Type 1 diabetes is a chronic condition that affects millions worldwide. It has long been understood as a disorder characterized by the body’s inability to produce sufficient insulin, a hormone necessary for regulating blood sugar levels. However, the pathophysiology behind type 1 diabetes is complex and involves an immune system malfunction. While type 1 diabetes is most often associated with insulin deficiency, its roots lie in an autoimmune attack that targets the pancreas. But is diabetes an autoimmune disease? This article explores the connection between type 1 diabetes and the immune system, unraveling how the body’s own defense mechanisms can inadvertently lead to diabetes development.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
Understanding Type 1 Diabetes
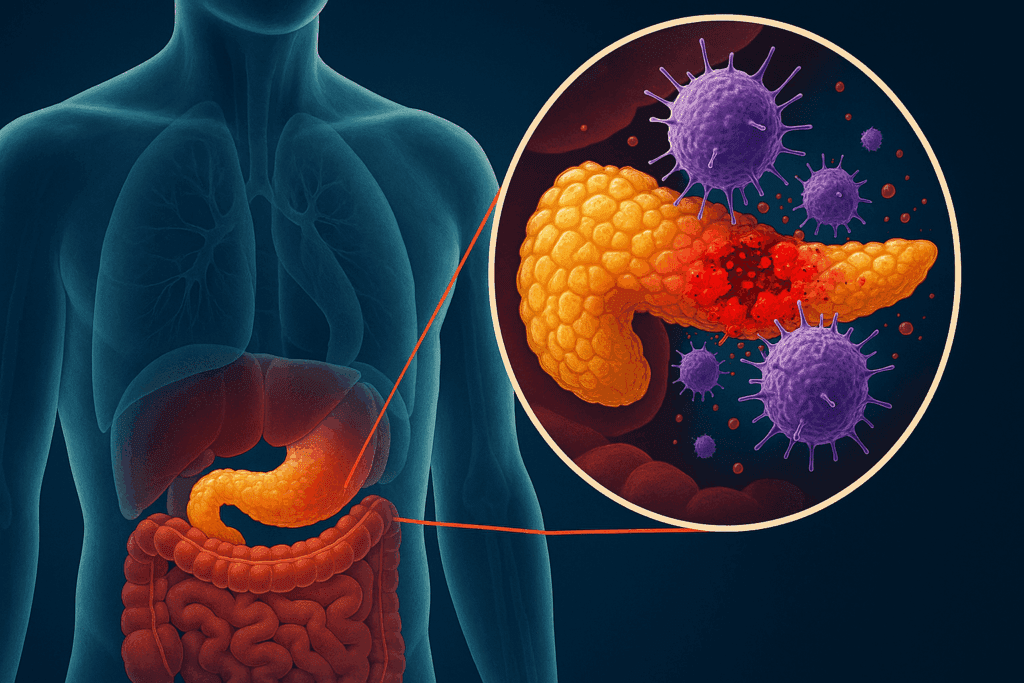
Type 1 diabetes, often diagnosed in childhood or adolescence, occurs when the body’s immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. Unlike type 2 diabetes, where the body becomes resistant to insulin, type 1 diabetes leads to a complete lack of insulin production. Without insulin, glucose cannot enter cells for energy, leading to high blood sugar levels that, over time, can cause serious health problems.
While the exact cause of this autoimmune response is not fully understood, it is widely accepted that both genetic and environmental factors play a significant role. The immune system’s inability to distinguish between normal cells and foreign invaders leads to the destruction of the body’s own tissues—specifically, the insulin-producing beta cells in the pancreas.
Is Type 1 Diabetes an Autoimmune Disease?
