCSK9 inhibitors and anti-inflammatory medications are being explored for their potential to further mitigate arterial calcification. The significance of coronary artery calcification on CT scan findings often guides physicians in determining the intensity of treatment required for each patient.
4. Is there a genetic predisposition to developing coronary artery calcifications?
Yes, genetics play a significant role in determining an individual’s susceptibility to coronary artery calcifications. Family history of cardiovascular disease, high cholesterol, or metabolic disorders such as diabetes increases the likelihood of developing calcified coronary atherosclerosis at an earlier age. Genetic factors influence how the body metabolizes lipids, regulates blood pressure, and responds to inflammation, all of which contribute to arterial calcification. However, having a genetic predisposition does not mean that severe coronary artery calcification is inevitable. Lifestyle interventions, regular cardiovascular screenings, and preventive medications can significantly reduce the risk, even in those with a strong family history of heart disease.
5. How does diabetes contribute to coronary artery calcifications?
Diabetes is a major risk factor for coronary artery calcifications due to its impact on vascular health. Chronic high blood sugar levels lead to endothelial dysfunction, increased oxidative stress, and systemic inflammation, all of which accelerate the calcification process in the arteries. Diabetics often experience abnormal calcium and phosphate metabolism, further promoting the deposition of calcium within atherosclerotic plaques. Over time, these deposits harden, resulting in severe coronary artery calcification that increases the risk of heart attacks and strokes. The significance of coronary artery calcification on CT scan results in diabetic patients is particularly high, as it helps assess cardiovascular risk and guide the intensity of treatment strategies.
6. How do coronary artery calcifications differ from traditional atherosclerosis?
Coronary artery calcifications are a specific manifestation of atherosclerosis in which calcium deposits accumulate within arterial plaques, causing arterial walls to stiffen and reducing their ability to expand and contract. While traditional atherosclerosis involves the buildup of cholesterol, inflammatory cells, and fibrous tissue in the arteries, calcified coronary atherosclerosis signifies a more advanced stage of the disease. The presence of calcium within plaques increases the likelihood of plaque rupture and subsequent clot formation, which can lead to life-threatening cardiovascular events. Detecting coronary artery calcifications through imaging, particularly CT scans, allows for early risk assessment and proactive management. Understanding what causes calcification of arteries is key to distinguishing different forms of arterial disease and tailoring treatment approaches accordingly.