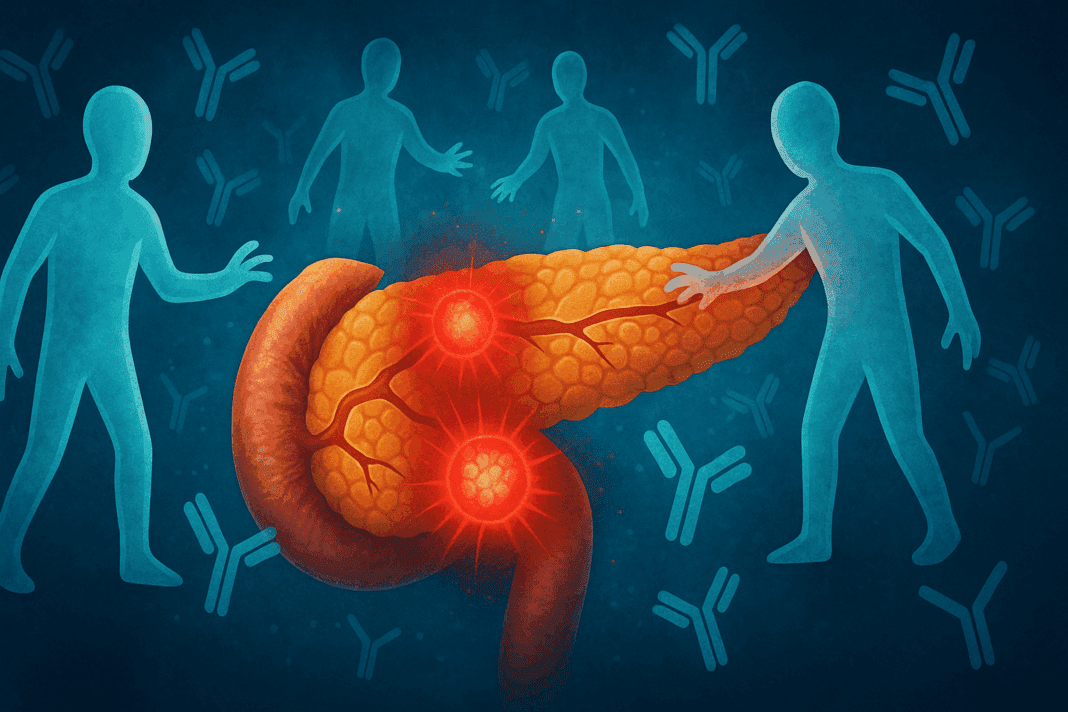
The term “autoimmune” refers to diseases where the immune system attacks the body’s own healthy cells and tissues. In the case of type 1 diabetes, the immune system targets and destroys the insulin-producing beta cells in the pancreas. This autoimmune response impairs the body’s ability to produce insulin, which is critical for regulating blood sugar levels.
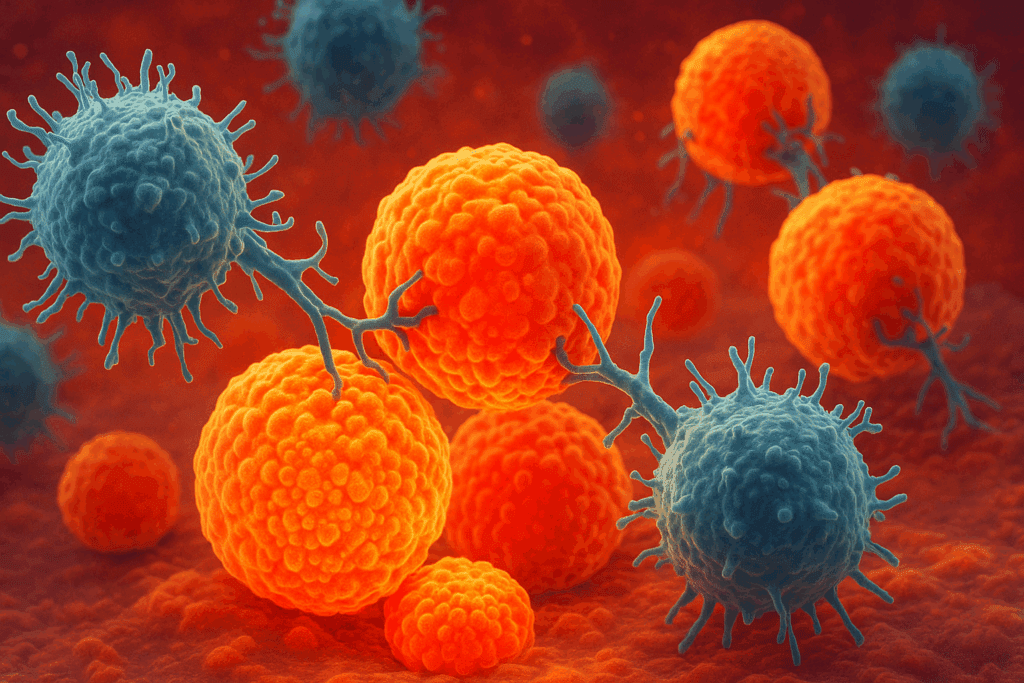
Research consistently supports the classification of type 1 diabetes as an autoimmune disease. Studies have shown that the immune system’s T-cells, which are typically responsible for defending the body against pathogens, mistakenly target and attack the beta cells in the pancreas. This autoimmune reaction leads to beta cell destruction, and consequently, insulin production is severely reduced or halted entirely. As a result, individuals with type 1 diabetes require lifelong insulin therapy to manage their blood sugar levels.
The connection between autoimmune diabetes and type 1 diabetes has been confirmed through various studies, including those involving individuals with other autoimmune disorders. Research shows that people with a family history of autoimmune diseases, such as autoimmune thyroid disease or celiac disease, are more likely to develop type 1 diabetes. This suggests that there may be a shared autoimmune predisposition among different conditions.
The Role of Genetics in Autoimmune Diabetes
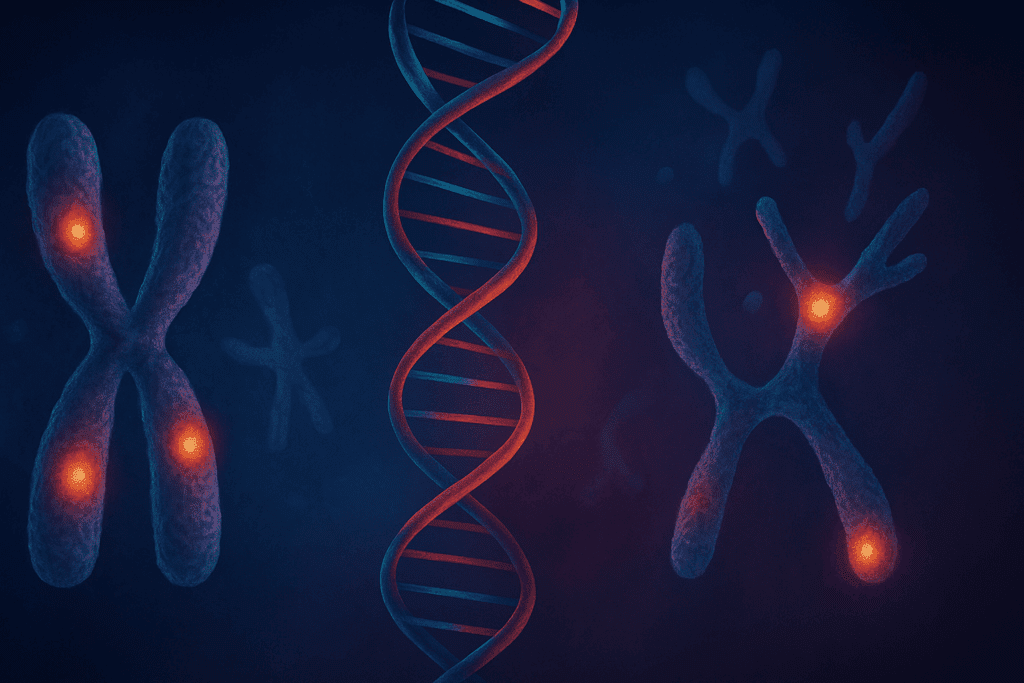
Genetics plays a crucial role in the development of autoimmune diseases, and type 1 diabetes is no exception. While the exact genetic triggers remain unclear, certain genes, particularly those related to the immune system, are known to increase the risk of developing type 1 diabetes. The most well-known genetic risk factors are located within the major histocompatibility complex (MHC) region on chromosome 6, which is involved in immune function.