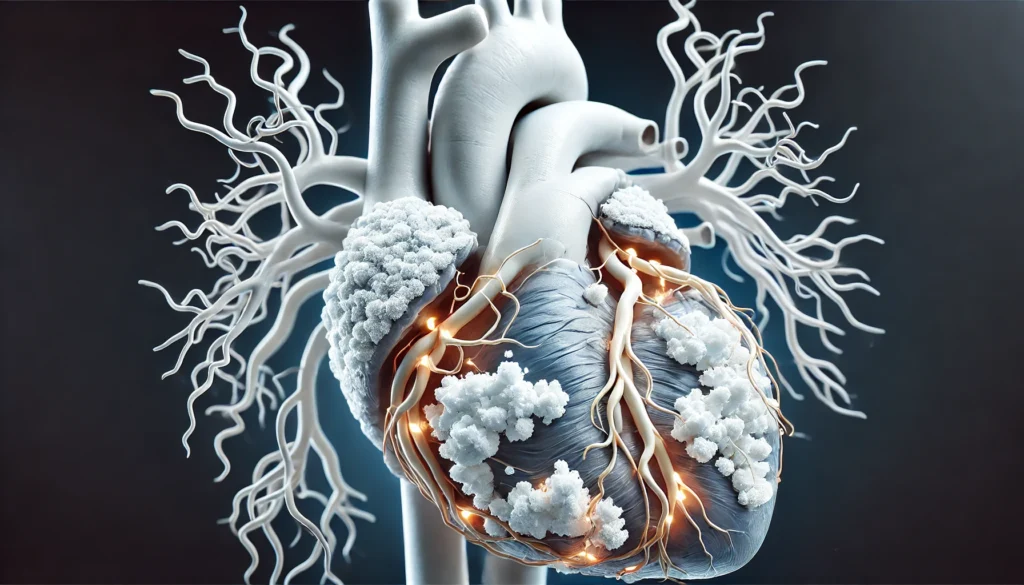
7. Can severe coronary artery calcification lead to heart failure?
Yes, severe coronary artery calcification can contribute to heart failure by restricting blood supply to the heart muscle over time. When calcified plaques narrow or completely obstruct coronary arteries, the heart is forced to work harder to pump blood, leading to increased strain on the cardiac muscle. Over time, this excessive workload can result in left ventricular hypertrophy, reduced cardiac output, and eventual heart failure. Patients with extensive calcified coronary atherosclerosis are at higher risk of developing ischemic heart disease, which significantly impairs heart function. Managing underlying risk factors, optimizing medication regimens, and undergoing timely interventions can help prevent the progression from severe coronary artery calcification to heart failure.
8. Are there non-invasive ways to monitor coronary artery calcifications over time?
Yes, several non-invasive techniques are available to monitor the progression of coronary artery calcifications and assess cardiovascular risk. The most widely used method is the coronary artery calcium score, obtained through a CT scan, which quantifies the extent of calcification and tracks changes over time. Advanced imaging modalities such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT) provide additional insights into plaque composition and arterial stiffness. In addition to imaging, blood tests measuring inflammatory markers like C-reactive protein (CRP) and lipid profiles help gauge the progression of calcified coronary atherosclerosis. Monitoring these indicators regularly allows healthcare providers to adjust treatment strategies and implement preventive measures accordingly.
9. What are the risks of undergoing invasive procedures for treating calcified arteries?
Invasive procedures such as angioplasty and coronary artery bypass grafting (CABG) carry inherent risks, particularly in patients with severe coronary artery calcification. One of the primary concerns is the difficulty of expanding stents in heavily calcified arteries, which can lead to suboptimal outcomes or stent failure. In such cases, specialized techniques such as rotational atherectomy or intravascular lithotripsy may be used to modify calcified plaques before stent placement. Additionally, surgical interventions carry risks of bleeding, infection, and complications related to anesthesia. The decision to undergo an invasive procedure is typically based on the significance of coronary artery calcification on CT scan results, symptom severity, and the overall cardiovascular health of the patient.
10. How can individuals lower their risk of developing coronary artery calcifications?
Reducing the risk of developing coronary artery calcifications requires a proactive approach to cardiovascular health. Maintaining a balanced diet low in processed foods and high in nutrient-rich whole foods can help regulate lipid levels and reduce systemic inflammation. Engaging in regular physical activity, such as aerobic exercise and strength training, improves arterial elasticity and blood flow. Avoiding smoking and managing stress effectively are also critical components of heart disease prevention. Regular health check-ups, including lipid panels and CT scans when indicated, allow for early detection and intervention before severe coronary artery calcification develops. By understanding what causes calcification of arteries and taking preventive measures, individuals can significantly lower their risk of cardiovascular complications.
Conclusion: Proactive Strategies for Cardiovascular Health
Coronary artery calcifications serve as a critical indicator of cardiovascular disease and warrant careful evaluation through advanced imaging techniques such as CT scans. Understanding what causes calcification of arteries enables individuals to adopt preventive measures that reduce their risk of severe coronary artery calcification. Lifestyle modifications, pharmacologic therapy, and, when necessary, interventional procedures play integral roles in managing CAC and improving cardiovascular outcomes.
Given the significance of coronary artery calcification on CT scans in predicting cardiovascular risk, early detection and proactive intervention are essential. Individuals at high risk should undergo regular cardiovascular assessments and work closely with healthcare providers to develop personalized strategies for optimizing heart health. By prioritizing preventive measures and adhering to evidence-based treatments, individuals can significantly reduce their risk of cardiovascular complications and improve their overall well-being.
arterial plaque buildup, cardiovascular disease risk, heart artery calcification, atherosclerosis progression, vascular health management, CT scan heart assessment, heart attack prevention, arterial stiffness treatment, coronary artery disease symptoms, cardiovascular imaging techniques, calcium deposits in arteries, lifestyle changes for heart health, cholesterol and heart disease, inflammation and vascular health, managing heart disease risk, non-invasive heart screening, blood flow restriction in arteries, heart disease prevention strategies, advanced heart diagnostics, coronary artery treatment options
Further Reading:
Coronary Artery Calcification and its Progression: What Does it Really Mean?
Coronary artery calcification in lung cancer screening
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.