One of the key genes associated with type 1 diabetes is the HLA (human leukocyte antigen) gene. The HLA gene plays a significant role in immune system regulation, and variations in this gene are linked to an increased risk of developing autoimmune diseases, including type 1 diabetes. However, having these genetic markers does not guarantee that an individual will develop the condition, suggesting that environmental factors, such as viral infections or other triggers, also play a significant role in the disease’s onset.
Autoimmune Diabetes Symptoms
The symptoms of autoimmune diabetes, also known as type 1 diabetes, develop gradually and can be life-threatening if not addressed. Early signs include excessive thirst, frequent urination, extreme hunger, fatigue, and unexplained weight loss. As the disease progresses, individuals may experience blurred vision, slow wound healing, and increased susceptibility to infections. These symptoms occur because the body cannot use glucose for energy, leading to high blood sugar levels.
In addition to the common symptoms of type 1 diabetes, people with autoimmune diabetes may also experience other autoimmune-related symptoms. For example, individuals with type 1 diabetes often have a higher incidence of other autoimmune disorders, such as autoimmune thyroid disease and celiac disease. These conditions share similar immune system dysfunctions, suggesting a common autoimmune mechanism that underlies multiple diseases.
The Immune System’s Role in Type 1 Diabetes
At the heart of autoimmune diabetes is the immune system’s mistaken attack on the beta cells in the pancreas. T-cells, which are responsible for attacking foreign pathogens, begin to destroy the insulin-producing beta cells as though they were invaders. This destruction leads to a lack of insulin production, which in turn leads to high blood sugar levels.
Research has shown that type 1 diabetes is triggered by a combination of genetic susceptibility and environmental factors. For example, viral infections, such as enteroviruses, have been linked to an increased risk of developing type 1 diabetes in genetically predisposed individuals. The immune system’s response to these infections may inadvertently trigger the autoimmune process that leads to beta cell destruction.
The Autoimmune Process and Beta Cell Destruction
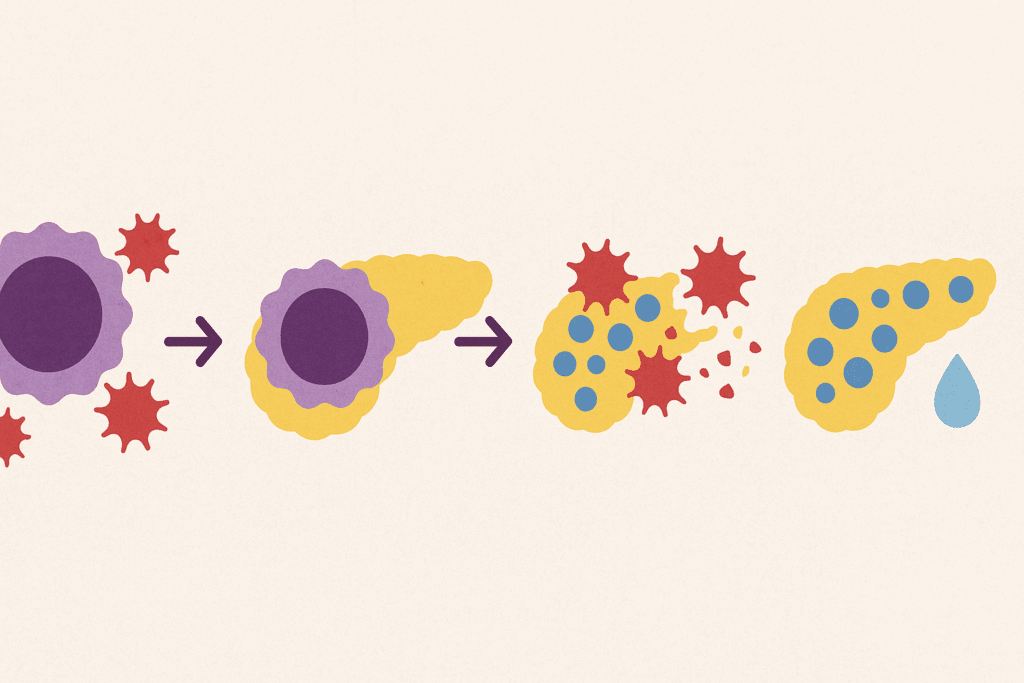
The autoimmune process that leads to type 1 diabetes begins when the body’s immune system recognizes the beta cells in the pancreas as foreign. This recognition occurs through the activation of antigen-presenting cells, which display fragments of the beta cell proteins to T-cells. The T-cells then launch an immune response, attacking the beta cells in an attempt to eliminate them. Over time, this continuous attack leads to the gradual destruction of the beta cells, resulting in the inability of the pancreas to produce insulin.
Interestingly, the autoimmune response in type 1 diabetes is not the same for everyone. Some individuals may experience a rapid destruction of beta cells, while others may retain some beta cell function for years. This variability in disease progression is one reason why the onset and severity of type 1 diabetes can vary widely among individuals.
Is Diabetes Mellitus an Autoimmune Disease?
Diabetes mellitus is a general term for a group of conditions that affect how the body uses blood sugar (glucose). Type 1 diabetes, which is an autoimmune condition, is one type of diabetes mellitus. However, diabetes mellitus also includes type 2 diabetes, a metabolic disorder that is not autoimmune in nature. In type 2 diabetes, the body becomes resistant to insulin, rather than attacking the insulin-producing cells.
It is important to distinguish between the different types of diabetes when discussing autoimmune responses. While type 1 diabetes is an autoimmune disease, type 2 diabetes is primarily related to lifestyle factors such as obesity, physical inactivity, and poor diet. Thus, not all forms of diabetes are autoimmune diseases, but type 1 diabetes is undoubtedly classified as one.
Late Onset Diabetes and Its Autoimmune Connection
While type 1 diabetes is typically diagnosed in childhood or adolescence, there is a growing recognition of “late-onset” type 1 diabetes. This form of diabetes is diagnosed in adults, often after the age of 30. The autoimmune mechanisms that cause beta cell destruction in these cases are similar to those seen in early-onset type 1 diabetes. However, the progression of the disease is often slower, and the initial symptoms may be less obvious.
Late onset diabetes may be challenging to diagnose because it shares many characteristics with type 2 diabetes, such as the development of insulin resistance. However, the underlying autoimmune process in late onset type 1 diabetes is the same, and it often requires specialized tests, such as the measurement of autoantibodies, to confirm the diagnosis.
Diabetes 1 Autoimmune Disease: Implications for Treatment
Understanding that type 1 diabetes is an autoimmune disease has important implications for treatment. Traditionally, type 1 diabetes has been managed with insulin therapy to regulate blood sugar levels. However, researchers are now exploring ways to modulate the immune system to prevent or reverse the autoimmune attack on beta cells.
One promising area of research involves the use of immunotherapies that target the immune system’s response to beta cells. By blocking the T-cells responsible for attacking the pancreas, scientists hope to preserve beta cell function and potentially reduce the need for insulin therapy. Although these treatments are still in the experimental stage, they hold promise for the future of type 1 diabetes management.
Frequently Asked Questions (FAQ) about Type 1 Diabetes and Its Autoimmune Connection
What is autoimmune diabetes, and how does it differ from other types of diabetes?
Autoimmune diabetes, often referred to as type 1 diabetes, is a chronic condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This differs from type 2 diabetes, which involves insulin resistance rather than autoimmune destruction. The main distinction lies in the cause: while type 1 diabetes is driven by an autoimmune response, type 2 diabetes is largely influenced by lifestyle factors, such as diet and physical activity. Understanding the autoimmune nature of type 1 diabetes helps in developing targeted treatments that aim to manage or even prevent the immune system’s attack on the pancreas. Autoimmune diabetes symptoms can include extreme thirst, frequent urination, fatigue, and unexplained weight loss, which occur due to the body’s inability to properly regulate blood sugar levels.
Is type 1 diabetes an autoimmune disease?
Yes, type 1 diabetes is considered an autoimmune disease. This condition occurs when the body’s immune system wrongly identifies the insulin-producing beta cells in the pancreas as foreign invaders and attacks them. As a result, the pancreas produces little to no insulin, leading to high blood sugar levels. This is fundamentally different from type 2 diabetes, where the body becomes resistant to insulin, rather than attacking the insulin-producing cells. Therefore, when people ask, “Is type 1 diabetes an autoimmune disease?”, the answer is definitively yes. The autoimmune nature of this disease underscores the need for treatments that address the immune system’s malfunction.
What causes the immune system to attack the pancreas in type 1 diabetes?
The exact cause of the immune system’s attack on the pancreas in type 1 diabetes is not fully understood, but both genetic and environmental factors play a role. Certain genes, particularly those involved in immune function, increase susceptibility to the disease. Additionally, viral infections, like enteroviruses, have been suggested as potential triggers that kickstart the autoimmune response. The immune system’s T-cells, which typically protect the body from infections, mistakenly target and destroy the beta cells in the pancreas, leading to insulin deficiency. The cause of the immune system malfunction is still a subject of ongoing research, but it is clear that both genetic predisposition and environmental triggers contribute to the development of this autoimmune diabetes.
Can autoimmune diabetes be prevented or reversed?
Currently, there is no known cure for autoimmune diabetes, but researchers are exploring various strategies to prevent the immune system from attacking the pancreas. One promising area of research focuses on immune-modulating treatments, which aim to stop or slow the immune system’s attack on the insulin-producing beta cells. While insulin therapy remains the standard treatment, scientists are investigating vaccines, immune system therapies, and even gene therapies that could potentially stop or reverse the disease in the future. However, it’s important to note that these treatments are still experimental and not yet available for widespread use. Prevention of autoimmune diabetes remains a major research goal, particularly in individuals at high genetic risk for developing the condition.
What are the key symptoms of autoimmune diabetes?
The symptoms of autoimmune diabetes, or type 1 diabetes, can develop rapidly and include extreme thirst, frequent urination, unexplained weight loss, and fatigue. These symptoms occur because the body cannot utilize glucose for energy due to the lack of insulin. Additionally, individuals may experience blurred vision, slow-healing wounds, and frequent infections. People with autoimmune diabetes often face other autoimmune conditions as well, such as autoimmune thyroid disease or celiac disease, as there is a shared genetic predisposition to autoimmune responses. Early detection of these symptoms is critical for effective management of the disease and to prevent complications such as diabetic ketoacidosis, a potentially life-threatening condition.
Is late onset diabetes an autoimmune disease?
Late onset diabetes, also known as Latent Autoimmune Diabetes in Adults (LADA), shares similarities with type 1 diabetes, as it involves autoimmune destruction of insulin-producing cells. However, LADA typically presents in adulthood, often after the age of 30, and progresses more slowly than type 1 diabetes. While LADA shares the autoimmune characteristic of type 1 diabetes, it may initially be misdiagnosed as type 2 diabetes because it often presents with insulin resistance. Over time, individuals with LADA may require insulin therapy as the autoimmune response continues to destroy beta cells. This form of autoimmune diabetes highlights the complexity of diagnosing and managing autoimmune diabetes in adults, particularly as it may resemble more common conditions like type 2 diabetes.
How is type 1 diabetes autoimmune different from type 2 diabetes?
The key difference between type 1 and type 2 diabetes lies in the underlying cause. Type 1 diabetes is an autoimmune disease, where the immune system attacks and destroys the insulin-producing cells in the pancreas, leading to insulin deficiency. On the other hand, type 2 diabetes occurs when the body becomes resistant to insulin or when the pancreas does not produce enough insulin to maintain normal blood sugar levels. While type 1 diabetes typically manifests in childhood or adolescence, type 2 diabetes is more common in adults and is often linked to lifestyle factors like obesity, poor diet, and lack of physical activity. Treatment for type 1 diabetes focuses on insulin replacement, whereas type 2 diabetes can often be managed with lifestyle changes and medications to improve insulin sensitivity.
What is the role of the immune system in the development of type 1 diabetes?
In type 1 diabetes, the immune system mistakenly targets and destroys the insulin-producing beta cells in the pancreas. Normally, the immune system protects the body from harmful invaders, such as bacteria and viruses, by identifying and attacking foreign cells. However, in autoimmune diabetes, the immune system fails to recognize the beta cells as part of the body and attacks them as if they were harmful pathogens. This leads to a significant reduction in insulin production, which is critical for regulating blood sugar levels. As the immune system continues its attack, the pancreas becomes unable to produce enough insulin, resulting in high blood sugar levels and the need for lifelong insulin therapy.
Are there genetic factors that contribute to autoimmune diabetes?
Yes, genetics play a significant role in the development of autoimmune diabetes. Certain genes related to the immune system, particularly those in the major histocompatibility complex (MHC) region, are associated with an increased risk of type 1 diabetes. Individuals with a family history of autoimmune diseases, such as autoimmune thyroid disease or celiac disease, have a higher likelihood of developing autoimmune diabetes. However, not everyone with these genetic risk factors will develop the disease, indicating that environmental factors, such as viral infections, also contribute to the onset of autoimmune diabetes. Understanding the genetic predisposition to autoimmune diabetes helps researchers identify high-risk individuals and develop preventive strategies.
Can autoimmune diabetes be diagnosed in adults, and how is it different from type 2 diabetes?
Yes, autoimmune diabetes can be diagnosed in adults, and it is often referred to as Latent Autoimmune Diabetes in Adults (LADA). LADA is similar to type 1 diabetes in that it involves the autoimmune destruction of beta cells in the pancreas. However, LADA progresses more slowly and often resembles type 2 diabetes in its early stages, particularly because adults with LADA may still produce some insulin at the beginning. As the disease progresses, the need for insulin therapy increases, just as it does in type 1 diabetes. The main distinction between LADA and type 2 diabetes is the autoimmune nature of the disease, which is identified through tests for autoantibodies and C-peptide levels, which are not typically present in type 2 diabetes. Early and accurate diagnosis is crucial for effective treatment and management.
Conclusion: The Future of Type 1 Diabetes Research
In conclusion, type 1 diabetes is an autoimmune disease characterized by the immune system’s attack on the insulin-producing beta cells in the pancreas. This autoimmune response leads to insulin deficiency and high blood sugar levels, which can result in a range of serious health complications. While the exact cause of this immune response is still not fully understood, genetics and environmental factors both play significant roles in the development of the disease.
The ongoing research into autoimmune diabetes continues to shed light on the complex interplay between the immune system, genetics, and environmental factors in the development of type 1 diabetes. As scientists uncover new insights into the autoimmune processes that drive this disease, the hope is that future treatments will not only focus on insulin replacement but also on immune system modulation, offering new avenues for managing and even reversing type 1 diabetes.
By understanding the autoimmune nature of type 1 diabetes, we can better appreciate the complexity of the disease and the need for innovative treatments that go beyond conventional insulin therapy. The future of type 1 diabetes research is promising, and as our knowledge of autoimmune diabetes grows, so too does the potential for improved therapies and, ultimately, a cure.
Further Reading:
Auto-immunity and the gut microbiome in type 1 diabetes: Lessons from rodent and human studies
Type 1 Diabetes: A Chronic Anti-Self-Inflammatory Response
Novel Insights into the Immunotherapy-Based Treatment Strategy for Autoimmune Type 1 Diabetes
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.